A Cutaneous Cılıated Cyst Mımıckıng a Pılonıdal Cyst
Seda Gun1, Duygu Kuru2, Levent Yildiz3
1 Assistant Professor, Department of Pathology, Ondokuz Mays University Medical School, Samsun, Turkey.
2 Resident, Department of Pathology, Ondokuz Mays University Medical School, Samsun, Turkey.
3 Professor, Department of Pathology, Ondokuz Mays University Medical School, Samsun, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Seda Gun, Department of Pathology, Ondokuz Mays University Medical School, Samsun, Turkey.
E-mail: sakifgun@yahoo.com
Cutaneous Ciliated Cyst (CCC) is a benign tumor encountered especially in the upper extremities and the perineal area in young women after puberty. CCC is located in the subcutaneous tissue in deep dermis, and histologically, it is a single, unilocular or multilocular cyst with mullerian origin and is lined with an epithelium similar to that of fallopian tube. In this case report, the histopathological immunohistochemical findings and controversial pathogenesis of a rare CCC case is described.
Ciliated cyst, Oestrogen receptor, Mullerian, PAX8
Case Report
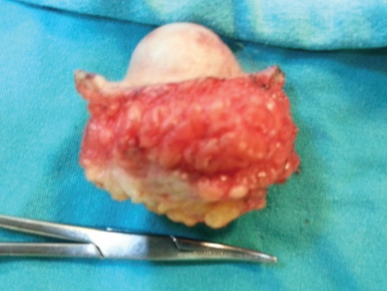
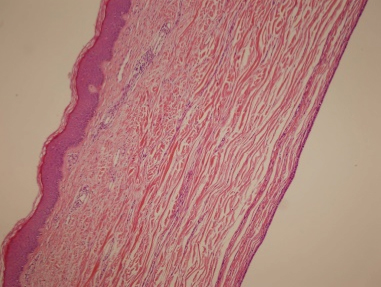
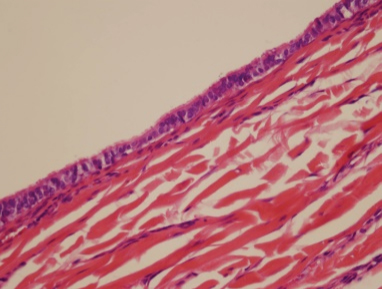
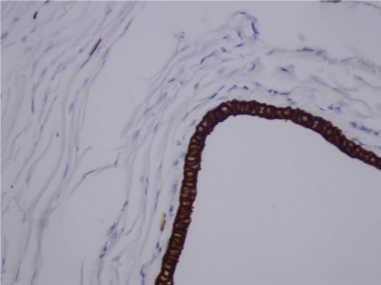
The patient was a 14-year-old female who presented to the hospital with the complaints of swelling and tenderness in the presacral region, lasting for two months. The lesion was previously aspirated in the external centre, but after a while, swelling had occurred again. Her medical history was unremarkable. Physical examination demonstrated a soft, solitary, painless mass, measuring 3 cm in diameter. The ultrasonography performed in Ondokuz Mayis University Medical School Hospital revealed a 29X24x17 mm, T2-hyperintense cystic lesion with regular contour at the S2-S4 localisation of the sacral area under the skin. It did not had any extension into the spinal canal. The patient was operated in the pediatric surgery department with the pre-diagnoses of pilonidal cyst, lipoma and meningocele, and the specimen was sent to the laboratory. On surgical exploration, it became apparent that mass was injected with methylene-blue [Table/Fig-1]. The material was covered with 4x2.5 cm surface of skin ellipse and dimensions of 4x4x3 cm. In the section of the material, there was a 3.5x2.5x3 cm cyst with haemorrhagic fluid discharge and regular internal lining [Table/Fig-2]. Histopathological examination revealed a cystic structure in deep dermis and subcutaneous tissue. The cyst was composed of columnar epithelium, with focal areas of pseudostratified columnar epithelium. It was surrounded by loose fibroconnective tissue. There was no inflammatory cell [Table/Fig-3,4]. Immunohistochemically, epithelium of the cyst stained positive for pan-cytokeratin (Clone AE/1/AE3, Genemed), EMA (Clone GP1.4, Novocastra), Oestrogen Receptor (Clone SP1, Biocare), Progesterone Receptor (Clone16, Novocastra) and Pax 8 (CloneZR-1, BioSB) [Table/Fig-5,6,7,8 and 9] and stained negative for S100 (Clone 4C4.9, Thermoscientific), CEA (Clone CEA 88, Biogenex), TTF1 (Clone 8G7G3/1, Genemed) and GFAP (Clone GA-5, Thermoscientific). Histochemical studies with PAS revealed some positively stained cells. [Table/Fig-10]. According to the histopathological and immunohistochemical findings, CCC diagnosis was made.
Methylene blue injected mass.

Excision material covered with skin.
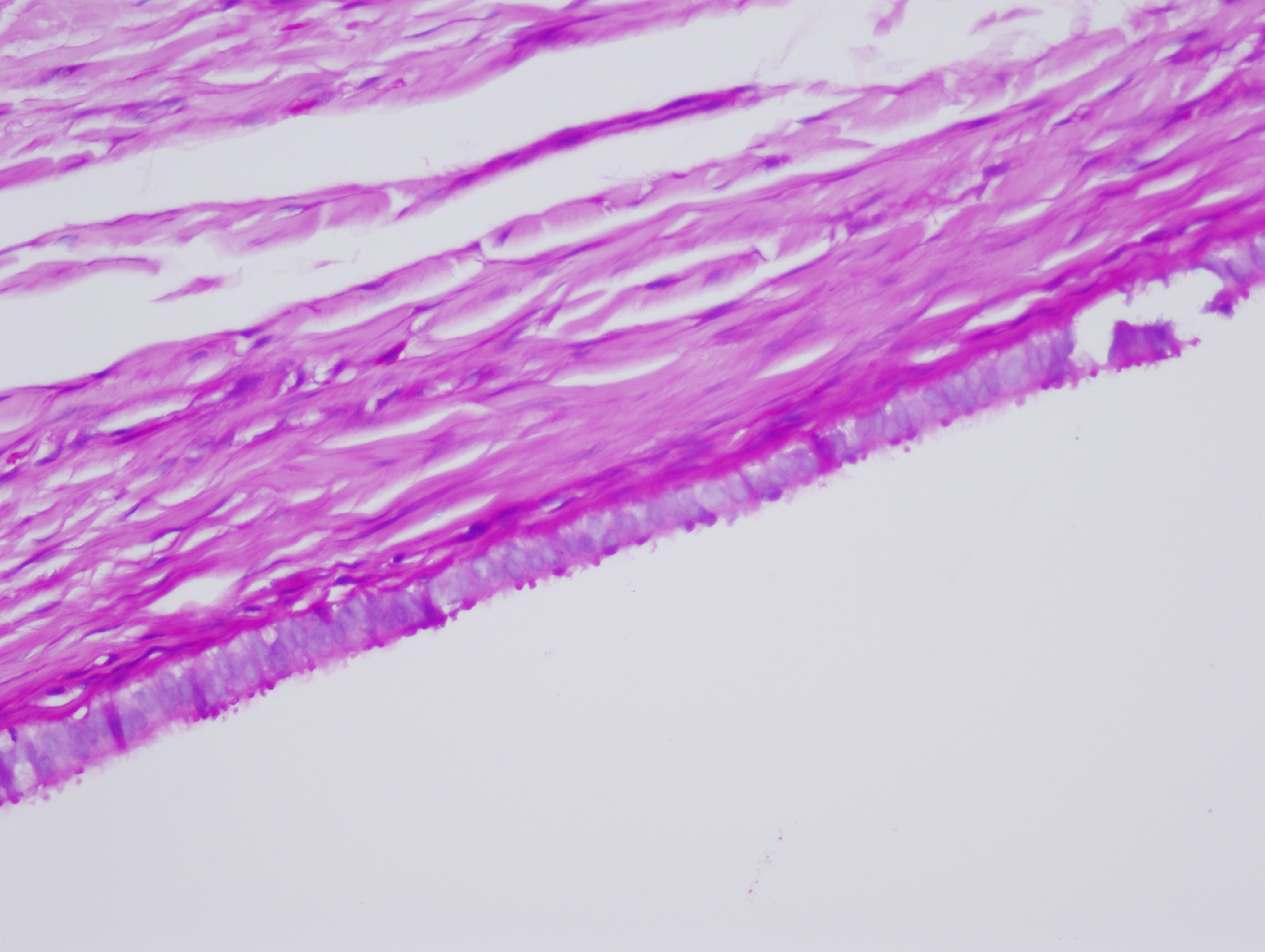
Relation of the cyst with the skin (H&E, 40X).
Epithelium of the ciliated cyst (H&E, 100X).
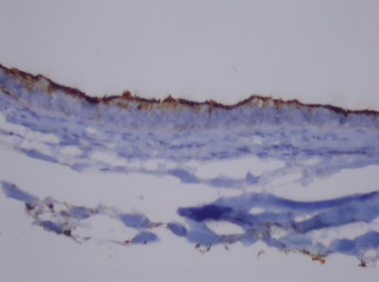
Nuclear pankeratin positivity in epithelium (DAB, 400X).
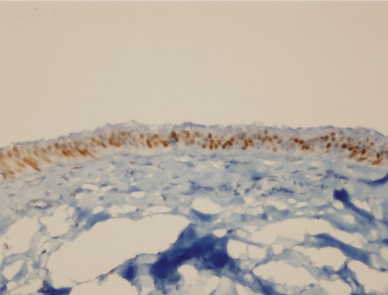
Nuclear EMA positivity in epithelium (DAB, 40X).
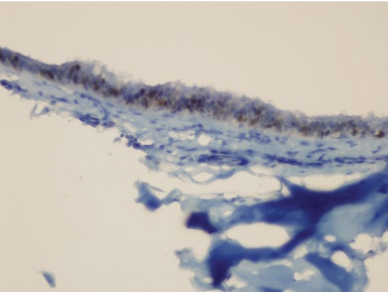
Nuclear ER positivity in epithelium (DAB, 100X).
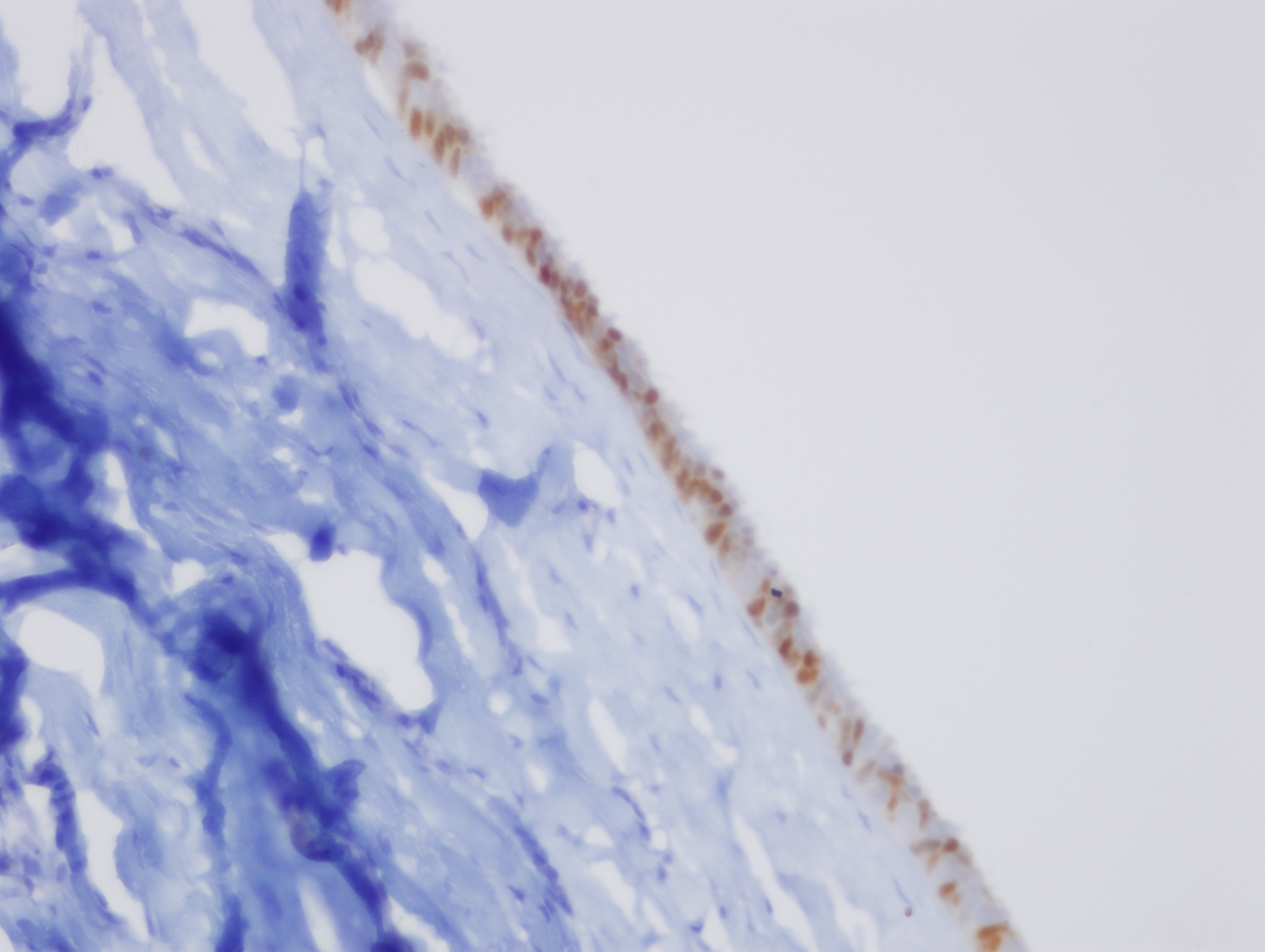
Nuclear PAX 8 positivity in epithelium (DAB, 100X).
Nuclear PR positivity in epithelium (400X).
PAS positivity in epithelium (PAS, 400X).
Discussion
Cutaneous Ciliated Cyst (CCC) is a rare benign cystic tumor often encountered in young women. It usually occurs in the dermis or subcutaneous tissue of the upper extremities and perineal region [1-3]. In the literature, CCC appears typically in the adolescence and reproductive period. It may grow during menstruation or pregnancy due to hormonal effects [3-5]. It has also been reported in males in atypical locations [4,6]. Atypical locations such as scalp, scapula, fingers, abdominal wall and mediastinum have also been reported [1,7-11].
Typically, CCCs are single, unilocular or multilocular, epithelial cysts. The epithelium lining the cyst can be composed of cuboidal, like the epithelium of the fallopian tube, ciliated or non-ciliated columnar, intercalated round peg cells [2,5]. Focal squamous metaplasia can be observed in the epithelium, while the presence mucinous cell is rare [2,6]. Cyst epithelium is often single-layered, but sometimes it can be pseudostratified, or papillary projections into the lumen may occur [2].
This controversial lesion whose pathogenesis is not known fully was first identified by Hess in 1890 [1-3]. The genesis of CCC is controversial. There are two main theories. According to the Mullerian heterotopia theory, migration and sequestration of the Mullerian rests occur during early embryogenesis (the 6th-7th weeks of gestation). Due to their anatomical closeness to the Mullerian canal, the rests are observed in pelvis, perineum, abdominal wall and deep dermis or subcutaneous tissue of the lower extremities. In puberty, heterotopic Mullerian epithelium secretes serous fluid and causes cyst formation due to hormonal effects. Just like Mullerian heterotopia, CCC is stained positive for EMA, PAX 8, WT-1, ER and PR, but it is usually stained negative for CEA, SMA, S100 or p63 [3,6,7,11]. However, CCC has been reported to show Dynein positivity similar to the fallopian tubal epithelium [3,10]. On the other hand, according to the theory of ciliated metaplasia of the eccrine glands, fetal eccrine duct fundamentally have ciliated epithelium, so the presence of cilia in the eccrine differentiation of the tumor is possible. This theory is proposed to explain the pathogenesis of CCC encountered in men and in atypical locations [2,3,7]. These cases are stained negative for ER and PR like eccrine gland epithelium, but stained positive for CEA, p63, S100, GCDFP-15 [3]. In the case, EMA, PAX8, ER and PR were stained positive, but CEA and S100 were stained negative. These findings support its Mullerian origin.
Pilonidal cysts, abscesses, meningocele, myelomeningocele, dermoid cysts, teratomas and lipomas plays a role in the clinical differential diagnosis of the lesions in the sacral region. Less frequently, chondroma, sweat gland tumors, metastatic masses, giant cell tumors and neurofibromas should also be considered [1]. In a pilonidal cyst, the drainage of the purulent material is typical. Myelomeningocele and meningocele differentiation can be done with the analysis of the cyst fluid and with the help of imaging methods [1]. In the present case, ultrasound revealed that cyst had no relation with the duct. Additionally, GFAP was stained negative in the immunohistochemical examination. Monodermal teratomas may include ciliated respiratory epithelium. TTF-1 is helpful in differentiation [1]. TTF-1 was negative in the present case.
Conclusion
According to the histopathological and immunohistochemical findings, our diagnosis was cutaneous ciliated cyst that was considered to develop according to the Mullerian heterotopic theory. Knowing that surgical excision is enough for the treatment, these rare lesions which mimic various diseases should be kept in mind for differential diagnosis.
[1]. Oh JS, Bhalla VK, Needham L, Sharma S, Pipkin WL, Hatley RM, Müllerian-type, cutaneous ciliated cyst in the gluteal cleft mimicking a pilonidal cystPediatr Surg Int 2014 30:545-48.10.1007/s00383-013-3363-z23913265 [Google Scholar] [CrossRef] [PubMed]
[2]. Bivin WW, Heath JE, Drachenberg CB, Strauch ED, Papadimitriou JC, Cutaneous ciliated cyst: A case report with focus on Mullerian Heterotopia and comparison with ecrine sweat glandsAm J Dermatopathol 2010 32(7):731-34.10.1097/DAD.0b013e3181d43f0120644463 [Google Scholar] [CrossRef] [PubMed]
[3]. Rodrigo-Nicolás B, Terrádez Raro JJ, Armengot-Carbó M, Molés-Poveda P, Pont Sanjuán V, Gimeno Carpio E, Müllerian and ecrine cutaneous ciliated cyst: two entities? The contribution of WT-1 and PAX 8 to diagnosisJ Cutan Pathol 2013 40:608-10.10.1111/cup.1213023550799 [Google Scholar] [CrossRef] [PubMed]
[4]. Santos DL, Mendelsohn G, Perineal cutaneous ciliated cyst in a malePathology 2004 36(4):369-70.10.1080/0031302041000172161815370143 [Google Scholar] [CrossRef] [PubMed]
[5]. Itakura HT, Itakura E, Horiuchi R, Matsumura M, Kiryu H, Takeshita T, Cutaneous ciliated cyst on the leg in a woman of post menapausal ageActa Dermato-venereologiva 2009 89:323-24.10.2340/00015555-062619479143 [Google Scholar] [CrossRef] [PubMed]
[6]. Lee JS, Kım YC, Lee ES, Cutaneous ciliated cyst of the inguinal area in a manJournal Dermatology 2006 2:146-49.10.1111/j.1346-8138.2006.00032.x16556287 [Google Scholar] [CrossRef] [PubMed]
[7]. Hung T, Yang A, Binder SW, Barnhill RL, Cutaneous ciliated cyst onthe finger: A cuaneous mullerian cystAm J Dermatopathology 2012 34(3):335-38.10.1097/DAD.0b013e318233055022240776 [Google Scholar] [CrossRef] [PubMed]
[8]. Fontaine DG, Lau H, Murray SK, Frase RB, Wright JR, Cutaneous ciliated cyst of the abdominal wallAm J Dermatopathol 2002 24(1):63-66.10.1097/00000372-200202000-0001311803285 [Google Scholar] [CrossRef] [PubMed]
[9]. Hattori H, Ciliated cyst of probable mullerian origin arising in the posterior mediastinumVirchows Arch 2005 446:82-84.10.1007/s00428-004-1087-015480767 [Google Scholar] [CrossRef] [PubMed]
[10]. Dini M, Russo GL, Baroni G, Colafranceschi M, Cutaneous ciliated cyst. A case report with immunohistochemical evidence for Dynein in ciliated cellsAm J Dermatopathol 2000 22(6):519-23.10.1097/00000372-200012000-0000711190444 [Google Scholar] [CrossRef] [PubMed]
[11]. Fabien-Dupuis C, Cooper B, Upperman J, Zhou S, Shillingford N, Mullerian-type ciliated cyst of the thigh with PAX-8 and WT1 positivity: a case report and review of the literatureCase Rep Med 2016 2016:248782010.1155/2016/248782028070193 [Google Scholar] [CrossRef] [PubMed]