Conservative Approach in a Patient with Cervical Intraepithelial Neoplasia Type-3 in Pregnancy: Impact on Disease Progression and Pregnancy Outcome
Pradip Kumar Saha1, Garima Sachdeva2, Rashmi Bagga3, Jaswinder Kaur Kalra4, Pranab Dey5
1 Additional Professor, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
2 Junior Resident, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, Delhi, India.
3 Professor, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
4 Professor, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
5 Professor, Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pradip Kumar Saha, Additional Professor, Department of Obstetrics and Gynaecology, Third Floor, Nehru Hospital, PGIMER, Chandigarh-160012, India.
E-mail: pradiplekha@yahoo.co.in
Treatment strategy of Cervical Intraepithelial Neoplasia-3 (CIN 3) in background of High Grade Squamous Intraepithelial Lesion (HSIL) is very different amongst the pregnant and non-pregnant women. This case report highlights the approach of diagnosis and management of CIN 3 in pregnancy. A 32-year-old woman, Fourth Gravida one Live issue and previous 2 Abortion (G4P1021), was diagnosed to have cervical intra-epithelial neoplasia (CIN 3) in pregnancy at 20+1 weeks period of gestation. The decision to continue pregnancy was made. She was followed with LBC and colposcopy 12 weekly during the pregnancy. Her pregnancy was uneventful. She delivered vaginally a live born girl, 2.74 kg at 38+4 weeks. In the postpartum period repeat, Liquid Based Cytology (LBC) and colposcopy-directed biopsy were done. The LBC revealed HSIL while biopsy was suggestive of CIN 3. Cone biopsy was done and histopathology report revealed CIN 3 with margins and tips of cone free of tumour. Thus, in this patient neither progression nor regression was noted with conservative approach and definitive management was deferred until the post-partum period. The aim of this article is to highlight the approach of diagnosis and management of CIN 3 in pregnancy.
Cervical intraepithelial neoplasia, Colposcopy, Conization, High-grade squamous intraepithelial lesion
Case Report
A 32-year-old female patient first visited the OPD for pre-conceptional counselling in view of recurrent pregnancy loss. She had a normal vaginal delivery six years back followed by spontaneous first trimester abortion. There was no other significant history.
Her general physical, breast, thyroid, per-abdominal and per-vaginal examination was unremarkable. As a part of routine screening LBC was taken and she was advised to follow up with work-up for recurrent pregnancy loss (TSH, OGTT, and APLA) and LBC report. The patient was lost to follow-up.
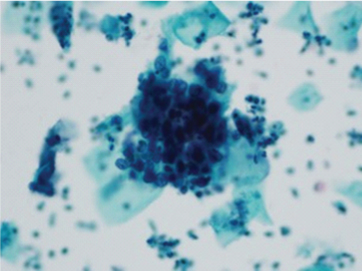
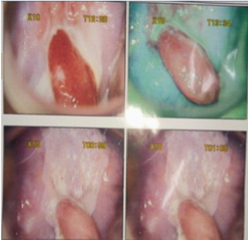
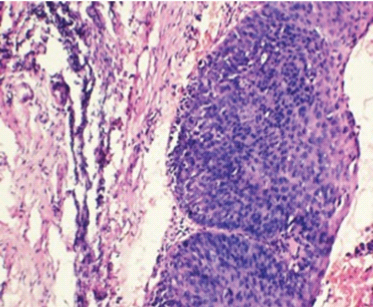
After eight months, she came back to the antenatal OPD with 20+1-week pregnancy. The RPL workup was within normal limits. Her pre-conceptional LBC report revealed HSIL [Table/Fig-1]. Colposcopy [Table/Fig-2] was done which was suggestive of type 2 Transformation Zone (TZ). Dense aceto-white area was present from which biopsy was taken. Also, an endocervical polyp was seen which was excised and sent for histopathology. On green filter application, no abnormal vessels were seen. The histopathology of cervical biopsy was suggestive of CIN 3 [Table/Fig-3] and the polyp was benign endocervical polyp.
Cervical cytology smear showing clusters of round cells with scanty cytoplasm and hyperchromatic moderately pleomorphic nuclei. (Papanicolaou’s stain of sure path preparation X 220).
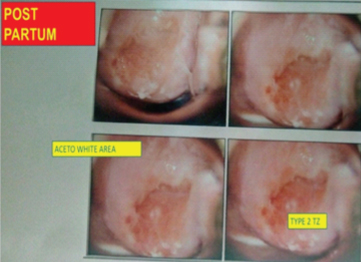
Colposcopy at 20+1 week showing type 2 transformation zone (TZ). An endocervical polyp (upper row left). No abnormal vessels are seen on green filter (upper row right). Dense aceto-white area (lower row).
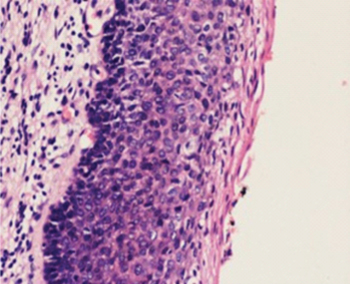
Cervical biopsy showing full thickness involvement of the squamous lining epithelium- CIN 3. (Haematoxylin and Eosin stain X 220).
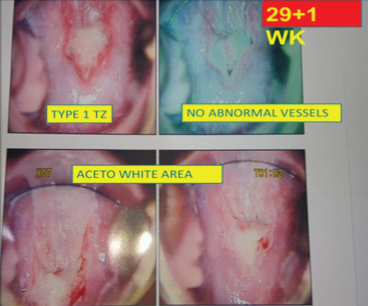
Decision to follow her up with LBC and colposcopy was made. Her routine antenatal investigations were normal. Her repeat LBC and colposcopy was planned at 29+1-week [Table/Fig-4]. Colposcopy findings revealed presence of cervical mucus, type 1 TZ, 1 cm endo-cervical polyp and aceto-white area at 12 0’ clock from which biopsy was taken. There were no abnormal vessels on green filter. LBC was suggestive of HSIL and biopsy revealed CIN 3. Her foetal biometry was normal. She delivered a live born girl, 2.74 kg at 38+ 4 weeks vaginally. She was called at six weeks postpartum for repeat cytology and colposcopy [Table/Fig-5]. There was no progression of disease with similar LBC and colposcopy findings. Cone biopsy was done and histopathology was suggestive of CIN 3 with margins and tip of the cone free of tumour. No invasion was noted [Table/Fig-6]. Thus, in this case there was persistence of CIN 3 with no progression or regression. Now, we plan to follow her up with co-testing at 12 and 24 months followed by routing screening if all reports normal as per ASCCP guidelines [1].
Colposcopy at 29+1-week POG with type 1 TZ, 1 cm endo-cervical polyp, aceto-white area at 12 0’ clock and no abnormal vessels on green filter.
Colposcopy at six weeks post-partum with type 2 TZ and aceto-white area at 12 o’clock.
Postpartum cone biopsy showing persistent full thick involvement by the dysplastic cells- CIN 3. (Haematoxylin and Eosin stain X 220).
Discussion
Cervical cancer is the second most common cancer among Indian women [2]. The lifetime risk of developing cervical cancer among Indian women is 2.5% and risk of death due to cervical cancer is 1.4% [3]. It is also the most common cancer complicating pregnancy with an incidence of 0.1-12/ 10000 pregnancies [4]. The incidence of CIN is 1.3-2.7/10000 pregnancies [4] while the incidence of CIN 3 in pregnancy is less than 1/10000 pregnancies [5].
According to the ASCCP, 2012 guidelines, all women of age more than 30 years should be screened for cervical cancer with three-yearly cytology or every five-yearly co-testing with HPV DNA and cytology [1]. Cytology and colposcopy are absolutely safe in pregnancy [5]. However, endocervical curettage should better be avoided due to the risk of preterm rupture of membranes, preterm labour, and bleeding.
HSIL is a significant cytological finding. The average five-year risk of CIN 3 is 29% if HPV testing is negative and 50% in HPV-positive HSIL and the risk of cervical cancer in these patients is 7% irrespective of HPV status [1]. So, it is mandatory to undergo colposcopy and directed biopsy in order to rule out cervical cancer [1].
CIN 3 does not usually pose any risk to pregnancy or the mother [1]. Moreover, spontaneous regression is noted after delivery in pregnant patients managed conservatively for CIN. Same was observed in the study conducted by Mailath-Pokorny M et al., [6]. In their study, CIN 1, 2 and 3 were diagnosed by colposcopy-guided biopsy in 33.3%, 13.7% and 52.9% of the pregnant women respectively. Pregnant females (post-delivery) with CIN had significantly higher regression rates (56.9% versus 31.4%, p=0.010) as compared to the non-pregnant. Also, significantly lower persistence rates were noted in the pregnant group (39.2% versus 58.8%, p=0.048). They did not observe any progression to invasive disease. The post-partum regression has been postulated because of the physiological changes in the cervical glands and stroma occurring during the antenatal and postnatal period which may have a positive influence on cervical cytology favouring its regression [7]. On the other hand, treatment during pregnancy can result in haemorrhage and pregnancy loss [8].
It is justified to offer patients with CIN diagnosed in pregnancy an option of a conservative approach. A study conducted by Bjorge T et al., found a significantly higher preterm birth and spontaneous abortion rates among the women who were treated with Cone biopsy, laser conization, and LEEP during pregnancy as compared to those who were managed conservatively [9]. The association was stronger for cold knife conization (13% as compared to 5.3%; HR 2.6, 95% CI 1.3–5.3) than laser conization (12% as compared to 5.3%; HR 2.3, 95% CI 2.0–2.5) and LEEP (0.4% as compared to 0.2%; HR 2.3, 95% CI 1.3-4.0) [9].
Also, in accordance with ASCCP, ideal management of CIN 3 in pregnancy is to follow the patient 12 weekly with cytology and colposcopy. Biopsy should only be taken if the cytology is suggestive of invasive disease or colposcopy worsens [1]. Also, to avoid the risk of haemorrhage, colposcopy-guided single biopsy from the most representative area should be taken rather than multiple biopsies. This is supported by the slow progression of CIN to cervical cancer [9]. Hence, it was decided to manage the patient conservatively deferring definite treatment until the postpartum period. No adverse maternal or foetal outcome was observed in the follow-up period.
Vaginal delivery favours regression of CIN as compared to caesarian section. This was observed in a study by Chung SM et al., [7]. There was a significant difference in the regression rates amongst those who delivered vaginally as compared to caesarian section (92.9% versus 63.2%, p=0.016). Various mechanisms have been suggested for postpartum regression. According to Vlahos G et al., it is due to the traumatic alteration followed by post-partum healing of the epithelial cells [10]. Also, the inflammatory reactions occurring secondary to trauma to the cervix during labour and delivery may result in higher post-partum regression [11]. Desquamation of the cervical epithelium during delivery resulting in localised immunological response has also been proposed [11]. This patient also delivered vaginally and there was no progression or regression of CIN noted in the follow up period.
This case highlights the ideal management approach to a patient with CIN 3 in pregnancy. This patient was diagnosed to have CIN 3 in pregnancy and she was followed up with cytology and colposcopy during the pregnancy and postpartum period. No progression or regression was noted during the follow up period and definitive management in the form of cone biopsy was done in postpartum period.
Conclusion
All pregnant females meeting the ASCCP screening criteria should be screened for cervical cancer. Conservative approach in CIN 3 with pregnancy is a reasonable option, provided patient is ready to undergo follow up. Cytology, colposcopy, and directed biopsy are safe in pregnancy. Single biopsy from the most representative area is always preferred. Cone biopsy, LEEP, and other interventions result in the risk of preterm labour and spontaneous abortion. Vaginal delivery is a preferred mode of delivery and favours post-partum regression. Colposcopy and directed biopsy should be done at 6-8 weeks’ post-partum to decide for the definitive management.
List of Abbreviations
| APLA | Anti Phospholipid Antibdy Syndrome |
| ASCCP | American Society for Colposcopy and Cervical Pathology Consensus Guidelines |
| CIN | Cervical Intra-Epithelial Neoplasia |
| HSIL | High-Grade Squamous Intraepithelial Lesion |
| LBC | Liquid Based Cytology |
| LEEP | Large Loop Excision Procedure |
| OGTT | Oral Glucose Tolerance Test |
| OPD | Out Patient Department |
| RPL | Recurrent Pregnancy Loss |
| TSH | Thyroid Stimulating Hormone |
| TZ | Transformation Zone |
| WK | Week |
| YRS. | Years |
[1]. Massad LS, Einstein MH, Huh WK, Katki HA, Kinney WK, Schiffman M, 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursorsJ Low Genit Tract Dis 2013 17(5 Suppl 1):S1-S27.10.1097/LGT.0b013e318287d32923519301 [Google Scholar] [CrossRef] [PubMed]
[2]. Fauser BC, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop GroupFertil Steril 2012 97(1):28-38 e25.10.1016/j.fertnstert.2011.09.02422153789 [Google Scholar] [CrossRef] [PubMed]
[3]. Kaarthigeyan K, Cervical cancer in India and HPV vaccinationIndian J Med Paediatr Oncol 2012 33(1):7-12.10.4103/0971-5851.9696122754202 [Google Scholar] [CrossRef] [PubMed]
[4]. Han SN, Mhallem Gziri M, Van Calsteren K, Amant F, Cervical cancer in pregnant women: treat, wait or interrupt? Assessment of current clinical guidelines, innovations and controversiesTher Adv Med Oncol 2013 5(4):211-19.10.1177/175883401349498823858330 [Google Scholar] [CrossRef] [PubMed]
[5]. Apgar BS, Kittendorf AL, Bettcher CM, Wong J, Kaufman AJ, Update on ASCCP consensus guidelines for abnormal cervical screening tests and cervical histologyAm Fam Physician 2009 80(2):147-55. [Google Scholar]
[6]. Mailath-Pokorny M, Schwameis R, Grimm C, Reinthaller A, Polterauer S, Natural history of cervical intraepithelial neoplasia in pregnancy: postpartum histo-pathologic outcome and review of the literatureBMC Pregnancy Childbirth 2016 16:7410.1186/s12884-016-0861-827055819 [Google Scholar] [CrossRef] [PubMed]
[7]. Chung SM, Son GH, Nam EJ, Kim YH, Kim YT, Park YW, Mode of delivery influences the regression of abnormal cervical cytologyGynecol Obstet Invest 2011 72(4):234-38.10.1159/00032450022024630 [Google Scholar] [CrossRef] [PubMed]
[8]. Karrberg C, Brannstrom M, Strander B, Ladfors L, Radberg T, Colposcopically directed cervical biopsy during pregnancy; minor surgical and obstetrical complications and high rates of persistence and regressionActa Obstet Gynecol Scand 2013 92(6):692-99.10.1111/aogs.1213823590574 [Google Scholar] [CrossRef] [PubMed]
[9]. Bjorge T, Skare GB, Bjorge L, Trope A, Lonnberg S, Adverse pregnancy outcomes after treatment for cervical intraepithelial neoplasiaObstet Gynecol 2016 128(6):1265-73.10.1097/AOG.000000000000177727824756 [Google Scholar] [CrossRef] [PubMed]
[10]. Vlahos G, Rodolakis A, Diakomanolis E, Stefanidis K, Haidopoulos D, Abela K, Conservative management of cervical intraepithelial neoplasia (CIN(2-3)) in pregnant womenGynecol Obstet Invest 2002 54(2):78-81.10.1159/00006771512566748 [Google Scholar] [CrossRef] [PubMed]
[11]. Ahdoot D, Van Nostrand KM, Nguyen NJ, Tewari DS, Kurasaki T, DiSaia PJ, The effect of route of delivery on regression of abnormal cervical cytologic findings in the postpartum periodAm J Obstet Gynecol 1998 178(6):1116-20.10.1016/S0002-9378(98)70310-2 [Google Scholar] [CrossRef]