Portal Vein Pseudoaneurysm: A Rare Complication of Post Pancreaticoduodenectomy Haemorrhage
Ganesh Nagarajan1, Aniruddha Kulkarni2, Vijeth Rai3, Kaushal Kundalia4, Himanshu Pendse5
1 Consultant, Department of Surgical Oncology, P.D. Hinduja National Hospital and Medical Research Center, Mumbai, Maharashtra, India.
2 Consultant, Department of Radiodiagnosis, P.D. Hinduja National Hospital and Medical Research Center, Mumbai, Maharashtra, India.
3 Senior Clinical Associate, Department of Surgical Oncology, P.D. Hinduja National Hospital and Medical Research Center, Mumbai, Maharashtra, India.
4 Liver Transplant Fellow, Liver Transplant Unit, King’s Hospital, London, United Kingdom.
5 Junior Consultant, Department of Radiodiagnosis, P.D. Hinduja National Hospital and Medical Research Center, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vijeth Rai, Senior Clinical Associate, Department of Surgical Oncology, P.D. Hinduja National Hospital, Veer Savarkar Road, Mahim West, Mumbai-400016, Maharashtra, India.
E-mail: vrai4455@gmail.com
Pancreaticoduodenectomy is a complex procedure which is associated with high rates of mortality and morbidity. With the improvement of surgical techniques and skills the mortality rates have come down drastically but morbidity rates have remained constant. Haemorrhage after pancreaticoduodenectomy is a rare complication which is associated with increased mortality and morbidity rates. Gastroduodenal artery is the most common site for haemorrhage. Early haemorrhage is most often due to technical complications while late haemorrhage is due to the pancreatic leak. Surgery and endovascular repairs are the preferred option of treatment. Here, authors present a case of a 60-year-old lady who presented with an upper gastrointestinal bleed following pancreaticoduodenectomy, which was diagnosed as a portal vein pseudoaneurysm. She was treated with endovascular repair.
Pancreaticoduodenectomy, Upper gastrointestinal bleed
Case Report
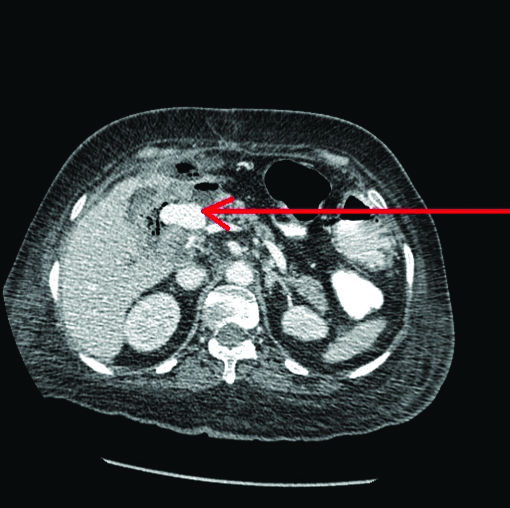
A 60-year-old female patient presented in casualty with abdominal pain, vomiting and malena. Two months earlier, she had been diagnosed with carcinoma head of pancreas for which she underwent pylorus-preserving pancreaticoduodenectomy. Her intraoperative course was uneventful. However, on postoperative day six she developed fever. A Computed Tomography (CT) scan was done which showed a peripancreatic collection for which CT guided aspiration ensued. She was discharged on the 11th postoperative day with the normal expected post-surgical course. On admission, her Haemoglobin (Hb) was 3.2 g/dL, platelet count-2,51,000/cumm, WBC count- 22,000/cumm, serum lactate-144 mg/dL, drain fluid amylase was 8088 U/L. CT scan of the abdomen showed a portal vein pseudoaneurysm [Table/Fig-1].
Contrast CT scan prior to stenting showing pseudoaneurysm arising from the main portal vein as pointed by the red arrow.
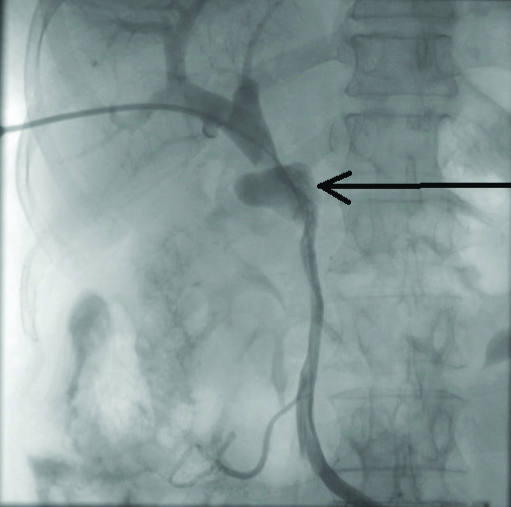
Endovascular repair of the pseudoaneurysm was performed. Under all aseptic precautions, percutaneous right portal vein access was taken with a micro-puncture access kit (Cook Inc. Bloomington USA). Portal venogram confirmed the CT findings demonstrating a pseudoaneurysm arising at the confluence of the portal vein and SMV [Table/Fig-2]. A 10×60 mm self-expanding covered stent (Fluency; BARD Peripheral Vascular, Tempe, AZ) was deployed across the pseudoaneurysm neck [Table/Fig-3].
Sheath was placed in the right branch of portal vein. Portogram showing the pseudoaneurysm arising from the main branch of portal vein as pointed by the arrow.
Black arrow pointing towards the stent placed in the main branch of portal vein. Portogram showing the complete exclusion of pseudoaneurysm from the portal circulation. Red arrow pointing towards the coil placed in the splenic vein to reduce the flow to portal vein.
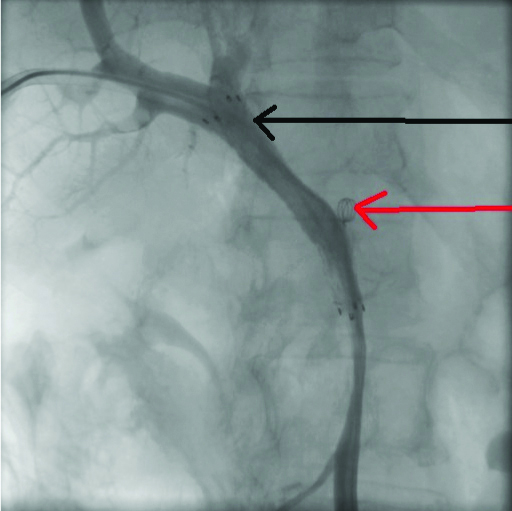
Post-procedure portogram showed complete exclusion of pseudoaneurysm from the portal circulation. CT guided pigtail drainage of the peripancreatic collection was performed with a 12Fr drainage pigtail catheter (CooKInc, Bloomington USA). Parenteral antibiotics were given post-procedure and the patient required inotropic support as well. Unfortunately, her clinical condition gradually deteriorated despite medical expert’s best efforts and she succumbed to multi-organ failure related to sepsis 16 days after the procedure.
Discussion
Post Pancreaticoduodenectomy Haemorrhage (PPH) is rare but serious complication of pancreaticoduodenectomy. It has got a high mortality rate. Despite improvements in surgical techniques, haemorrhage still remains one of the most dreaded complications of pancreaticoduodenectomy [1,2]. PPH occurs in 2-8% of cases and carries a mortality rate of 11-38% [2,3]. The most common source of bleeding is from the peripancreatic vascular structures, mainly the stump of the gastroduodenal artery, hepatic artery and superior mesenteric artery [2-4]. Although quite a rare occurrence, the portal vein can also be a source of postoperative bleeding [5,6]. Present patient had a Grade C PPH [2]. Portal vein pseudoaneurysm is a rare and unusual cause for haemorrhage after pancreaticoduodenectomy. There is a positive correlation between pancreatic leak, intra-abdominal sepsis and pseudoaneurysm formation [3]. It is known that pancreatic leaks damage the vascular integrity due to infection and associated inflammation [3].
Multidimensional CT angiography has become the preferred imaging modality for evaluation of nontraumatic emergent abdominal vascular complications [7]. Aggressive surgical approach remains the treatment of choice in early haemorrhage [2,3,8]. Delayed PPH resulting from arterial blowouts and pseudoaneurysms are generally managed with interventional radiological procedures [5,6,9]. Surgical repair is considered the standard treatment for portal vein aneurysm, however, it is a difficult task in the setting of the recent surgery and associated inflammation [10]. In such a setting, endovascular treatment option is attractive as it is less invasive.
To the best of our knowledge, this is the second reported case of portal vein pseudoaneurysm after pancreaticoduodenectomy. The first case was reported by Burke CT and Park J, where the patient presented with massive gastrointestinal bleeding following pancreaticoduodenectomy due to the development of a portal vein pseudoaneurysm with a porto-enteric fistula. The patient was managed surgically during which the defect in the portal vein was repaired with cadaveric vein patch [5].
Conclusion
Portal vein pseudoaneurysm is a rare complication of pancreaticoduodenectomy. Haemorrhagic complications following pancreaticoduodenectomy can be managed surgically or by endovascular repair. In delayed haemorrhage, endovascular repair can be preferred.
[1]. Ginsburg M, Ferral H, Alonzo MJ, Talamonti MS, Percutaneous transhepatic placement of a stent-graft to treat a delayed mesoportal hemorrhage after pancreaticoduodenectomyWorld J Surg Oncol 2014 12:31510.1186/1477-7819-12-31525315011 [Google Scholar] [CrossRef] [PubMed]
[2]. Wente MN, Veit JA, Bassi C, Post pancreatectomy hemorrhage (PPH)-An International Study Group of Pancreatic Surgery (ISGPS) definitionSurgery 2007 142(1):20-25.10.1016/j.surg.2007.02.00117629996 [Google Scholar] [CrossRef] [PubMed]
[3]. Rajarathinam G, Kannan DG, Vimalraj V, Post pancreaticoduodenectomy haemorrhage: Outcome prediction based on new ISGPS Clinical severity gradingHpb 2008 10(5):363-70.10.1080/1365182080224708618982153 [Google Scholar] [CrossRef] [PubMed]
[4]. Asai K, Zaydfudim V, Truty M, Management of a delayed post-pancreatoduodenectomy haemorrhage using endovascular techniquesHpb 2015 17(10):902-08.10.1111/hpb.1246426235930 [Google Scholar] [CrossRef] [PubMed]
[5]. Burke CT, Park J, Portal vein pseudoaneurysm with portoenteric fistula: an unusual cause for massive gastrointestinal hemorrhageSemin Intervent Radiol 2007 24(3):341-45.10.1055/s-2007-98574821326482 [Google Scholar] [CrossRef] [PubMed]
[6]. Suzuki K, Igami T, Komada T, Stent-graft treatment for extrahepatic portal vein hemorrhage after pancreaticoduodenectomyActa Radiol open 2015 4(6):205846011558933810.1177/205846011558933826137314 [Google Scholar] [CrossRef] [PubMed]
[7]. Frauenfelder T, Wildermuth S, Marincek B, Boehm T, Nontraumatic Emergent Abdominal Vascular Conditions: Advantages of Multi-Detector Row CT and Three-Dimensional ImagingRadioGraphics 2004 24(2):481-96.10.1148/rg.24202571415026595 [Google Scholar] [CrossRef] [PubMed]
[8]. Blanc T, Cortes A, Goere D, Hemorrhage after pancreaticoduodenectomy: when is surgery still indicated?Am J Surg 2007 194(1):3-9.10.1016/j.amjsurg.2006.08.08817560900 [Google Scholar] [CrossRef] [PubMed]
[9]. Gervais DA, Fernandez-del Castillo C, O’Neill MJ, Hahn PF, Mueller PR, Complications after Pancreatoduodenectomy: Imaging and Imaging-guided Interventional ProceduresRadioGraphics 2001 21(3):673-90.10.1148/radiographics.21.3.g01ma1667311353115 [Google Scholar] [CrossRef] [PubMed]
[10]. Shrikhande GV, Khan SZ, Gallagher K, Morrissey NJ, Endovascular management of superior mesenteric artery pseudoaneurysmJ Vasc Surg 2011 53(1):209-11.10.1016/j.jvs.2010.07.07121184935 [Google Scholar] [CrossRef] [PubMed]