Paraganglioma of the Urinary Bladder – A Diagnostic Dilemma
Bhaskar Smitha1, Koppalkar Kiran Rachana2, Pai Muktha Ramesh3
1 Postgraduate student, Department of Pathology, A.J Institute of Medical Sciences, Mangalore, Karnataka, India.
2 Postgraduate Student, Department of Pathology, A.J Institute of Medical Sciences, Mangalore, Karnataka, India.
3 Professor, Department of Pathology, A.J Institute of Medical Sciences, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. B Smitha, Manasmitha House, Kangila Road, Ukkinadka, Via Perla-671552, Kasaragod, Kerala, India.
E-mail: smithabhaskar00@gmail.com
Paraganglioma of the urinary bladder is a unique neuroendocrine tumour originating from chromaffin tissue of the sympathetic nervous system. Clinically, patients may be asymptomatic or may present with hypertension or haematuria. Imaging features may suggest urothelial carcinoma. An uncommon case of a silent paraganglioma of the urinary bladder in an elderly female is documented here, who presented with a single episode of haematuria. Transurethral resection biopsy was performed with suspicion of malignancy. Histopathological evaluation revealed paraganglioma of the urinary bladder, which was confirmed by immunohistochemistry. These tumours require complete surgical excision and should be included in the differential diagnosis of any solitary bladder mass.
Catecholamines, Chromogranin, Cystectomy, Neuroendocrine tumour, Transurethral resection
Case Report
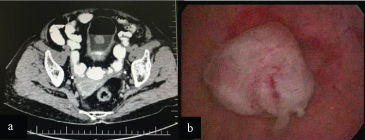
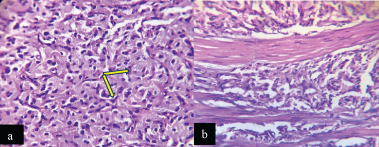
A 67-year-old female presented to the urology department with a single episode of haematuria with passage of blood clots since one day. The patient had no other complaints. Ultrasonography of the abdomen showed hyperechoic area at right lateral wall of urinary bladder. CECT abdomen revealed a mass on the posterior wall and dome of the bladder measuring 18x15 mm involving full thickness of urinary bladder [Table/Fig-1a]. The patient was a known hypertensive on medication, with blood pressure of 120/80 mmHg at the time of admission. Routine haematologic investigations revealed anaemia with Hb of 8.2 g/dL. Urinalysis showed numerous RBCs, albumin and pus cells. Urine cytology was negative for malignant cells. Cystoscopy showed a polypoid fleshy lesion at the dome of the bladder measuring 2×2 cm [Table/Fig-1b]. Clinically, carcinoma of the bladder was suspected. The patient was subjected to a cold cup biopsy. Histopathologic examination revealed nests of polygonal cells with pink granular cytoplasm arranged in a characteristic Zellballen organoid growth pattern [Table/Fig-2a]. There was no evidence of necrosis or mitoses. The neoplasm was dissecting through the muscularis propria [Table/Fig-2b].
a) CECT abdomen: Mass in the posterior wall and dome of bladder; b) Cystoscopy: Polypoid fleshy lesion at the dome of bladder.
a) Section shows Zellballen pattern of tumour cells (yellow arrow) (H&E stain 20X); b) Tumour cells infiltrating the muscular layer (H&E stain 20X).
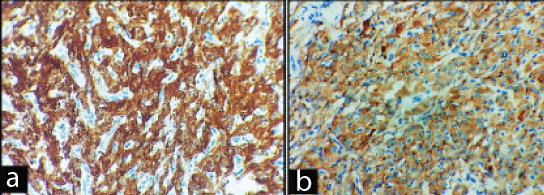
Diagnosis of paraganglioma was given. Immunohistochemical staining revealed a strong cytoplasmic chromogranin and synaptophysin positivity [Table/Fig-3]. The patient was planned for a partial cystectomy after 2 weeks. Unfortunately patient did not come for surgery or follow up as she was clinically normal.
Strong immunoreactivity for: (a) synaptophysin (DAB, 40X); and (b) chromogranin (DAB, 40X).
Discussion
Paragangliomas (PGLs) are tumours emerging from the paraganglia located along the parasympathetic nerves in the head, neck, mediastinum, along the sympathetic chain and urinary bladder [1]. Of these, 10% are localized in the bladder wall, accounting for 0.05% of all bladder tumours [2]. The first case of paraganglioma (pheochromocytoma) of the urinary bladder was reported by Zimmerman I et al., [3]. These tumours can occur in any age, common in females with a mean patient age of 43.3 years.
The tumours are often hormonally active, causing hypertension in 1/3rd of the patients. Even though most common presentation is haematuria, many of them have voiding associated symptoms of headache, blurred vision and sweating [4]. About 17% of bladder paragangliomas are hormonally nonfunctional and can be asymptomatic [5].
Due to the lack of classical symptoms in a silent paraganglioma, preoperative diagnosis is a challenging task. Consequently, imaging modalities with serum and urine markers should be used for further evaluation [6]. On suspicion of paraganglioma, one should estimate the biochemical parameters like catecholamines, metanephrine and vanillyl mandelic acid secretion in either blood or urine. The preoperative catecholamine levels maybe deceiving as most of the cases are hormonally inactive [7]. In the study done by Menon S et al., on 14 cases of paraganglioma, only one case presented with hypertension and raised suspicion for paraganglioma, whereas all other cases had haematuria as chief complaint [8].
Priyadarshi V et al., has illustrated a case of silent paraganglioma in an elderly lady who presented with only one episode of haematuria. The patient developed severe hypertension during its trans-urethral resection, but was efficiently controlled [9]. The differentiation between benign and malignant paraganglioma has been argumentative. Metastasis to other organs has been the decisive proof of malignancy. Tumour necrosis, high mitosis greater than 3/30 high power field, capsular invasion, large nests with central degeneration, lack of hyaline globules, high nuclear/cytoplasmic ratio, uniform cytological pattern and spindle cell patterns are symbolic of increased malignant behaviour [7]. It may be misdiagnosed as nested variant of urothelial cancer because of frequent involvement of the detrusor muscle layer [7]. Nested variant of urothelial carcinoma shows confluent small nests and abortive tubules of mildly atypical cells mimicking Zellballen architecture dissecting through the lamina propria and/or muscularis propria [8]. Paragangliomas are positive for neuroendocrine markers (synaptophysin, chromogranin), whereas nested variant of urothelial carcinoma is immunoreactive for cytokeratin and p63 [10]. Other morphological differentials include malignant melanoma, metastatic renal cell carcinoma of the bladder, granular cell tumour, carcinoid tumours [8].
Conclusive diagnosis requires correlation of clinical, histological parameters and immunohistochemical markers like cytokeratin, epithelial membrane antigen, HMB-45, S-100 protein, chromogranin, synaptophysin and Non specific enolase (NSE) [11]. The treatment of choice in most of the bladder paragangliomas is surgical resection; either Transurethral Resection of Bladder Tumor (TURBT) after control of co-existent hypertension or a partial cystectomy [8]. Approximately, 30% of paragangliomas are familial and exhibit germline mutations associated with Von-Hippel Lindau (VHL) syndrome, MEN2 syndrome, NF1, RET oncogene and Succinate Dehydrogenase (SDH) mutations [8]. Hence, genetic testing plays a vital role.
Conclusion
In conclusion, paraganglioma of the urinary bladder is a rare tumour and may cystoscopically and histologically mimic an urothelial neoplasm. Significant cautery artifacts in a transurethral resection specimen may lead to erroneous diagnosis. Hence, awareness of this entity amongst urologist and pathologist is of utmost importance, to avoid surgical misadventures and labeling of this entity as a urothelial neoplasm. A high index of suspicion, careful search for the characteristic histologic features and application of immunohistochemistry is important to differentiate this tumour from other bladder tumours.
Long term follow up is essential as the disease can recur decades after the initial event.
[1]. Lloyd RV, Adrenal cortical tumours, pheochromocytomas and paragangliomasMod Pathol 2011 24:S58-65.10.1038/modpathol.2010.12621455202 [Google Scholar] [CrossRef] [PubMed]
[2]. Moch H, Humphrey PA, Ulbright TM, Reuter VE, Tumours of the urinary tractIn: WHO classification of tumours of the urinary system and male genital organs 2016 4th edLyonIARC:77-133. [Google Scholar]
[3]. Zimmerman I, Biron R, MacMahon H, Pheochromocytoma of the urinary bladderN Engl J Med 1953 249:25-26.10.1056/NEJM19530702249010613063676 [Google Scholar] [CrossRef] [PubMed]
[4]. Fletcher CD, Tumours of the urinary tractDiagnostic histopathology of tumours 2000 4th edPhiladelphia, PAChurchill Livingstone Elsevier:610-57. [Google Scholar]
[5]. Al Zahrani AA, Recurrent urinary bladder paragangliomaAdv Urol 2010 2010:91212510.1155/2010/91212520672008 [Google Scholar] [CrossRef] [PubMed]
[6]. Tsamboukas G, Vossos V, Gkeka K, Kotsikogianni I, Papatsoris A, Paraganglioma of the urinary bladderHellenic Urology 2017 29(4):47-51. [Google Scholar]
[7]. Ranaweera M, Chung E, Bladder paraganglioma: a report of case series and critical review of current literatureWorld J Clin Cases 2014 2(10):591-95.10.12998/wjcc.v2.i10.59125325073 [Google Scholar] [CrossRef] [PubMed]
[8]. Menon S, Goyal P, Suryawanshi P, Tongaonkar H, Joshi A, Paraganglioma of the urinary bladder: A clinicopathologic spectrum of a series of 14 cases emphasizing diagnostic dilemmasIndian J Pathol Microbiol 2014 57:19-23.10.4103/0377-4929.13087324739826 [Google Scholar] [CrossRef] [PubMed]
[9]. Priyadarshi V, Pal DK, Paraganglioma of urinary bladderUrol Ann 2015 7:402-04. [Google Scholar]
[10]. Amin MB, Tickoo SK, Other tumours of urinary bladderDiagnostic Pathology: Genitourinary 2016 2nd edPhiladelphia, PAElsevier:462-69. [Google Scholar]
[11]. Patnayak R, Preetam P, Jena A, Subramanian S, Lakshmi AY, Space occupying lesion (paraganglioma) of the urinary bladder in a young male: A case report and brief review of the literatureJ Can Res Ther 2015 11(4):103910.4103/0973-1482.14738626881655 [Google Scholar] [CrossRef] [PubMed]