Diabetes mellitus is an ever increasing disease in developing countries more so in the middle age group population. This prevalence pattern is different from developed countries in which the disease process is seen in an older age group [1]. In terms of Indian population the increase in prevalence of this disease is attributable to changing lifestyle which includes sedentary habits and lack of physical activity. Peripheral Arterial Disease (PAD) is a pandemic and one of the most under recognised complication of diabetes mellitus in spite of contributing to disease morbidity to a great extent. Pathologically it manifests in the form of inadequate tissue perfusion caused by atherosclerotic changes that may be acutely compounded by thrombotic or embolic phenomenon. It is a clinical disorder characterized by stenosis and or occlusions of branches of aorta with much higher affliction for lower than upper limbs presenting as distinct clinical identities of claudication and ischaemia [2]. Further progression of clinical symptoms leads to rest pain, critical ischaemia, ulceration, gangrene and potentially amputation. In an attempt to obviate invasive angiographic investigations, need of non-invasive techniques was felt which could not only identify presence and extent of disease but also a useful tool in follow-up of these cases and reducing morbidity as well as mortality. Clinical evaluation followed by non-invasive imaging by CDUS and CTA are main stay for the definite diagnosis of this disease process. Conventional arteriography is being considered as the gold standard imaging modality for the evaluation of PAD albeit lacking in assessing haemodynamic significance of stenotic arterial segments [3]. CDUS is safe, popular, cost-effective repeatable, non-invasive modality that provides both anatomical and haemodynamic information in the form of degree and extent of occlusive lesions [4]. It also plays a role in follow-up of postoperative cases. It has limited role in evaluation of complex anatomical sites as in adductor canal, in morbid obese patients, those with significant limb swelling or ulceration [5]. CTA has emerged as another promising tool having a short examination time, three dimensional imaging capabilities, uncompromised imaging in swollen limbs or those with presence of soft tissue pathology and better visualisation of distal leg arterial segments as seen in run off phase. In the recent past CTA has challenged conventional angiography in the evaluation of many regions. In fact the diagnostic accuracy of CTA has been proved superior to that of conventional angiography in evaluation of carotid stenosis patients for preoperative evaluation [6]. The introduction into clinical practice of multi detector row spiral CT with simultaneous acquisition of four channels had a substantial effect on CTA by enabling high resolution imaging of large scan volumes with excellent visualization of small branches and by permitting reduction in dose of iodinated contrast agent [7]. Another study showed the feasibility of multidetector row CTA of distal run off vessels with excellent arterial enhancement and no substantial venous enhancement [8]. Both CDUS and CTA have role to play in non-invasive imaging of PAD. On one hand there is CDUS which is safer, widely available, relatively cost-effective, devoid of potential harmful effects of ionising radiation and iodinated contrast medium and provides objective evaluation in terms of flow velocity and spectral pattern to assess stenotic segments. CTA on the other hand is relatively faster technique in terms of acquisition, being less operator dependent, having relatively less interobserver variability in interpretation of results, far better evaluation of aortoiliac arterial segments. The present study is a comparative analysis between CDUS and CTA in evaluation of PAD by parameters of flow velocities and spectral waveform in CDUS and characteristics of vessel opacification and reduction of vessel diameter on CTA with special emphasis on effect of vascular calcification on assessment of diseased segments.
Materials and Methods
This was a prospective study involving 40 patients between ages of 40 and 70 years having diabetes or any other cardiovascular risk factors based on the questionnaire regarding any concomitant cardiovascular risk factor like diabetes, hypertension, smoking or hyperlipidaemia as well as clinical symptoms pertaining to lower limb arterial system including intermittent claudication, rest pain, alteration in skin colour or trophic changes. The study spanned over a period of one year from June 2013 to May 2014. The study was approved by the ethical committee of the institution. Subjects included were those having diabetes mellitus or other cardiovascular risk factors, those willing to undergo the protocol design after providing patient information sheet and giving written consent. Patients who were allergic to iodinated contrast media, having deranged renal parameters, pregnant patients, those not agreeing to the study protocol and those not providing written consent were excluded from the study.
All patients were subsequently evaluated with both CDUS and CTA. The lower extremity arterial doppler was performed by Esaote my lab 60 that combined real time B mode imaging system with pulsed and continuous wave doppler. In CDUS the patients were scanned from aortic bifurcation till origin of common femoral arteries by 2.5-3.0 MHz frequency curved transducer followed by 7.5-10 MHz frequency transducer from level of common femoral arteries proximally till the level of ankle distally. The corresponding vessels were first evaluated by grey scale for stenosis, thrombosis, intimo-medial wall thickness, presence of any plaque with its characterisation. It was followed by doppler assessment for grading of stenosis based on spectral flow pattern and peak systolic velocities, presence of thrombosis or collateral formation. The doppler angle was kept less than 60 degrees, smallest colour box was chosen, pulse repetition frequency and sample volume size was set optimally to detect best velocity and colour flow pattern.
Following CDUS, patients were subjected to CTA on Siemens Somatom Sensation 40 slice scanner, Germany. The anatomic coverage extended from the T11-T12 vertebral level proximally to the feet distally. Isosmolar iodinated contrast of 300-350mg/ml iodine concentration was injected via antecubital vein at 4ml/second flow rate using 18gauge intravenous cannula with total volume of contrast being 1.5ml/kg according to body weight. The scanning parameters were 120 kV, 280 mAs and 00 gantry tilt with a cranio-caudal scanning direction. The images were acquired via bolus tracking technique with a threshold of 100 HU in abdominal aorta. Initial slice thickness was 5mm and axial reconstruction has been done at 2.0mm interval of 1mm thickness and in coronal and sagittal sections at 2mm interval with 1.0mm overlap. The multiplanar reconstructed images were manipulated to generate Curved Planar Reconstruction (CPR), Maximum Intensity Projection (MIP) and Volume Rendered Technique (VRT) images. The images were analysed for extent and pattern of wall calcification, luminal narrowing, distal run off flow and presence of collateral flow if any.
Statistical Analysis and Graphical Presentation
It was a diagnostic accuracy study. The collected data was analysed and presented in the form of table, charts and diagrams. The statistical analysis was done using 2x2 contingency table of true positive, true negative, false positive and false negative findings on both CDUS and CTA to calculate comparative sensitivity, specificity, positive and negative predictive values of both imaging modalities. The software used for calculation was MedCalc Version 13.2.2.0.
Results
Among 40 patients enrolled in the study, 90% were between ages of 40 and 60, most commonly in 46-50 year age group with predilection for male gender [Table/Fig-1]. The most frequently occurring symptoms were intermittent claudication and rest pain with former more frequent in males and latter in females [Table/Fig-2]. Rest of symptoms were more commonly seen in males except that of colder extremities.
Distribution of patients according to gender and age distribution.
| Males | Females |
|---|
| Age (years) | 40-45 | 46-50 | 51-55 | 56-60 | 61-65 | 66-70 | 40-45 | 46-50 | 51-55 | 56-60 | 61-65 | 66-70 |
| no. | 5 | 9 | 4 | 6 | 1 | 0 | 2 | 3 | 4 | 2 | 3 | 1 |
Distribution of patients according to presenting symptoms.
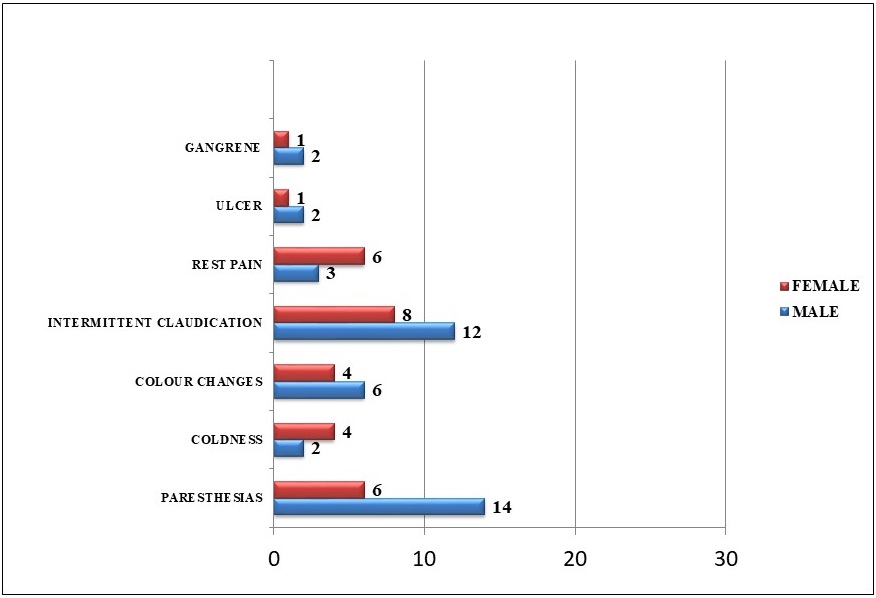
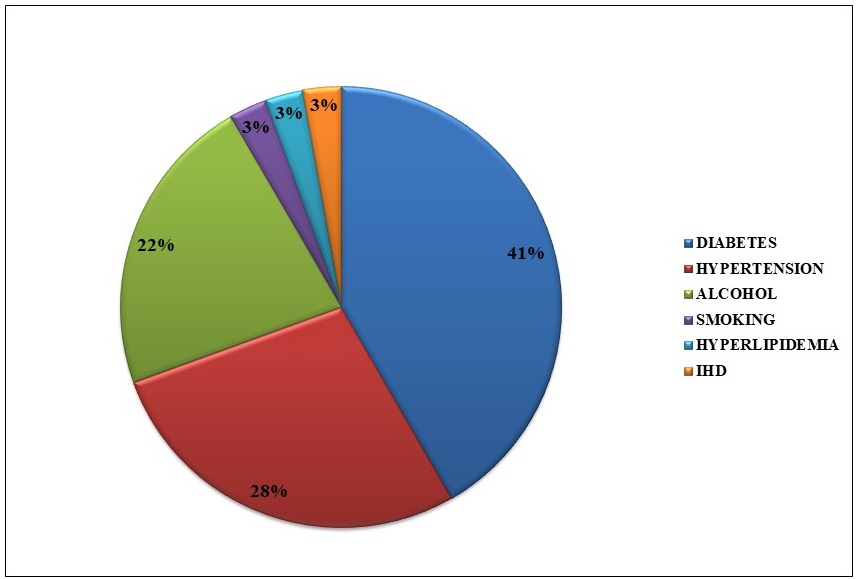
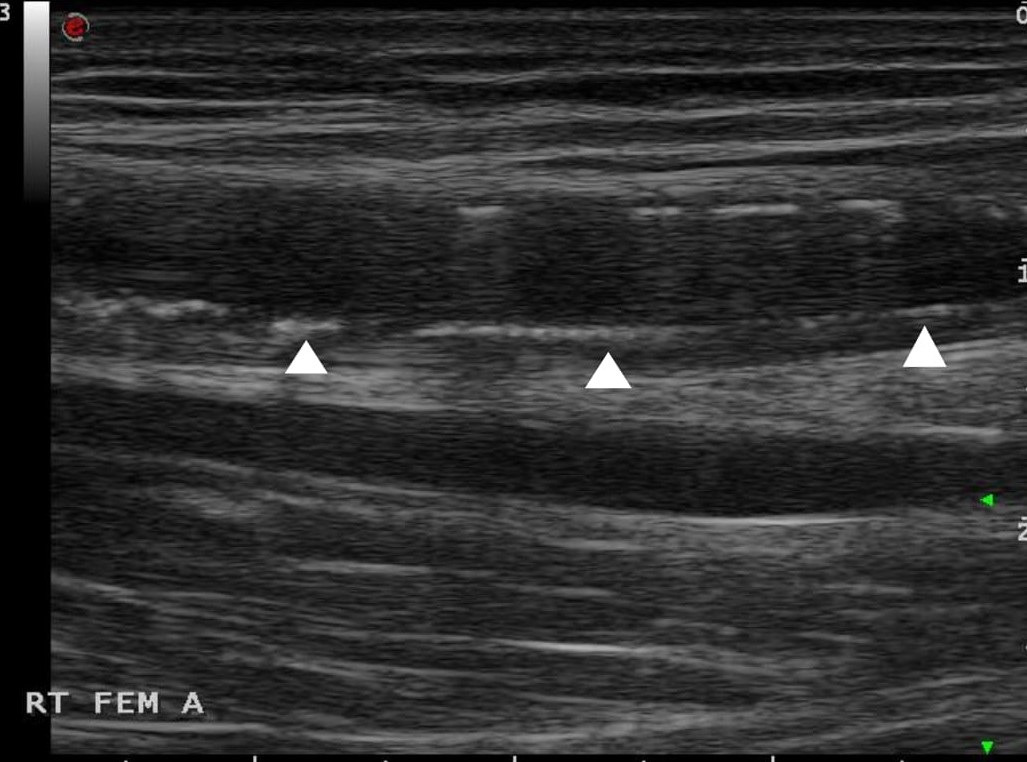
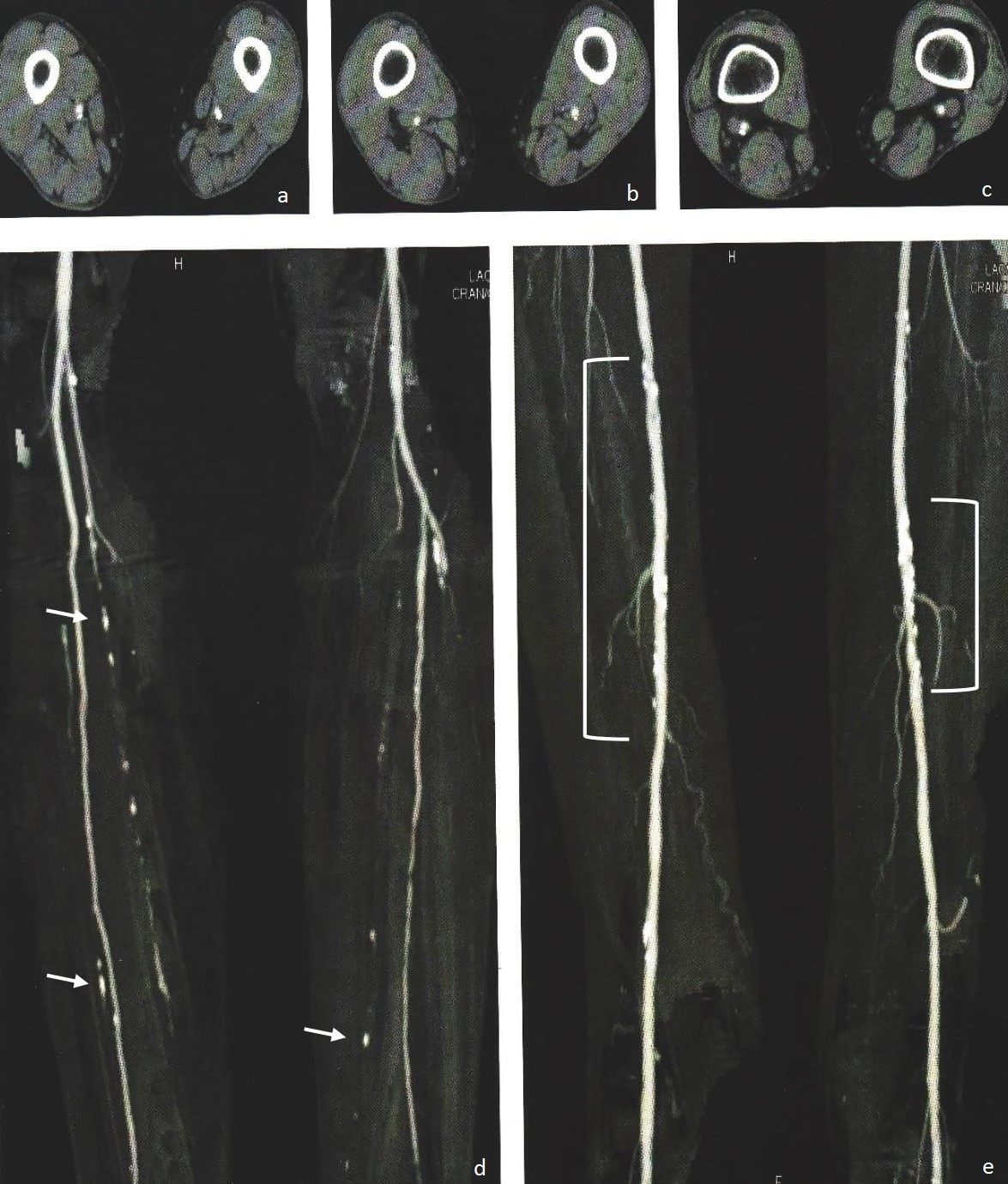
The right limb was more frequently involved with no gender bias. Diabetes mellitus, smoking and hypertension were most frequently occurring risk factors with diabetes mellitus with or without smoking and hyperlipidaemia being strong predictor of vascular calcification [Table/Fig-3,4 and 5]. There was also presence of intimo/medial thickening as well as presence of plaques [Table/Fig-6], the morphology of latter being most frequently moderately echogenic.
Distribution of patients according to risk factors.
Grey scale ultrasonography image shows diffuse wall calcification (white arrowheads) with areas of posterior acoustic shadowing in superficial femoral artery.
Axial and Coronal reconstructed images show diffuse wall calcification involving bilateral superficial femoral, tibial and peroneal arteries (short white arrows in 5d and white brackets 5e).
Grey scale ultrasonography image shows intimo-medial thickening (between calipers) along posterior wall of superficial femoral artery.

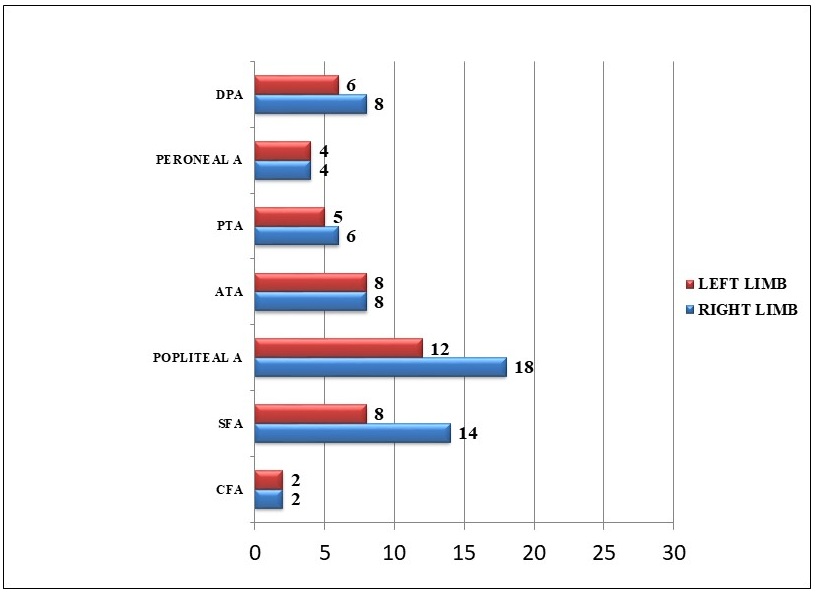
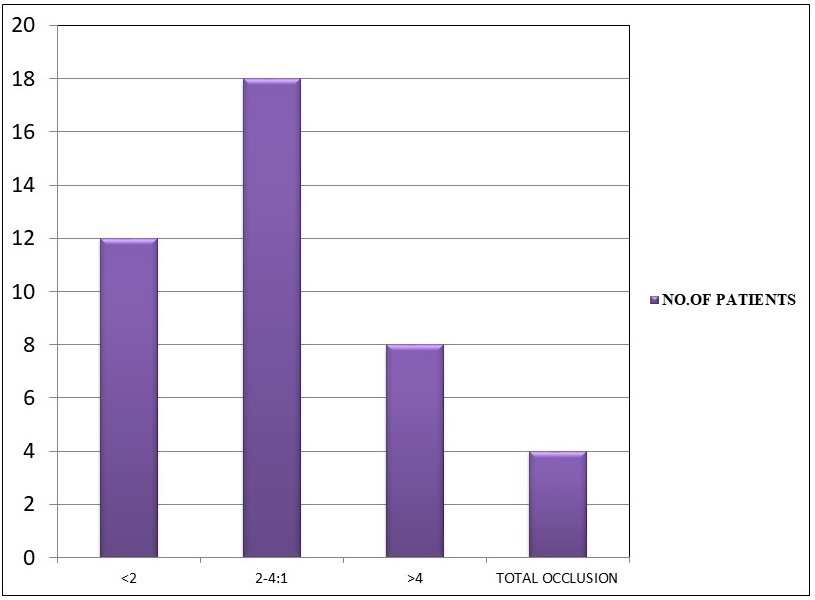
The most frequent site of lesion was popliteal artery in thigh and anterior tibial artery in below knee segments [Table/Fig-7] with CDUS detecting more above knee and CTA detecting below knee lesions more frequently. CDUS was able to detect areas of wall irregularity and <50% stenosis with greater confidence, whereas CTA detected sites of >50% stenosis and occlusion more frequently [Table/Fig-8,9 and 10]. Higher grade of stenosis were seen frequently in leg arterial segments, whereas low grade stenosis were seen more frequently in thigh arterial segments. Majority of patients had PSV (peak systolic velocity) ratio of either <2 or 2-4 [Table/Fig-11]. The overall sensitivity, specificity and accuracy of CDUS in comparison to CTA in our study were 91%, 87% and 89%.
Distribution of patients according to site of lesion (DPA-Deep Peroneal Artery, PTA-Posterior Tibial Artery, ATA-Anterior Tibial Artery, SFA-Superficial Femoral Artery, CFA-Common Femoral Artery).
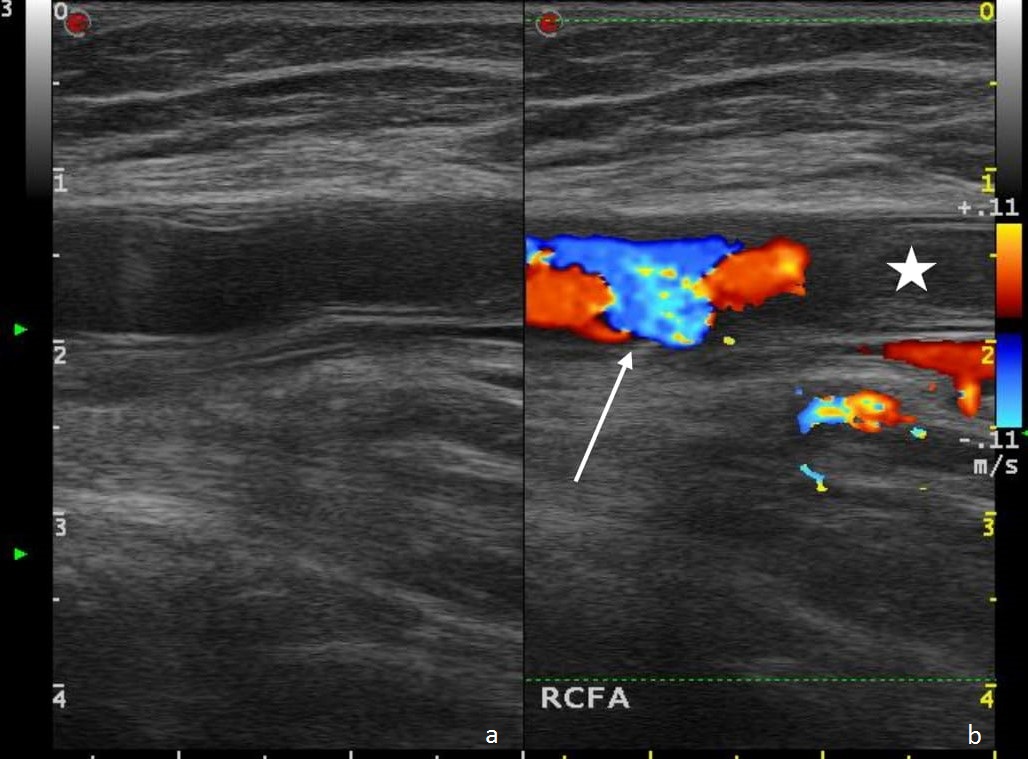
CDUS image showing heteroechoic thrombus in common femoral artery with disruption of laminar flow in proximal patent lumen (white asterisk and white arrow in 8b).
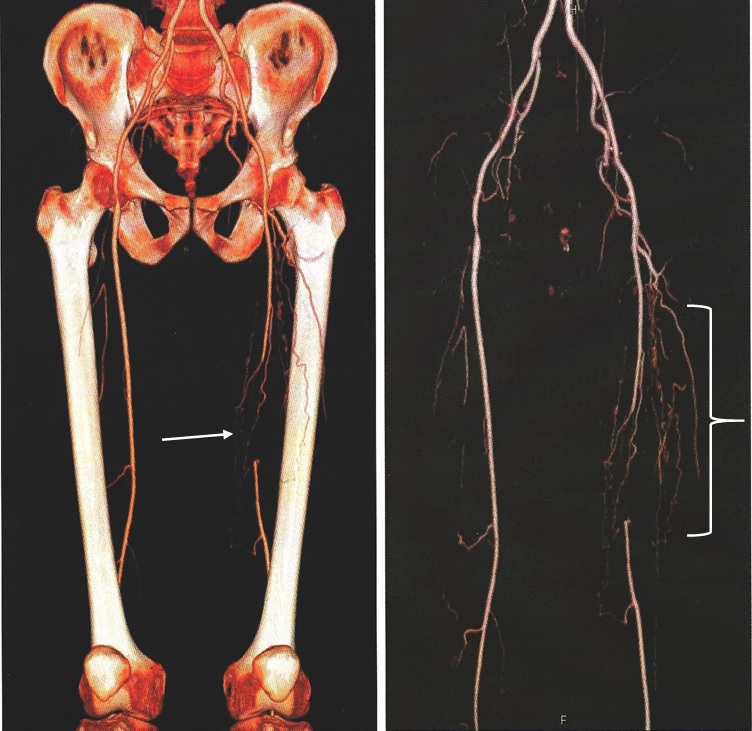
Volume rendered image shows non visualisation of left superficial femoral artery at level of midshaft femur (white arrow in 9a) with presence of multiple collateral vessels across the thrombosed segment (white brace in 9b).
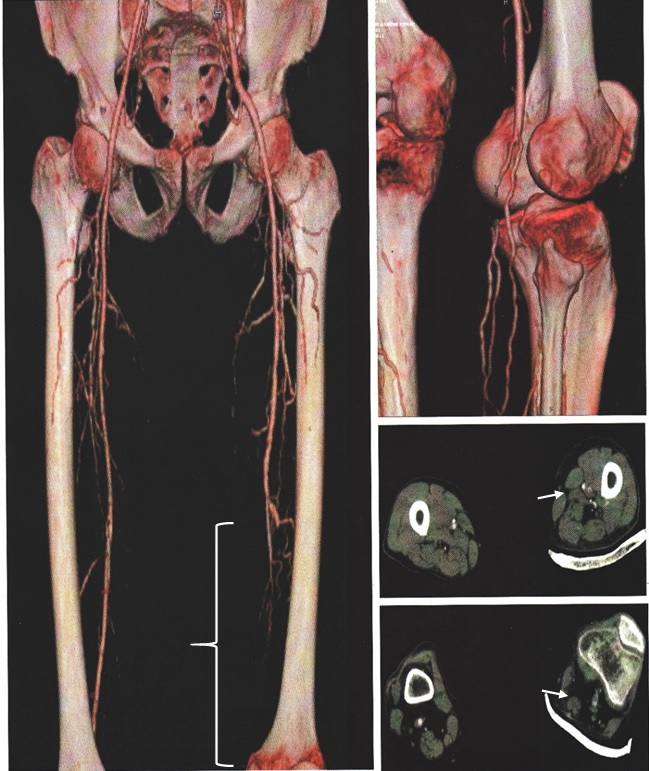
Volume rendered and axial images show complete occlusion of distal left superficial femoral artery (white brace in 10a, short white arrows in 10c and 10d) with normal appearing corresponding arterial segments on right side.
Distribution of patients according to peak systolic velocity ratio.
Discussion
A total of 40 patients were evaluated with both CDUS and CTA. Out of 40 patients 25 were male and 15 were female patients. Majority of patents were between 40 to 60 years of age with mean age of 51 years. The most common associated risk factor was diabetes mellitus followed by smoking and hypertension seen with similar frequency as in another study [9]. Analysis of clinical background revealed that intermittent claudication was the main presenting symptom followed by rest pain along same line with observations of another study [10]. Another study postulated that diabetes itself is a risk factor in propagation of claudication to critical ischaemia of the limb [11].
A total of 510 arterial segments were evaluated by CDUS and 560 arterial segments were evaluated by CTA. Out of 50 arterial segments which could not be assessed on CDUS, reasons were attributed to bowel gas, bony shadowing and improper patient positioning due to associated osteoarthritic changes leading to pain.
In present study, atherosclerotic plaque was seen in 30 patients with moderately echogenic plaque morphology being most frequent. Majority of moderately echogenic plaques were found in 14 patients with diabetes alone or those with diabetes and hypertension, whereas high echogenicity plaques were seen in eight patients with diabetes and hyperlipidaemia.
The corresponding arterial segments showing luminal irregularity in eight cases on CDUS and six cases on CTA, less than 50% luminal stenosis was 16 on CDUS and 14 on CTA, with more than 50% seen in 14 patients on CDUS and 16 patients on CTA with lesions localised to femoropopliteal segment in 60% and infrapopliteal segment in 40% of cases, comparable to study by Faglia E [12]. Complete occlusion was seen in two patients on CDUS and four patients on CTA. In patients who had complete occlusion, the exact site of origin, number of collaterals and distal reformation site were better demonstrated on CTA as compared to CDUS.
The PSV ratio was found to be <2 in 12 patients, 2-4 in 18 patients, >4 in eight patients with complete luminal block in four patients. The PSV ratio was calculated by comparing ratio at site of stenosis and 1-2 cm upstream in an unaffected segment. According to study by Cossman DV et al., PSV ratio of >2 are indicative of haemodynamically significant stenosis in 50-75% range with ratio of >4 corresponding to 75-99% stenosis [13]. Their study had produced accurate quantification of degree of stenosis by using PSV ratio. Similarly in present study we used PSV ratio which was easy to quantify and equally accurate in sub classifying percentage stenosis especially 75-99% stenosis.
As far as spectral waveform is concerned the two main features assessed were change in overall shape of arterial waveform and the degree of spectral broadening. The spectral waveform was monophasic with loss of second and third phases of normal triphasic waveform at and distal to sites of haemodynamically significant stenosis. At a site beyond the stenosis the width of first systolic complex is increased with overall decrease in height representing spectral broadening. No flow was detected in segments of complete occlusion. Proximal to site of obstruction changes seen were reduced diastolic component evident from loss of third component and reduced PSV depicting high peripheral resistance. These findings are comparable to the findings of other studies [13,14]. In our study among the false positive one case showed wall irregularity with other showing <50% stenosis were recognised on CDUS, labelled as occlusion on CTA due to presence of thick wall calcification.
Areas of significant wall calcification signifying stenotic lesion seen on CTA are difficult to assess on both MIP and VR images and require additional imaging in the form of either MR angiography or Digital subtraction angiography with latter preferred if interventional treatment is contemplated [15]. There was also increased prevalence of arterial wall calcification in diabetics [16]. Other predictors for vessel wall calcification found in our study were smoking and hyperlipidaemia. Although the upper age limit of patients in present study was 70 years, still we were not able to demonstrate increase in frequency of vascular calcification among higher age group patients.
The third false positive was detected to have <50% stenosis and PSV ratio of <2 on CDUS seen as >50% stenosis on CTA with similar occurrence postulated as limitation of CTA in evaluating eccentric stenosis in thigh segments [17]. One of the explanations for this marked decrease in velocity is proximal obstruction as well as presence of collateral channels [11] with another possibility being inability to detect tandem lesions [18].
Among the false negatives, two cases were seen in distal thigh segment labelled as <50% stenosis on CDUS and >50% stenosis on CTA. This was attributed to lesions being at the level of adductor canal [17]. Among rest of four false negative, two were seen in proximal and middle third segments of anterior tibial artery with the third at level of peroneal artery. All three segments were interpreted as <50% stenosis on CDUS and occlusion on CTA with long stenotic segment proceeded by proximal occlusion. The reason for this discrepancy is that in such lesions the area of colour flow in lumen is underestimated because flow velocities near the arterial wall were below the sensitivity of the machine as well as low PSV values in long stenotic segment in comparison to high values in short segment stenosis [18]. Another explanation for this result is partial volume averaging seen as superimposition of adjacent branches as stated by Rieker et al., [19]. In contrast to present study, by Martin ML et al., found that CTA underestimates degree of stenosis more frequently than overestimation either due to suboptimal or delayed opacification of leg arteries [20]. This disparity may be also be due to technical differences in the study protocol as well as interpreting results based on different post processing techniques [21]. A statistically significant difference (p<0.05) was established between CDUS and CTA across all grades of stenosis, implying one investigation is better than other across different segments. The overall sensitivity, specificity and accuracy of CDUS as compared to CTA in our study was 91%, 87% and 89% comparable to study by Chidambaram PK et al., [22].
CTA had some limitations, short segment stenosis were missed or underestimated explained by Wise SW et al., that resolution of CTA along Z-axis is inferior. On the counterpart the length of occluded segment was more accurately estimated on CTA as phenomenon of post occlusive flow and retrograde filling of vessel distal to an occlusion [20]. The length of occlusion is an important parameter, short segment occlusion may be treated by interventional techniques whereas surgery is usually preferred for long segment occlusions [23].
Current study showed that orientation and actual percentage of vessel stenosis had a greater impact on accuracy of display of CTA data. These findings suggested that CTA was more accurate in evaluation of vessels oriented perpendicular to axial plane that for vessels having in plane orientation. This was explained as well as proved by Kuszyk BS et al., that VR images were significantly less accurate with phantoms oriented parallel to axial plane [24].
CDUS has advantage over CTA in assessment of haemodynamic significance of stenotic lesions. This quantitative evaluation can be used to identify which patients are to be subjected to CTA leading to improved results and more accurate multimodality approach for disease management. CTA is a three dimensional technique that provides information about the imaged vessel and adjacent structures. It requires only vascular access and can be done on outpatient basis with minimal risk. Post processing with appropriate window selection and use of multiplanar reconstruction generally enables confident discrimination between vascular calcification and intravascular contrast medium. This quality comes as an advantage in planning of endovascular procedures [23]. CTA also has limitations, iodinated contrast administration being a basic prerequisite, time consuming post processing reconstructions and relatively inferior assessment of haemodynamic information as compared to CDUS.
Limitation
The major limitation of CTA in present study was erroneous evaluation of luminal narrowing or thrombosis as well as interpretation of multiplanar reconstructed images in segments showing significant vascular wall calcification. CTA also showed under or overestimation of short segmental stenosis. CDUS showed limit role in long segment of stenosis making vascular mapping difficult, in cases of suspicious thrombosis, evaluation of distal leg segments, when surgical treatment is contemplated and in cases of inadequate examination.
Conclusion
CDUS should be used as a first modality in evaluation of patients of PAD especially where low grade stenosis is anticipated, patients prone for significant vascular calcification especially those with long standing diabetes or diabetes with associated smoking or hyperlipidaemia and those having predominant femoropopliteal disease burden. On the other hand CTA should be first modality of investigation in patients showing clinical signs and symptoms of high grade stenosis, cases suspicious for vascular thrombosis, predominant infrapopliteal disease affliction, non diabetics or recently diagnosed diabetics and those in which surgical or radiological intervention is contemplated. The major predictors for vessel wall calcification in our study were diabetes, smoking and hyperlipidaemia. CDUS showed higher confidence in diagnosing eccentric, low grade and short segment stenosis, wall irregularity/intimo-medial thickening as well as assessing haemodynamic significance of stenotic lesion. On the other hand, CTA showed higher diagnostic confidence in evaluation of long stenotic segments, arteries showing tortuous course and in anatomically complex location, cases of overlying soft tissue lesions abnormality. CTA was accurate than CDUS in determining length of occlusion, post occlusive flow, evaluation of collateral vessels and retrograde filling of vessels distal to site of occlusion.