In the programme of extensive and multidrug resistance cases nosocomial transmission is in the propagation. Along-side with HIV, Tuberculosis (TB) infection is global priority in Healthcare Associated Infection (HAI). Effective prevention strategies are needed to control the transmission of TB mostly in low economic and overcrowded settings of highly susceptible population. TB is the ninth leading cause of death worldwide and also form a single infectious agent, ranking above HIV/AIDS. In 2016, there was an estimated 1.3 million TB deaths among HIV negative people (down from 1.7 million in 2000) and an additional 374 000 deaths among HIV positive people. In 2016, 1936,158 cases of TB were notified by World Health Organization (WHO) in India among which 72% were with known HIV status [1].
India is the country with the highest burden of TB. The WHO TB statistics for India for 2016 gave an estimated incidence figure of 2.79 million cases of TB for India [2]. In 2015, RNTCP (Revised National Tuberculosis Control Programme) was notified with 111 TB cases per 100000 populations. In state of Karnataka, 81187 cases of TB were notified by RNTCP among them 84% of the cases were pulmonary TB [3]. Fundamental infection control practices in India revolve around biomedical waste management and disposal of sharps; while AIC measures were mostly absent from the protocol of health care facilities [4].
The purpose of the study is to assess infection control practices that a health care personnel follows to prevent transmission of TB and to evaluate the resources and facilities available in the area and also to identify the factors which helps to improve the practices; thereby to minimize the risk for transmission of pulmonary TB infections.
Materials and Methods
This study was conducted in a tertiary care multi-specialty hospital in southern India with 82 health care personnel between 2nd January 2017 and 4th February 2017. Pulmonary medicine departments were selected for the study and combination of staff who were working in the pulmonary medicine department were recruited.
The present study adopted sequential explanatory design (QUAN QUAL) of Mix- methodology approach as the researcher wanted to use both quantitative and qualitative methods in an attempt to acquire deeper understandings of health care personnel experiences on infection control practices and identify the factors to improve those practices to prevent pulmonary TB within the single study. Quantitative data was collected among health care personnel by an observation checklist and by administering a structured knowledge questionnaire. After the analysis of these quantitative data researcher has conducted a focus group discussion.
The data was collected after obtaining administrative permission, Institutional Ethical Committee registration (IEC) number is 813/2017. Informed consent was taken from the participant after explaining and participant information sheet was also given to each participant.
Units which take care of patient with pulmonary TB like pulmonary ward, emergency, out-patient department were included for the study. Health care personnel working in the units which take care of pulmonary TB patient were considered for the study. Housekeeping staffs were excluded from assessment of knowledge on infection control. Complete enumerated sampling was used for observing the practices of health care personnel and convenient purposive sampling was used for assessing knowledge and for focus group discussion.
In this study, sample size for the observation of infection control practices by health care personnel consisted of all those events that were observed during the data collection period. One health care personnel was observed maximum for five times. An observation checklist was developed by the researcher. The tool consisted of 25 items which were divided into five domains: Standard precaution, Waste management, Isolation practices, Personal Protective Equipment and Respiratory hygiene.
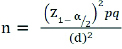
Sample size was calculated based on pilot study findings for assessing knowledge on infection control practices.
Where;
n= minimum sample size
Z1-α/2 = 1.96 at @ 0.05 level of significance
p= anticipated proportion i.e. 0.6 for power 60%
q= 1-p
d= margin of error i.e. 0.05
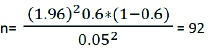
Final sample size was estimated to be 92 including 5% nonresponse rate. But due to time limitation 82 sample were covered for the knowledge assessment.
Sample for Focus group discussion consisted of health care personnel who were available at the time of data collection. The sample used for quantitative were used for qualitative data collection. Sample size was 14.
The survey had captured the socio-demographic data of the respondents. A structured knowledge questionnaire was administered which consisted of 30 items with five domains such as Diagnosis, Transmission, Isolation practices, Personal Protective Equipment, Waste disposable. Each questionnaire had four options from which participants were instructed to select one correct answer. Each question carried one mark thus total score for this tool was 30 which is categorized into Excellent (22-30), Good (16-21), Satisfactory (8-15) and Poor (0-7).
All the tools used in this study were validated by seven experts from the field of Microbiology, Infection Control, Nursing and Pulmonary Medicine. Reliability of the tool was done by split half method using Spearman Brown Formulae and the tool was found to be reliable. R is 0.87.
After collecting and analysing quantitative data a focus group discussion was carried out to collect qualitative data. The discussion was conducted among 14 health care personnel to elicit reason for non-practice and how to overcome the challenges faced. Focus group discussion was conducted among doctors, nurses, respiratory therapist and housekeeping supervisors in the hospital in one clinical class room which is situated in the out-patient department area. The focus group questions were mainly focus on the challenges faced by health care personnel to comply with the infection control practices. The discussion took around two hours. The language of the discussion was English and it was audiotaped. Confidentiality was maintained throughout the study by giving them participant numbers. Data were transcribed to verbatim and validated. Validation was done by few of the participant and experts from qualitative research field. Categories were made by using thematic analysis. Then the investigator identified themes and sub-themes emerging from the data analysis.
Results
Descriptive Analysis:
Majority of the study participants were females 56(68.3%) and age group of 20-30(89.2%), the mean age of the participants were 25.76±5.968 years. Majority of the participants 50(61%) had experience of more than one year and 32(39%) of the participants had less than one year of experience. A total of 69(84.1%) of the participants had not received any training on tuberculosis prevention. Maximum of the participants (56.1%) were nurses [Table/Fig-1].
Socio demographic characteristics.
| Samplecharacteristics | Frequency (f) | Percentage (%) |
|---|
| Age in years20-30>30 | 739 | 89.210.8 |
| GenderMaleFemale | 2656 | 31.768.3 |
| DepartmentNursingRespiratory therapistDoctors | 462313 | 56.12815.9 |
| Work AreaOPDWardEmergencyLaboratory | 1036324 | 12.243.9394.9 |
| Years of experience<1 year>1 year | 3250 | 3961 |
| Training on TuberculosisYesNo | 1369 | 15.984.1 |
N=82
Data shows that among 82 health care personnel, 13(15.9%) participants had excellent knowledge, 48(58.5%) had good knowledge regarding TB infection control practices. Although few 20(24.4%) had average knowledge regarding TB infection control practices [Table/Fig-2].
Frequency (f) and percentage (%) distribution of participants based on knowledge score.
| Knowledge score | Frequency(f) | Percentage (%) |
|---|
| Excellent knowledge>80%(24-30) | 13 | 15.9 |
| Good knowledge60-79%(18-23) | 48 | 58.5 |
| Average knowledge40-59%(12-17) | 20 | 24.4 |
| Poor knowledge<40% (0-12) | 1 | 1.2 |
N=82
The study showed that health care personnel had knowledge gap in the prevention of the transmission of pulmonary TB. Most of them (67.1%) were unaware regarding isolation room characteristics. Fifty three percentage participants were not aware of disposing waste generated from pulmonary TB patients.
In hand hygiene practice performed by health care personnel it was revealed that 67.3% of them did not perform hand hygiene after touching the patient surroundings. Six percent of health care personnel did not perform hand hygiene after body fluid exposure risk. Out of 27 observations 29.6% of health care personnel maintained cough etiquettes in the work settings. N 95 masks were not used by health care personnel whenever required. Most of the time health care personnel were failed to put three layer masks properly (47.8%), it was either hanging in the neck or in the pockets of health care personnel. Biomedical waste bin was not found in the isolation room. Sputum of the suspected TB cases and Active TB cases were not treated with Phenol before discarding it. There was no separate area found in the units for collecting sputum samples.
Thematic Analysis:
The findings of the survey were further analysed in-depth for finding the root causes and creating an awareness to bring the suspected changes. Focus group discussion was conducted for the purpose. Care givers safety vs. Cost, Availability vs. Compliance, Practice vs. Risk and Education vs. Behaviour were the most important theme brought out after the analysis. The themes are described below in details with expressive quotes from the participants.
1. Care givers safety vs. Cost
Most of the participants verbalized that health care personnel who provides care to the TB patient should be taken care for the safety of their health. They should consider safety as a prime concern. In the discussion it was agreed upon that care giver safety should be the priority than the cost. As most of the participants expressed that they were not wearing N95 mask as the cost goes to the patients. N95 masks were not provided by the hospital for the health care personnel.
Participant 2: “Throughout the world now, the care giver safety is first concern, we are not doing charity; we are doing professional work. The care givers safety should be first then the patient, if you are doing some charity work then you are going out of this”.
Sub themes under the main theme emerged were: Comfort of health care personnel, unavailability of Facility, Contact period with the patient and Need based allocation. Participants were asked to clarify whenever needed. One participant stated that wearing N95 mask is very uncomfortable. In addition they told that they cannot wear it for long time as it suffocates.
Participant 7: “First you have to wear and know the practicality; I have worn it during H1N1 outbreak, it was very suffocating. And many people develop claustrophobia like in MRI they have and not only these;they get mad. Nurses are very good, we should really appreciate them that they wear that long.”
The respondent also reported that they do not have the facility of isolation room as per need. Although patient need to be kept in isolation room it was not possible many a times.
Participant 7: “….and we don’t have facilities. The problem is we have TB patient who is diabetics, renal failure on dialysis and ARDS. How do I manage in isolation where there is no dialysis port? He will 100% die; only one thing we can do is probably we can put him in ICU1 isolation that is only 4 bedded.”
Some of the respondents were concerned about the time period that health care personnel spend with patient with active TB. They stressed on to the point that if time period is less that the risk of transmission is less.
Participant 6: “When I go to see a patient in isolation room I don’t discuss; I just go and examine the patient. So when contact period is extremely short; triple layer is fine. But if you are going there and examining, spending more than 10-15 minutes than you cannot wear triple layer mask. It will become a compromise.”
When discussion was focusing on finding a solution for masking, majority of them were agreed that if suspected cases of pulmonary tuberculosis would be known; there is a possibility to control the transmission by giving surgical mask to the suspected case. Discussion came to an agreement of giving a surgical mask to the suspected patient so that source of infection can be controlled.
Participant 7- “That is what I am telling; see there is a balance between practicality. What I meant is in any infection control practices, first things is the source control, as 60-70% infection is from the source; if you can reduce the source most of the problem is solved. Firstly, give mask to the patient that itself will reduce the problem. That is what I do.”
2. Availability vs. Compliance
Most of the participant agreed that there were enough hand hygiene facility e.g., Handrub, wash basin; however compliance of hand hygiene remains low. Some suggested that nurses carrying hand rub and offering it to doctors may increase the compliance. However, there was a strong opposition that this will jeopardize the hand hygiene practice and doctors may forget to do it themselves without support. Nurse’s time for the same is also considered non-productive. Therefore, encouraging the individual to practice hand hygiene as a part of the clinical practice to emphasize and reinforce.
Participant 2-“We are practicing hand hygiene but not entirely, in OPD I do, because wash basin is nearby, everytime I see an OPD patient, I wash my hands. In wards, it is not 100%. But in OPD I do that with every contact. By the end of the day the dustbin used to be full of tissue papers.”
3. Practice vs. Risk
Sputum of confirmed cases of pulmonary TB and suspected TB cases should be treated well as per standards. Most of the participants agreed that they know about sputum disinfection process and same should be carried out in the settings. All of them stressed that giving phenol in the sputum cup to the patient will be helpful for disinfecting the sample before disposing it. Some participants were surprised to hear that facility of waste bin was not provided in isolation room and suggest implementing the same immediately.
Practice: Disinfecting the sputum of pulmonary TB patient
Participant 1-“Before in one hospital where I have worked for TB patients; there we used to put phenol in sputum cups before giving to the patients.”
Risk: Availability of waste management facility and knowledge on waste management
Participant 5- “Waste bins were not there (surprise) it is not acceptable. It must be there.”
4. Education Vs. Behaviour
Influential talk or education to the patient and patient relatives regarding preventive measures on Pulmonary TB is helpful to make the patient and relative aware about the disease and its transmission. All the participants expressed that talking to the patients can have a great impact on their behaviour. It was decided to develop a pamphlet and poster by the staff to educate the patient as well as relatives.
Participant 2-“Many times patients and relatives do not follow instructions. They used to roam here and there. Every time new patient party may come for visiting the patient. We can put some display so that everyone can read it and go.”
Participant 7-“Pamhplet is only one of the ways; it cannot replace talking. Talks with nurse’s and doctor make huge difference. Two words of mine will be 10 words of anybody. I think that is how it should be. Anyway pamphlet is a good supplement.”
Discussion
This paper attempts to explore challenges to practice infection control measures in pulmonary TB among health care personnel in resource limited health care setting. Majority (58.5%) of the participants had good knowledge. A 74.1% participant had answered correctly in the area of personal protective equipment. Our findings suggested that knowledge regarding TB infection control practices among health care personnel should be 100%. Another nationwide study reported that 86.1% of the participants obtained a fair score (40.0%–69.0%) in assessing knowledge regarding TB infection control. Forty-seven of the respondents self-reported inappropriate practices [5]. In terms of knowledge regarding transmission, the majority of the participants correctly answered that TB can be transmitted through coughing and sneezing. This finding is in line with a study done in Bangladesh and Pakistan where most of the respondents answered that TB spreads through air droplets, coughing and sneezing [6]. On compliance of personal protective measures, 92 (71.3%) respondents reported that they used masks, of which 38.8% used the N95 respirators. The current study revealed that there was a specific written policy for hospital infection control but that does not include TB infection control policy. Environmental infection control measures were better than the personal protective measures as there were no adequate supply of mask (N 95) for the health care personnel. TB related information was not available in the facility for the patients. There was no documented training programme on TB for the health care personnel. Similar findings were reported in a study done in Ikeja LGA [7] and India where none of the health care facility out of 20 health care facility had written infection control policy for TB. Only 30% health care facility had reported to have a designated person for TB infection control practices. This study also aligns with the result of present study as 45% health care facility gave information to patient regarding TB prevention practices, cough etiquettes in terms of poster. Only 20% health care facility is observed to give mask for patients with cough [7,8]. In the present study there was no evident of fit test of N 95 mask as discussed in the focus group discussion. Concerns were also related to lack of space to separate the suspected patient with Pulmonary TB and regarding cost of the resources which is chargeable to the patient. The current study also expressed that there is disproportionate focus on personal protective equipment for the health care personnel. These findings were in harmony with a study done by Zelnic J et al., [9]. The qualitative study had categorized the findings related to TB infection control implementation in the setting into three domains. These are: 1) lack of resources; 2) distrust of infection control measures by health care personnel; and 3) a disproportionate focus on personal protective equipment specially respirators. Participants have expressed many difficulties to implement the policy as they have expressed that N95 mask is costly in many hospitals and opening window is difficult during cold weather. Also, many health care personnel were confused regarding N95 mask; although fit testing is required to ensure effectiveness of N95 but none was reported [9]. After the focus group discussion, during consequent visit, it was observed that all the staff in the ward were wearing N95 mask. It was also noted that doctors coming for rounds also started wearing N95 mask after participating in focus group discussion. In the ward and ICU; patients with suspected pulmonary TB were given surgical mask. All the participants expressed that effective communication with patient can have a great impact on their behaviour. It was also decided to develop a pamphlet and poster by the staff to educate patient and relatives on preventive practices for pulmonary TB. It was also observed that all health care personnel voluntarily comply with hand hygiene (nurses decided not to carry hand rub for other health care personnel). Compliance to the waste management improved significantly, for example biomedical waste bins were placed in the isolation rooms. It was also observed that housekeeping personnel’s started using N95 masks when they were inside isolation room with pulmonary TB patients. Although 5% phenol was not available in the settings, however 10% sodium hypochlorite was used to disinfect the sputum of pulmonary TB patients.
Reducing transmission of pulmonary TB will require strenuous efforts to improve case detection and initiate right infection control measures. Despite introduction of DOTs strategy, WHO TB control efforts towards reducing the transmission of TB [1], face significant challenges in many health care settings. Cost is one of the major barriers in resource limiting settings.
Conclusion
The current study explores the elements of hospital infection control practices in resource limited health care setting. Lowering transmission risk for pulmonary TB requires a combination approach centered on rapid identification of active TB cases and tuberculosis drug resistance, exploring available resources followed by rapid initiation of appropriate treatment and adherence support, complemented by universal TBIC (TB Infection Control) measures in healthcare facilities.