Bilateral Psammomatoid Ossifying Fibroma of Maxilla
Ruchika Ravi Agrawal1, Jyoti Dilip Bhavthankar2, Mandakini Subhash Mandale3, Abdul Ahad Khan4, Jayanti Humbe5
1 Post Graduate Student, Department of Oral Pathology, Government Dental College and Hospital, Dhanwantari Nagar, Ghati Campus, Aurangabad, Maharashtra, India.
2 Professor, Department of Oral Pathology, Government Dental College and Hospital, Dhanwantari Nagar, Ghati Campus, Aurangabad, Maharashtra, India.
3 Associate Professor, Department of Oral Pathology, Government Dental College and Hospital, Dhanwantari Nagar, Ghati Campus, Aurangabad, Maharashtra, India.
4 Lecturer, Department of Oral Pathology, Government Dental College and Hospital, Dhanwantari Nagar, Ghati Campus, Aurangabad, Maharashtra, India.
5 Associate Professor, Department of Oral Pathology, Government Dental College and Hospital, Dhanwantari Nagar, Ghati Campus, Aurangabad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ruchika Ravi Agrawal, Post Graduate Student, Department of Oral Pathology, Government Dental College and Hospital, Dhanwantari Nagar, Ghati Campus, Aurangabad-431001, Maharashtra, India.
E-mail: ruchikaagrawal26@gmail.com
Ossifying-Fibroma (OF) is a benign neoplasm histopathologically composed of fibrocellularstroma and variable amount of mineralized material. Generally, these tumours in jaw bones are found as solitary lesions. Occurrence of these tumours as Multiple Ossifying Fibromas (MOF) in jaw bones is very rare. The studies reported till now have found an association between MOF and Hyperparathyroid Jaw Tumour Syndrome (HPT-JT). HPT-JT is always associated with the genetic mutation in tumour suppressor gene HRPT2 which encodes protein parafibromin. The simultaneous presentation of ossifying fibroma and other features of HPT-JT may or may not be present. Thus, the expression of parafibromin needs to be evaluated in MOF to rule out it’s association with HPT-JT. The present case of 24 years old female patient, showed bilateral maxillary Psammomatoid Juvenile Ossifying Fibroma (PsJOF). The patient was further investigated for association with HPT-JT. Other finding such as blood serum calcium and parathyroid assay were normal. A negative expression of parafibromin in the tumour tissue suggested an association with HPT-JT. Thus, evaluation of parafibromin can help in accurate diagnosis and treatment of MOF of jaws.
Hyperparathyroid Jaw Tumour syndrome, Jaw, Multiple Ossifying Fibroma (MOF), Parafibromin
Case Report
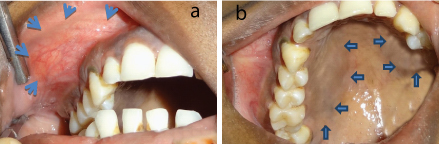
A 24-year-old female reported to the department of Oral Pathology with a chief complaint of an asymptomatic slowly progressive swelling on right side of face since 4 months. Initially swelling was small in size about 1 x 1 cm when patient noticed it and increased to the present size. Patient was well oriented with time, place and person. She was afebrile with no signs of pallor and blood pressure was 124/78 mm Hg. Extraoral examination revealed a well demarcated swelling over right side of maxilla [Table/Fig-1]. It was approximately 4.5 x 4 cm in size, bony hard in consistency with overlying skin normal in appearance. Right eye involvement with upward movement of eyeball was seen. Intraoral examination revealed an expansile, hard, non- tender swelling in maxillary right premolar-molar region causing obliteration of buccal vestibule and palatal expansion [Table/Fig-2a,b]. No extraoral signs were seen on left side of maxilla. A separate palatal expansion was noted on left side [Table/Fig-2b]. The swelling was slightly brownish in colour.
Swelling on right side midface region. Upward movement of right eyeball.

a) Obliteration of right buccal vestibule; b) Right side -Buccal and palatal cortical plate expansion. Left side- Palatal cortical plate expansion.
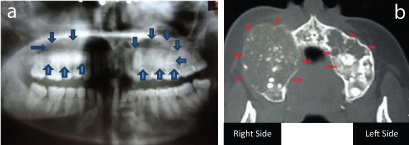
A panoramic radiograph showed large, well demarcated, mixed radiolucent-radioopaque lesion in the right posterior maxilla. Incidentally, a contralateral well circumscribed radiolucency with variable degrees of calcification was found involving the region of 23 to distal of 27 [Table/Fig-3a]. Cone Beam Computed tomography revealed unilocular and hypodense image with radio-opaque areas associated with right maxilla. The right side lesion extended anteroposteriorly from canine upto maxillary tuberosity, superiorly into Lower 2/3rd of maxillary sinus and inferiorly into alveolus with roots of 13, 14, 15, 16 and 17 extending into lesion. Thinning of palatal plate was noted. Expansion and destruction of buccal cortical plate were also seen. The other lesion located on left maxilla also showed hypodense areas with internal dense opacities suggesting osteoid formation. The left side lesion extended from 23 to 27 and superiorly into lower 2/3rd of maxillary sinus and inferiorly into the alveolus [Table/Fig-3b]. The results of blood chemistry (Serum Calcium, Serum Parathyroid hormone levels) of the patient were within normal limits. Provisional Diagnosis of OF and fibrous dysplasia was given based on clinical features. Radiographically, Fibrous dysplasia and ossifying fibroma were taken into consideration. Differential Diagnosis of OF and fibrous dysplasia and desmoplastic ameloblastoma was given.
a) OPG shows mixed radiolucent-radiopaque swelling in posterior maxilla bilaterally; b) CBCT showing cortical expansion bilaterally.
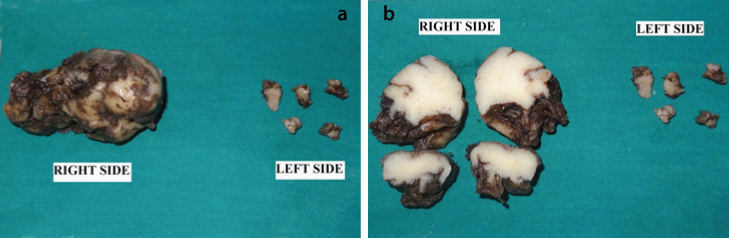
Surgical exploration revealed large bony hard lesions, well demarcated from surrounding bone. Both the tumours were surgically enucleated with curettage and submitted for histopathological examination. On Gross examination, tumours were creamy white in colour with a gritty consistency [Table/Fig-4a,b].
a) Gross tissue showing creamy white appearance; b) Cut surface show gritty consistency.
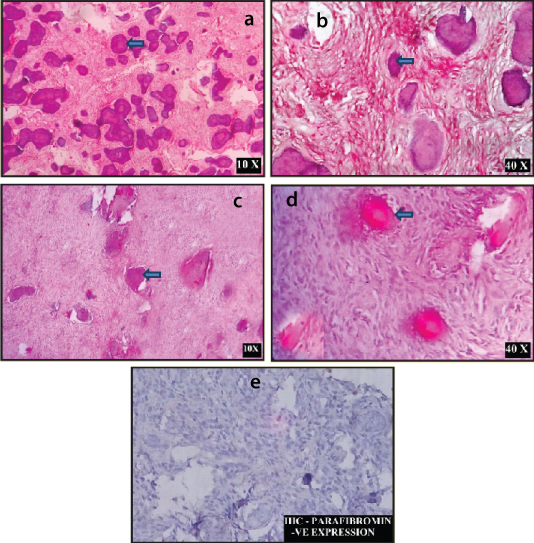
Histopathological examination showed a hypercellular stroma with bland fibroblast and minimal extracellular collagen deposition. No mitotic activity was seen. Numerous irregular and spherical ossicles were seen interspersed between the fibroblastic cells. These ossicles exhibited varying degrees of calcification. These psammoma bodies like ossicles were acellular with a concentric lamination [Table/Fig-5a-d]. The section was also subjected for immunohistochemical analysis with parafibromin and ki67. Parafibromin was negative [Table/ Fig-5e].
Haematoxylin and Eosin Stain: a) 10X; b) 40X; c) 10X; and d) 40X. Psammoma like ossicles seen in bland fibroblastic connective tissue stroma. e) Immunohistocemical staining for Parafibromin is negative
Correlation of clinical, radiographic and histopathological features of both the maxillary lesions supported a diagnosis of PsJOF. No postoperative complications were present and there was no sign of recurrence at one year of follow up [Table/Fig-6].
Postoperative photograph of the patient.

Permission was obtained from patient for publication of images.
Discussion
Benign Fibro-osseous lesions (BFOLs) are group of bone disorders that share similar histologic features. In these lesions, normal bone is replaced by tissue containing collagen and fibroblast with varying amounts of mineralized substance. This mineralized substance may be bone or cementum like in appearance [1]. Ossifying Fibroma (50.8 %), Fibrous Dysplasia (42.6%) and Osseous Dysplasia (6.6%) are the most common BFOLs [2]. OF is well circumscribed and composed of fibrocellular tissue and mineralized material [3]. Occurrence of MOF is very rare in the jaws. Till date, out of 13 cases of MOF of jaw bones, only one case presented as Psammomatoid Juvenile Ossifying Fibroma (PsJOF). PsJOF is an aggressive variant of OF that is more common in extragnathic craniofacial bones involving periorbital, frontal and ethmoid bones, often as solitary lesions with infiltrative growth pattern. This case report presents a second case of bilateral PsJOF of maxilla [4]. Considering the association of MOF with Hyperparathyroid Jaw Tumour Syndrome (HPT- JT), the present case was investigated for HPT-JT. Serum Parathyroid and serum Calcium levels were normal. IHC evaluation was negative for Parafibromin. It was positive for Ki67 (>20%).
Juvenile Ossifying Fibroma (JOF) is benign, potentially aggressive fibro-osseous lesions of the craniofacial bone with infiltrative growth pattern. It has a higher incidence in children and young adults, having predilection for males [5]. Based on the difference in the age of occurrence, Thankappan S et al., classified JOF into 2 types – JOF-WHO type and JOF-PO (Psammoma like ossicles type) [6]. Based on histologic criteria and predilection for specific age groups, Mofty categorized the juvenile ossifying fibroma into – trabecular JOF (TrJOF) and PsJOF. The average age range of occurrence of TrJOF is 81/2 - 12 year. The age of occurrence for PsJOF is 16-33 years [7].
Around 75% of PsJOF occur in the orbit, paranasal sinuses and calvaria while merely 25% encompass the maxilla or mandible [8]. Present case in a 24-year-old female involving both the maxillae exhibited characteristic feature of PsJOF.
JOF occur as an asymptomatic bony hard swelling. The extent and the duration of the swelling depend on the site and aggressiveness of the lesion [6]. Radiographically the lesion may be radiolucent, radio-opaque or mixed in appearance.
Microscopically, the PsJOF characteristically shows a fibrocellular stroma containing small ossicles resembling psammoma bodies. Psammoma is derived from Greek word ‘psammos’ meaning sand. The stroma range from being loose and fibroblastic to predominantly cellular with less intervening collagen. For smaller lesions, simple excision with adjacent marginal bone and, for larger lesions, more aggressive surgical treatment is done. Recurrence rate range from 30-60% [5,6].
OF usually present as a solitary lesion and rarely as multiple lesions. The aetiology and pathogenesis for both remain unknown. Solitary lesion and multiple lesions represent different clinical presentations of same pathology as they both show similar clinical, radiologic and histopathologic features. Some systemic conditions like Hyperparathyroid Jaw Tumour Syndrome (HPT-JT) are associated with recurrent or MOF of the jaws especially in young patients [4]. HPT-JT is an inherited autosomal dominant disorder. It is characterized by the occurrence of parathyroid adenoma or carcinomas, Wilm’s tumour, fibro-osseous lesions of the jaws, renal cyst, renal hamartoma, renal cortical adenomas, papillary renal cell carcinoma, pancreatic adenocarcinoma and testicular tumours [3,9]. Inactivation of HRPT2 gene is associated with the pathogenesis of hereditary HPT-JT. The gene HRPT2 encodes for parafibromin. Parafibromin has tumour suppressor activity along with repression of cyclin D1 and inhibition of c-myc proto-oncogene. It also activates the Wnt signaling through interaction with B catenin in dephosphorylated form with increased cell proliferation. This gene mutation leads to decreased parafibromin expression and an increase in cell proliferation. This further can be confirmed by genetic mutational analysis of HRPT2 gene [10,11]. Hypercalcaemia and high PTH levels with ossifying fibromas have been reported only in 25-50% of HPT-JT cases which means that there may be cases of HPT-JT where serum levels of calcium and phosphate may remain normal [1]. In the present case, serum Calcium and serum PTH hormone levels were within normal limits; Serum PTH- 30pg/ml and Serum Calcium- 9mg/dl. But the loss of nuclear expression of parafibromin suggested HRPT2 mutation.
In the literature review of cases of HPT-JT with jaw ossifying fibromas, out of 24 cases, 16 cases were solitary lesions and 8 cases were multiple lesions [Table/Fig-7] [12-19]. The suggested treatment for HPT-JT associated OF is enucleation with parathyroid gland resection which prevents recurrence [1], whereas for sporadic cases, enucleation of the tumour is only required. Hence, the differential diagnosis of OF associated with HPT-JT from sporadic OF is important for treatment and prognosis. Thus the clinicians should be aware of the possibility of HPT-JT in young patients with OF, because this disease is usually associated with recurrent or multiple OFs of the jaws requiring more aggressive treatment and proper follow up protocol. The literature regarding the clinical features and origin of multiple OF’s is very scarce and controversial. It is thought to arise from the periodontal ligament, which contains multipotential cells. The significance of this topic depends on the probable association with HPT-JT which in turn is related with additional abnormalities in other organs including malignant tumours and systemic findings.
Cases of Multiple ossifying fibroma affected with HPT-JT in the literature [12-19].
| Sr. no | Author | Age/Gender | Location |
|---|
| 1 | Teh BT et al., [12] | 54/M | Lesion 1. MandibleLesion 2. Maxilla |
| 2 | Mallette LE et al., [13] | 17/N.S* | Lesion 1. MandibleLesion 2. Hard palate |
| 3 | Schmidt BP et al., [14] | 37/M | Lesion 1. Right maxillary canine and premolar areaLesion 2. Left maxillary canine and premolar areaLesion3. Left mandibleLesion 4. Right mandible |
| 4 | Szabo J et al., [15] | 22/M | Lesion 1. Right MaxillaLesion 2. In the right mandible |
| 5 | Howell VM et al., [16] | 16/M | Lesion 1. Right MandibleLesion 2. Right Mandible |
| 6 | Aldred MJ et al., [17] | 22/M | Lesion 1. The right mandibleLesion 2. The left mandible |
| 7 | Fujikawa M et al., [18] | 22/F | Lesion 1. Left maxillaLesion 2. Left mandibleLesion 3. Right Mandible |
| 8 | Cavaco BM et al., [19] | 13/F | Lesion 1. MaxillaLesion 2. Mandible |
*N.S- Not stated
Thus, grounded on clinical, radiographic, histopathologic, immunohistochemistry and laboratory findings, diagnosis of Syndrome associated Psammomatoid Juvenile Ossifying fibroma was done.
Conclusion
Juvenile Ossifying Fibroma is an aggressive tumour that may or may not be associated with HPT-JT. Hyperparathyroid Jaw tumour syndrome may not always show altered blood chemistry. Thus patients with multiple ossifying fibroma should always be evaluated by Immunohistochemistry for its association with HPT-JT. Early diagnosis of HPT-JT may help in identifying and treating other tumours associated with HPT-JT.
*N.S- Not stated
[1]. Wan TT, Zhang R, Wang L, Chen Y, Dong Q, Li TJ, Two cases of multiple ossifying fibromas in the jawsDiag Pathol 2014 9:7510.1186/1746-1596-9-7524678936 [Google Scholar] [CrossRef] [PubMed]
[2]. Tayfur M, Kadioglu E, Balci MG, Deger AN, Cimen FK, Daltaban F, Bilateral Synchronous ossifying fibromasof the mandible: A case reportInt J Clin Exp Pathol 2015 8(5):5844-47. [Google Scholar]
[3]. Riberio ACP, Carlos R, Diaz KP, Vargas PA, Bilateral central ossifying fibroma affecting the mandible: report of an uncommon case and critical review of the literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2011 111:e21-e26.10.1016/j.tripleo.2010.10.02421237424 [Google Scholar] [CrossRef] [PubMed]
[4]. Popli DB, Desai R, Bansal S, Andrade NN, Bilateral Psammomatoid ossifying fibroma: a case report and review of the literatureJ Oral MAxillofac Surg 2013 71:714-20.10.1016/j.joms.2012.10.01023245519 [Google Scholar] [CrossRef] [PubMed]
[5]. Malathi N, Radhika T, Thamizhchelvan H, Ravindran C, Ramkumar S, Giri G, Gopal D, Psammomatoid Juvenile Ossifying Fibroma of the jawsJOMFP 2011 15(3):326-29.10.4103/0973-029X.8671022144839 [Google Scholar] [CrossRef] [PubMed]
[6]. Thankappan S, Nair S, Thomas V, Sharafudeen KP, Psammomatoid and Trabecular variants of JOF- Two case reportsIJRI 2009 19:116-19.10.4103/0971-3026.5083219881065 [Google Scholar] [CrossRef] [PubMed]
[7]. El-Mofty S, Psammomatoid and trabecular juvenile ossifying fibroma of the craniofacial skeleton: Two distinct clinicopathologic entitiesOral Surg Oral Med Oral Pathol Oral Radiol Endod 2002 93:296-304.10.1067/moe.2002.12154511925539 [Google Scholar] [CrossRef] [PubMed]
[8]. Barnes L, Everson WJ, Reichart P, Sidransky D, WHO classification of tumours-Pathology and Genetic-Head and Neck tumours 2005 FranceIARC press [Google Scholar]
[9]. Cavaco BM, Barros L, Pannett AAJ, Ruas L, Carvalheiro M, Ruas MMA, The Hyperparathyroidism jaw tumour syndrome in a Portuguese kindredQ J Med 2001 94:213-22.10.1093/qjmed/94.4.21311294964 [Google Scholar] [CrossRef] [PubMed]
[10]. Netto AC, Gomez RS, Diniz MG, Silva TF, Campos K, Marco LD, Assessing the contribution of HRPT2to the pathogenesis of jaw fibrous dysplasia, ossifying fibroma, and osteosarcomaOral Surg Oral Med Oral Pathol Oral Radiol 2013 115(3):359-67.10.1016/j.oooo.2012.11.01523453027 [Google Scholar] [CrossRef] [PubMed]
[11]. Zhang M, Li Q, Zhang L, Fu R, Wang Y, Chen S, Identification of a germline mutation in the HRPT2 gene in a chinese family with parathyroid carcinomasIRDR 2012 1(1):27-29.10.5582/irdr.2012.v1.1.2725343069 [Google Scholar] [CrossRef] [PubMed]
[12]. Teh BT, Farnebo F, Kristoffersson U, Sundelin B, Cardinal J, Axelson R, Autosomal dominant primary hyperparathyroidism and jaw tumour syndrome associated with renal hamartomas and cystic kidney disease: linkage to 1q21-q32 and loss of the wild type allele in renal hamartomasJ Clin Endocr Metab 1996 81:4204-11.10.1210/jcem.81.12.89540168954016 [Google Scholar] [CrossRef] [PubMed]
[13]. Mallette LE, Malini S, Rappaport MP, Kirkland JL, Familial cystic parathyroid adenomatosisAnn Int Med 1987 107:54-60.10.7326/0003-4819-107-1-543592449 [Google Scholar] [CrossRef] [PubMed]
[14]. Schmidt BP, Bradrick JP, Gabali A, Hyperparathyroidism-jaw tumour syndrome: a case reportJ Oral Maxillofac Surg 2009 67:423-27.10.1016/j.joms.2008.07.01519138622 [Google Scholar] [CrossRef] [PubMed]
[15]. Szabo J, Heath B, Hill VM, Jackson CE, Zarbo RJ, Mallette LE, Hereditary hyperparathyroidism-jawtumour syndrome: the endocrine tumour gene HRPT2 maps to chromosome1q21-q31Am J Hum Genet 1995 56:944-50. [Google Scholar]
[16]. Howell VM, Zori RT, Stalker HJ, Williams C, Jesse N, Nelson AE, A molecular diagnosis of hyperparathyroidism—jaw tumour syndrome in an adolescent with recurrent kidney stonesJ Pediatr 2004 145:56710.1016/j.jpeds.2004.04.02315480389 [Google Scholar] [CrossRef] [PubMed]
[17]. Aldred MJ, Talacko AA, Savarirayan R, Murdolo V, Mills AE, Radden BG, Dental findings in a family with hyperparathyroidism jaw tumour syndrome and a novel HRPT2 gene mutationOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:212-18.10.1016/j.tripleo.2005.06.01116448924 [Google Scholar] [CrossRef] [PubMed]
[18]. Fujikawa M, Okamura K, Sato K, Mizokami T, Tamaki K, Yanagida T, Familial isolated hyperparathyroidism due to multiple adenoma as associated with ossifying jaw fibroma and multiple uterine adenomyomatous polypsEurn J Endocrinol 1998 138:557-61.10.1530/eje.0.13805579625369 [Google Scholar] [CrossRef] [PubMed]
[19]. Cavaco BM, Guerra L, Bradley KJ, Carvalho D, Harding B, Oliveira A, Hyperparathyroidism-jaw tumour syndrome in Roma families from Portugal is due to a founder mutation of the HRPT2 geneJ Clin Endocr Metab 2004 89:1747-52.10.1210/jc.2003-03101615070940 [Google Scholar] [CrossRef] [PubMed]