Large Placenta and Small Foetus at Early Gestation Predicts Foetal Growth Restriction due to Placental Dysmorphology
Vidyashree Ganesh Poojari1, Akhila Vasudeva2, Jyothi Shetty3, Ranjini Kudva4, Divya Solipuram5
1 Assistant Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Professor and Unit chief, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
3 Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
4 Professor, Department Pathology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
5 Senior Resident, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Akhila Vasudeva, Professor and Unit chief, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal-576104, Karnataka, India.
E-mail: akhilavasudeva@gmail.com
When placenta appears large on ultrasound, there are certain differential diagnoses to be kept in mind. We present a series of three cases in which large placenta was observed in first trimester scan. All three pregnancies resulted in Foetal Growth Restriction (FGR) associated with placental morphological abnormality.
Chorangiosis, Partial mole, Placental Mesenchymal Dysplasia, Placentomegaly
Introduction
It seems beneficial to subjectively look for placental size and morphology in the first trimester scan. Placental Dysmorphology (PMD) is an important cause of early onset of Foetal growth restriction. PMD is a rare (incidence 0.02%) placental vascular anomaly as described by Moscoso et al., in 1991. However, many healthcare providers are unfamiliar with the clinical entity hence under-diagnosed or under reported [1].
Case 1
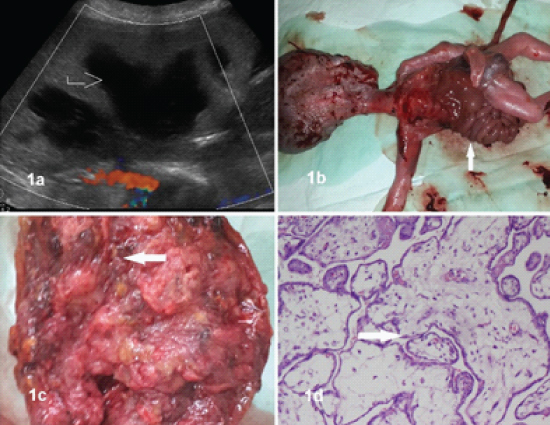
A 23-year-old primigravida was referred with early onset FGR at 21 weeks. She was normotensive, clinical examination revealed uterine height less than the period of gestation. Her medical history and family history were unremarkable. Ultrasound showed unusually large placenta, with multiple lakes of blood with low velocity/absent flow within [Table/Fig-1a] and cob web appearance. Gross oligoamnios severely compromised the anatomical survey. Maternal evaluation, revealed active SLE and hypothyroidism, for which treatments were begun. β-HCG was 19,415 μIU/mL. However, growth curves flattened and doppler studies worsened. She developed severe preeclampsia at 28 weeks. Unfortunately, Foetal demise occurred at 29 weeks. She had induced vaginal expulsion. Foetus had large gastroschisis, widely separated bony chest, large head and exophthalmos [Table/Fig-1b,c]. Histopathology confirmed placental mesenchymal dysplasia [Table/Fig-1d]. Immunohistochemistry showed Desmin-positivity. Unusually, our case of PMD was associated with active maternal SLE along with unusual Foetal anomalies. Couple refused autopsy. Foetal karyotype was normal.
(1a) large placenta, with multiple lakes of blood as marked in arrow; (1b) Arrow showing expelled fetus showing multiple fetal malformation; (1c) Arrow showing placenta with vesicles and dilated tortuous vessels; (1d) Arrow showing enlarged chorionic villi, loose myxoid strom, (H and E X100)
Case 2
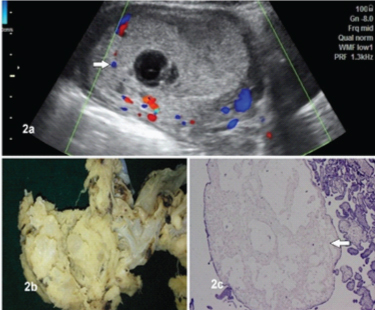
A 21-year-old primigravida was referred at 19 weeks with gross oligohydramnios and unusually large placenta. History was unremarkable for maternal infections like toxoplasmosis, cytomegalovirus or syphilis. There was no family history of diabetes mellitus. Examination was not suggestive of early Preterm Prelabor Rupture Of Membrane (PPROM). Ultrasound showed large globular placenta with homogenous echotexture, multiple lakes and sinuses [Table/Fig-2a]. No structural anomalies were found. β-HCG was 110,660 μIU/ml. Cytomegalovirus (CMV) IgM/ IgG was negative. ANA Profile was negative. Patient underwent medical termination of pregnancy. Placental Histopathology was consistent with placental mesenchymal dysplasia [Table/Fig-2b,c]. Post abortion β-HCG came back to normal.
(2a) Ultrasound image showing large globular placenta with homogenous echo texture, multiple lakes and sinuses; (2b) Placenta with cord attached;(2c) Arrow showing enlarged and hydropic stem villi with cistern (H and E X100)
Case 3
A 32-year-old primigravida, presented at 19 weeks with severe early onset FGR. Uterus corresponded to 16 week size. Medical and family history was unremarkable. USG showed large homogenous placenta occupying most of the uterus, multiple large sinuses [Table/Fig-3a,b]. Karyotype was normal. Infection screen negative and no structural anomalies found. No GDM, anaemia or preeclampsia. ANA was weakly positive. Foetal demise occurred at 23 weeks. She had induced vaginal expulsion. Autopsy revealed dysmorphic features including hypertelorism, short nose, long philtrum, micrognathia, short great toes and overriding of the toes. Placental histopathology revealed Chorangiosis [Table/Fig-3c].
(3a) USG showing large homogenous placenta as marked by arrow; (3b) Arrow showing placenta with multiple large sinuses; (3c) Arrow showing microscopic picture of >10 capillaries in the villous. (H and E X 100)

Discussion
Congenital malformation of the mesoderm, molecular disruption of the imprinting genes of chromosome 11p15.5 associated with Beckwith-Wiedemann Syndrome (BWS) and Androgenetic/Biparental mosaicism are some of the theories explained for this condition [1]. PMD is associated with BWS in 25%, FGR in 50%, and IUFD/neonatal death in 43%; but can also be associated with normal appearing Foetuses. PMD disproportionally affects females [1]. About 52% deliver preterm, either due to medical reasons or due to spontaneous preterm labor. Nine percent are associated with maternal complications like gestational hypertension, preeclampsia, eclampsia and HELLP syndrome. Uneventful pregnancies are rare [2]. [Table/Fig-4] compares various published articles on placentomegaly against the present study [1-3].
Summary of published literature on the outcome of pregnancies complicated by placental dysmorphology on USG [1-3].
| Published articles | No of cases | Ultrasound diagnosis | Hormone levels | Maternal problems | Foetal problems | Placental HPE |
|---|
| Nayeri UA et al., [2],systematic review | 61 | Cystic placenta (80%)Enlarged thickened placenta (50%)Dilated chorionic vessels (16%)Fetal anomaly (38%) | Elevated β-HCG (38%)Elevated msAFP (70%) | Preterm delivery (52%)PPROM (17%)PE/ Eclampsia/ HELLP/ GHTN- (9%) | TOP (19%)FGR (33%)IUFD (13%)Abnormal genetic evaluation (28%)BWS (19%)Uncomplicated pregnancy (9%) | Suspected PMD but not confirmed by HPE |
| Martinez-Payo C et al., [3] | 1 | At 21wk, FGR, placentomegaly, severe oligohydramnios, normal uterine, umbilical, ductus venosus flow, cerebellar hematoma in fetus | PAPP-A 0.3MoM,β-HCG- 0.9MoM | Gestational hypertension, TORCH negative | Karyotype 46XXFoetal demise at 27 weeks | PMD |
| Gerli S et al., [1], | 1 | At 10 wks, “mounted in snow” trophoblastic tissue.At 23 wks, placentomegaly with multiple anechoic areas, FGR. | β-HCG- 110.45mIU/ml. | Nil | CVS- normal. Foetal demise at 31 wks.Foetal karyotype- normal | PMD |
| Present study | 3 | Placentomegaly, multiple lakes, early onset FGR | β-HCG- normal | PE, SLE | Foetal demise at 29 wk, | PMD |
| Severe oligohydramnios, large placenta, no structural abnormalities | High β-HCG | CMV/ANA- negative | Foetal demise | PMD |
| Early onset FGR, large homogenous placenta | - | ANA weakly positive | Karyotype normal.Foetal demise at 23 wks | Chorangiosis |
NS- Nil Significant, CVS- Chorionic Villous Sampling, TOP- Termination Of Pregnancy, β-HCG- Beta- Human Chorionic Gonadotropins, IUFD- Intra Uterine Fetal Demise, Msafp- Maternal Serum Alphafeto Protein, PE- Preeclampsia, GHTN- Gestational Hypertension.
These are the differential diagnosis to be kept in mind when PMD is suspected- partial molar pregnancy, complete mole with co-existing normal Foetus, chorangioma, subchorionic hematoma, confined placental mosaicism and spontaneous abortion with hydropic changes [2]. Since the sonographic features of PMD are very similar to those of partial moles-enlarged, thickened placenta with cystic spaces, PMD is often mistaken for molar pregnancy. PMD is associated with low velocity blood flow in the placental lesion and normal or slightly high β-HCG which returns to normal after delivery whereas partial mole is associated with high velocity blood flow and high β-HCG levels, often >100,000 μIU/mL. It is important to distinguish PMD from partial mole especially in the presence of normal appearing Foetus; as this would influence important decisions including termination of pregnancy. Elevated maternal serum Alfa-fetoprotein is associated with PMD in 70% of the cases. Confirmation of the normal karyotype should be performed by either chorionic villous sampling or amniocentesis to exclude partial molar pregnancy [4]. Partial molar pregnancies demonstrate triploidy, which is extremely rare in PMD.
Chorangiosis is a rare placental vascular abnormality involving predominantly the terminal villi. Here there are >10 terminal villi containing more than 10 capillaries per villous in 10 medium power fields and this pattern is seen in multiple areas (at least 3) of placenta. Chorangiosis has been associated with hypoxia in placental tissue, thereby increasing the risk of adverse pregnancy outcome. There is a higher incidence of Foetal anomaly, FGR and Foetal death. Chorangiosis is often seen in many maternal medical illnesses resulting in placental hypoxia [5]. Several obstetric complications and outcomes like perinatal deaths, maternal diabetes mellitus, chronic infection, umbilical cord problems, congenital anomalies, Foetal vascular thrombosis and multiple pregnancies are related to Chorangiosis.
Placentomegaly may be associated with adverse pregnancy outcome. Diagnosis of PMD/ Chorangiosis should be considered with specific sonological findings like enlarged, cystic placenta with dilated chorionic vessels. Detailed anatomical survey is a must to rule out Foetal anomalies. Doppler, β-HCG levels and Alpha-feto protein help us to distinguish between PMD and partial mole [6]. In addition to Foetal karyotype, it is worthwhile considering genetic testing to rule out BWS, if sonological features are suspicious of PMD. Patients should be counselled regarding complications such as Foetal growth restriction, intrauterine Foetal demise and preterm delivery. Serial growth scan and assessment of Foetal well-being in the third trimester is of utmost importance. Foetal autopsy is always advised. Placenta should be sent for pathological evaluation after delivery for confirmation of the placental pathology. Histopathological confirmation helps to know the exact diagnosis, recurrence of the condition, counselling of the couple as well as placental survey from first trimester itself in future pregnancy. Around 15% of PMDs are familial and theoretically there is a small recurrence risk in these families, but a follow-up study of five years for PMD showed no signs of trophoblastic disease or recurrence of PMD in the next pregnancies [4].
Conclusion
A large placenta seen in first trimester ultrasound should alert the obstetrician towards the possibilities of several above mentioned feto-maternal complications. Placental dysmorphologies including PMD should also be kept in mind. Parents should be alerted about the likelihood of conditions including growth restriction, intrauterine death and BWS associated with PMD. However, careful observation and follow-up ultrasounds help in diagnosing the Foetal and placental pathology. As majority of the Foetuses are phenotypically and morphologically normal, unnecessary termination of pregnancy should be avoided.
NS- Nil Significant, CVS- Chorionic Villous Sampling, TOP- Termination Of Pregnancy, β-HCG- Beta- Human Chorionic Gonadotropins, IUFD- Intra Uterine Fetal Demise, Msafp- Maternal Serum Alphafeto Protein, PE- Preeclampsia, GHTN- Gestational Hypertension.
[1]. Gerli S, Giordano C, Del Sordol R, Fratini D, Di Renzo GC, Early ultrasonographic diagnosis of placental mesenchymal dysplasiaEur Rev Med Pharmacol Sci 2014 18(17):2419-23. [Google Scholar]
[2]. Nayeri UA, West AB, Grossetta HK, Copel JA, Sfakianaki AK, Systematic review of sonographic findings of placental mesenchymal dysplasia and subsequent pregnancy outcomeUltrasound Obstet Gynecol 2013 41(4):366-74.10.1002/uog.1235923239538 [Google Scholar] [CrossRef] [PubMed]
[3]. Martinez-Payo C, Bernabeu RA, Villar IS, Goy EI, Intrauterine growth restriction associated with hematologic abnormalities: probable manifestations of placental mesenchymal dysplasiaAm J Perinatol Rep 2015 5(2):e85-e88. [Google Scholar]
[4]. Adelaide C, Joana C, Barbara F, Graca R, Olimpia C, Placental mesenchymal dysplasia- Review articleActa Obstet Gynecol Port 2015 9(3):235-40. [Google Scholar]
[5]. Jerzy S, Chorangiosis of chorionic villi. What does it really mean?Arch Pathol Lab Med 2016 140(6):588-93.10.5858/arpa.2015-0160-OA27232351 [Google Scholar] [CrossRef] [PubMed]
[6]. Minakshi R, Sujata S, Vanita J, Raje N, Placentomegaly and placental mesenchymal dysplasiaBMJ Case Reports 2012 2012:piibcr201200777710.1136/bcr-2012-00777723266781 [Google Scholar] [CrossRef] [PubMed]