Periodontal diagnosis and treatment plan rely on an important aspect which is called as the periodontal probing. The gold standard in determining an individual’s healthy periodontium is based on clinical parameters like Probing Pocket Depth (PPD) and Clinical Attachment Level (CAL) that are determined by periodontal probing [1].
In periodontal practice, the first encounter between the patient and periodontist is usually a periodontal examination. Periodontal examination consists of probing which is an essential part of examination and can elicit dental pain, anxiety and fear in patients. Hence it is important for a periodontist to understand each and every patient’s attitude towards dental treatment as it can adversely affect the diagnosis of gingival and periodontal diseases [2-5].
Pain as a symptom can discourage patients for diagnosis and treatments such as probing and scaling which can result to progression of periodontal disease [6].
Quantification of pain is relatively a difficult step as it may be associated with either physical or psychological factors. Studies have shown that use of Visual Analogue Scale (VAS) for assessment of pain is simple and reliable [7]. In an effort to eliminate pain on periodontal probing and thereby improving patient’s comfort and approach towards dental care various forms of anaesthesia were used. Injection type of anaesthesia is a conventional remedy but it has its own limitations like prolonged duration of action and anaesthetizing unwanted areas. Various topical anaesthetics in the form of gels, sprays and ointments were also used but the limitation is due to their physical properties like more flow, less retainability in pocket and lack of adequate duration time [8,9]. To overcome this, currently EMLA (Eutectic Mixture of Local Anaesthesia which is 25mg/g Lidocaine and 25 mg/g Prilocaine) is being used as intrapocket anaesthesia [10-14]. Apart from this there are other anaesthetic agents used such as Lidocaine 10% and Benzocaine 20%. However, EMLA has its own limitations like it is known to induce methemoglobinemia in some patients and it is also contraindicated in some cardiac patients and moreover it is quite expensive. Lidocaine and Benzocaine were effective at higher concentrations. Hence, an anaesthetic gel with less concentration and cost effective, ones which can be used in daily dental practice so far is not known. Lox 2% gel (Lidocaine 2%) is cost effective and the concentration of the drug being less if found effective can be used in our regular clinical practice.
The aim of the study was to evaluate the efficacy of 2% LOX Vs Placebo as an intrapocket anaesthesia to reduce pain on periodontal probing using a True Pressure Sensitive probe in patients with untreated chronic periodontitis patients.
Materials and Methods
This study was a randomized, double-masked, split mouth clinical trial comparing the efficacy of anaesthetic gel (LOX 2%) and placebo in a group of untreated chronic periodontitis patients using a TPS. Ethical clearance was obtained from the institutional ethical committee. Out of 28 patients 20 agreed to take part in the study. All patients were explained regarding the procedure to be done and the possible benefits associated with the study. The study was started in June 2017 and was completed in December 2017 (6 months).
Twenty participants (12 males and 8 females) with age range of 20 to 70 years (mean age 35.2+2.55years) were recruited who were referred to the Department of Periodontology, Sree Sai Dental College and Research Institute, Srikakulam, Andhra Pradesh. Taking into consideration, confidence interval and acceptable β error the power of the study was calculated and estimated as 80%.
Patients with atleast one tooth in each quadrant with a probing depth of >5mm were included. The study was conducted in a split mouth design. The patient was informed prior to the study that he/she is being given anaesthetic gel on all sites before probing. As VAS pain scores were recorded for test and placebo gel within the same patient, the bias has been avoided. Initially, the patient was examined in the out-patient department for periodontal disease who were then informed about the study and a written consent was taken from the patients. Since the patient was informed about the application of anaesthetic gel before probing the apprehension towards pain while probing may be eliminated. Patients should not have undergone any periodontal therapy prior to the study.
Patients who were excluded from the study were: patients suffering from any psychiatric disorders, those requiring prophylactic antibiotics before periodontal probing, patients who were under medications such as non-steroid anti-inflammatory drugs, individuals reporting allergies to dental anaesthetics, female patients who were pregnant or lactating, patients who had acute periodontal pain, pulpitis, abscesses, or other acute infections.
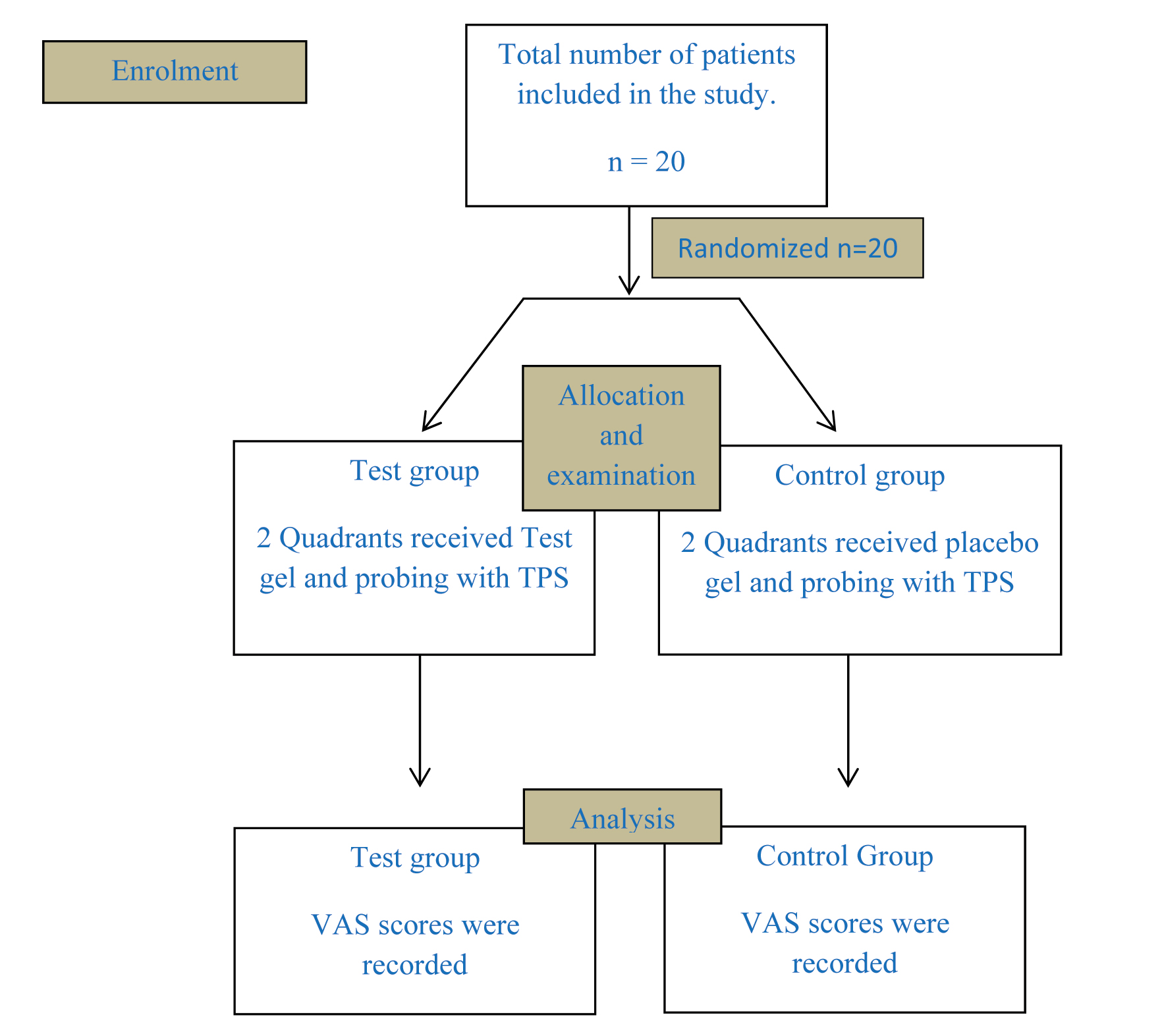
The study was carried out by two examiners, examiner 1(DD) performed the screening evaluation which included routine case history (chief complaint, past medical history, past dental history, oral hygiene status, extra oral and intra oral examination). Patients who were diagnosed with chronic periodontitis were allocated to the study and the sites for application of Cartridge 1 (C1) or Cartridge 2 (C2), were decided based on simple random method of randomization [Table/Fig-1]. Since we have included sites with similar probing depth for application of both test gel and placebo we have used simple randomization method. Examiner 2 (SSVP) performed the test probing. Both examiner 1 and examiner 2 were blinded to the study. The study was conducted in a split mouth manner with one side of the mouth receiving test gel and the other side of the mouth receiving placebo. Test gel was Lox 2% jelly (Lidocaine 2%) NEON laboratories. Placebo was formulated in Andhra University (School of Pharmaceuticals), Visakhapatnam, Andhra Pradesh. Excepting the anaesthetic ingredient the placebo gel contained Methylparaben, Propylparaben, purified water and a water based jelly in order to obtain the same physical characteristics like the anaesthetic gel [Table/Fig-2].
Consort flow diagram showing a detailed description of the present trial.
Armamentarium used for the trial – Placebo, LOX 2% jelly, C1 and C2 cartridges, Visual analogue scale, mouth mirror and True pressure sensitive probe.
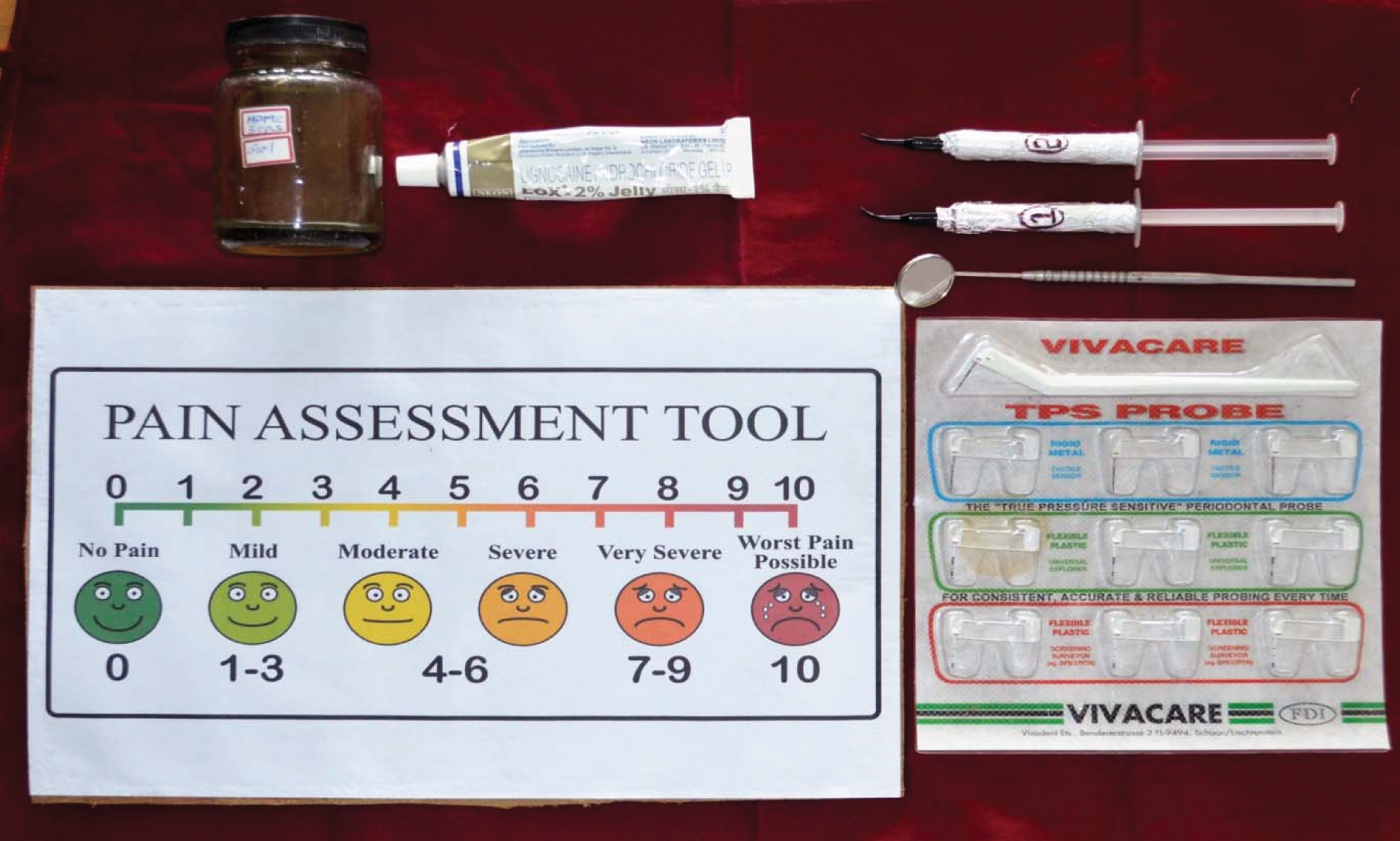
A third party (SBP) who was not involved in the study randomly allocated test gel and placebo in either of the cartridges C1 or C2 with respective sides [Table/Fig-3,4]. Probing was performed using a VIVACARE True Pressure Sensitive probe [Table/Fig-5,6]. Most of the studies used manual probes while probing in-order to reflect the conditions applicable to private practice. However, use of manual probes may produce excessive probing force i.e. >25g which may result in bias. In order to overcome this, in the present study we used a pressure sensitive probe to avoid excessive probing force caused by the use of a routine manual probe and also to standardize probing force. Post isolation, C1 and C2 were randomly allocated to either side. The patient was unaware of the composition of C1 and C2. The gels were applied and left in situ for 30 seconds. Eventually, probing was performed and pain assessment was done using a Visual Analogue Scale. The patient was asked to rate the pain from ‘0’ (indicating no pain) to ‘10’ (worst pain). The procedure was continued on the other side of the patient in a similar manner. The visual analogue scores for C1 and C2 were recorded and analysed.
Application of C1 gel with respect to third quadrant after isolation.

Application of C2 gel with respect to fourth quadrant after isolation.

Probing performed with TPS probe in third quadrant.

Probing performed with TPS probe in fourth quadrant.

Statistical Analysis
Statistical analysis was done using Mann-Whitney U test for comparing the VAS scores for C1 and C2. The mean probing depth was compared by Paired t-test. The software package used for the analysis was SPSS version 23.0 for Windows. All results were considered significant at p<0.05.
Results
Demographic Variables
A total of 20 individuals participated in the study with the mean age group included was 35.2±2.55years [Table/Fig-7]. Out of all the participants12 were males and 8 were females.
(Patient demographics) Demographic details of the patient.
| Value | Range |
|---|
| Age (Years, Mean+Sd) | 35.2±2.55 | 20-70 |
| Gender (M/F) | 12/8 | |
Clinical Variables
Probing Pocket Depth (PPD): PPD was measured with respect to the all the sites receiving test gel and placebo. The mean probing pocket depth for the teeth which received anaesthetic gel was 7.18±0.96 mm and the teeth which received placebo gel was 7.35±1.03mm [Table/Fig-8]. By conventional criteria, this difference is considered to be not statistically significant.
Mean probing depth calculated by using Paired
| Mean+Std Deviation | T Statistic |
|---|
| PPD Test Site | 7.870±1.076 | 0.7066 |
| PPD Placebo Site | 7.950±1.001 | |
t-test in the test and the placebo site.
PAIRED t-test (p>0.05)
Visual Analog Scale Score (VAS): The mean VAS score for the test group was 0.621±0.25 and the placebo group was 3.22±1.08 [Table/Fig-9]. Significant difference in the mean VAS scores was found between the test group and the placebo group. Mean, standard deviation, median, minimum, maximum, range and inter quartile range were calculated.
Mann Whitney U Test performed to calculate VAS scores
| N | Mean | Std. Deviation | Minimum | Maximum | u Statistic |
|---|
| C1 | 20 | 0.6210 | 0.25089 | 0.16 | 1.08 | 14 |
| C2 | 20 | 3.2225 | 1.08779 | 0.50 | 5.08 | |
Descriptive Statistics.
C1-Anaesthetic gel; C2-Placebo. p<0.05
Discussion
Periodontal probing is one of the baseline clinical examination procedures which is carried out to assess the degree of periodontitis in the patients. The response to periodontal therapy is evaluated with the help of parameters like PPD and CAL. In untreated chronic periodontitis patients the periodontal tissues are in their inflamed state as a result of which probing performed at this state has proven to be a painful procedure in about 15-77% of patients [15-17]. The amount of pain during probing procedures is associated with the extent of periodontal inflammation [18]. Results from one study demonstrated at a histologic level that in an untreated inflammed periodontal site, the periodontal probe penetrates the epithelium at the base of a periodontal pocket into the surrounding connective tissue, which is heavily infiltrated with inflammatory cells. In a treated, non-inflamed site, the periodontal probe does not penetrate through the epithelium at the base of the pocket [19].
Previous studies, which were conducted in a similar manner to eliminate pain on probing used anaesthetic gels of higher concentration (EMLA, 10% Lidocaine, 20% Benzocaine, etc.,) which are not cost effective. Hence, the present study focused on an anaesthetic gel that is of less concentration and cost effective which can be used in our daily dental practice. The aim of the present trial was to evaluate the efficacy of LOX 2% as an intrapocket anaesthetic gel in the reduction of pain while probing when compared with placebo. The results demonstrated a significant reduction in pain on the side receiving test gel compared to the side that received placebo. These findings were in accordance with the study [20] wherein, they evaluated the efficacy of two anaesthetic gels (Lidocaine 10% and Benzocaine 20%) in the reduction of pain during periodontal probing using Florida probe in patients with untreated CGP in comparison with manual probing and they concluded that use of local anaesthetic gels in baseline periodontal probing provide a significant reduction in pain in untreated periodontitis patients. The use of local anaesthetic gels previously was carried out in SRP procedures in three previous multicenter, double-masked, randomized, placebo-controlled clinical trials wherein the efficacy of the anaesthetic gel for purpose of SRP procedures was evaluated. The three studies included 337 individuals at 18 study centers. The studies used Hodges-Lehmann point estimate of treatment differences and found that the results favor the anaesthetic gel by reducing VAS pain scores by magnitudes of 8 (12), 4 (13), and 10 (14). Later on the use of anaesthetic gels prior to periodontal probing was performed in order to reduce pain on probing thereby increasing patients comfort and approach towards periodontal procedures. A study compared the use of a 5% Eutectic Mixture Of Local Anaesthetics (EMLA) cream to a standard 5% lidocaine intra oral topical anaesthetic for the purpose of performing periodontal probing in which 14 patients participated in the study where a 5 minute application of EMLA cream in a customized intraoral splint was done [21]. Recently, a study done by Winning L et al., evaluated the efficacy of Oraqix in the reduction of pain during periodontal probing, results of the above studies were in accordance with the present study, in that the use of anaesthetic gels significantly reduced pain on probing and there was also increase in the probing depths recorded [22]. Another study compared the efficacy of EMLA 5% cream and Lox 2% gel wherein the results showed anaesthetic efficacy for EMLA 5% as well as LOX 2% gel with statistically significant reduction in pain on periodontal probing in patients with untreated chronic periodontitis [23]. However, the use of EMLA in periodontal probing has its own limitations. LOX 2%, when compared to other anaesthetic gels has very minimal side effects and also is very cost effective. Some studies however used manual probing in order to reflect private clinical conditions and therefore, there is every chance of bias occurring with respect to amount of probing force employed. Hence, in the present study we performed probing with a TPS. The idea of using a TPS (VIVACARE) is for standardization of probing force i.e., 8.4g at all the probing sites [24]. As far as our knowledge is concerned this is the first study to use a low concentration level and cost effective anaesthetic gel (LOX 2%) as well as probing using a true pressure sensitive probe for evaluation of pain while probing and the results demonstrated a significant reduction in pain on probing.
Limitation
The limitation of the present study was that the sample size was relatively smaller.
Future Perspectives and Clinical Implications
The results of the study demonstrated that the use of LOX 2% jelly prior to periodontal probing has proven to be effective in reducing pain while probing. However additional trials with larger sample size can be done to confirm the results of the present trial.
Periodontal disease is a “silent disease” and periodontal screening should be an integral part of diagnosis. Periodontal examination, which consists of probing has become a technique sensitive method. There is a need for easy, reliable and reproducible method of periodontal probing in daily practice. The association of pain while probing makes it a difficult procedure. Hence, the study was done to eliminate the pain elicited during the probing procedure which can alter the diagnosis and treatment plan.
Conclusion
Within the limitations of the study, administration of LOX 2% gel in periodontal pockets prior to probing have shown a significant reduction in pain while probing. However, additional trials with larger sample size should be performed to confirm the efficacy of the gel, so that it can be used in our day to day practice.