Terbinafine in Fixed Cutaneous Sporotrichosis: A Case Series
Shailendra Vikram Jitendra Singh1, Romita Bachaspatimayum2, Usham Dharmaraja Meetei3, Subhalakshmi Devi Akham4, Rita Devi Sanjenbam5
1 Postgraduate Student, Department of Pharmacology, RIMS, Imphal, Manipur, India.
2 Assistant Professor, Department of Dermatology, Venereology and Leprosy, RIMS, Imphal, Manipur, India.
3 Assistant Professor, Department of Pharmacology, RIMS, Imphal, Manipur, India.
4 Professor, Department of Pharmacology, RIMS, Imphal, Manipur, India.
5 Professor, Department of Pharmacology, RIMS, Imphal, Manipur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shailendra Vikram Jitendra Singh, Room no. 102, First floor, Gents hostel no. 5, RIMS campus, RIMS, Lamphelpat, Imphal -795004, Manipur, India.
E-mail: shailendravikram121@gmail.com
Sporotrichosis is a chronic granulomatous mycotic infection caused by thermally dimorphic fungus, Sporothrix schenckii. The disease is endemic in tropical and subtropical belts throughout the world. In India, it is commonly seen in the Himalayan belt, frequently encountered in gardeners. Infection generally occurs by traumatic inoculation of soil and plants contaminated with the fungus. In humans, the lesions are usually restricted to the skin, subcutaneous cellular tissue and adjacent lymphatic vessels. Disseminated disease occurs when the fungus spreads throughout the body. Itraconazole is regarded as the treatment of choice for patients with most forms of cutaneous as well as extracutaneous sporotrichosis and amphotericin B as the preferred treatment for patients who are severely ill in disseminated mycotic infections. Terbinafine is a synthetic allylamine used as the drug of choice in tinea infections. This article compiles three cases of fixed cutaneous sporotrichosis, proven histopathologically, who were treated with oral terbinafine due to poor response to itraconazole or because of cost factor, with dosage ranging from 250mg/day to 1g/day, given upto six weeks after clinical resolution. The article also highlights the importance of terbinafine as an effective drug for sporotrichosis where there is poor response to itraconazole or affordability may be an issue.
Antifungal, Cutaneous infection, Sporothrix schenckii
Case Series
Case 1
A 51-year-old Hindu housewife from a rural area in Manipur presented with scaly crusted lesion over the left ear lobule with hypopigmented lesion over the left pre-auricular area of two years duration. There was history of being scratched by a domestic cat’s nails prior to the development of the lesions. The hypopigmented lesion was preceded by scaly crusted lesion which resolved spontaneously.
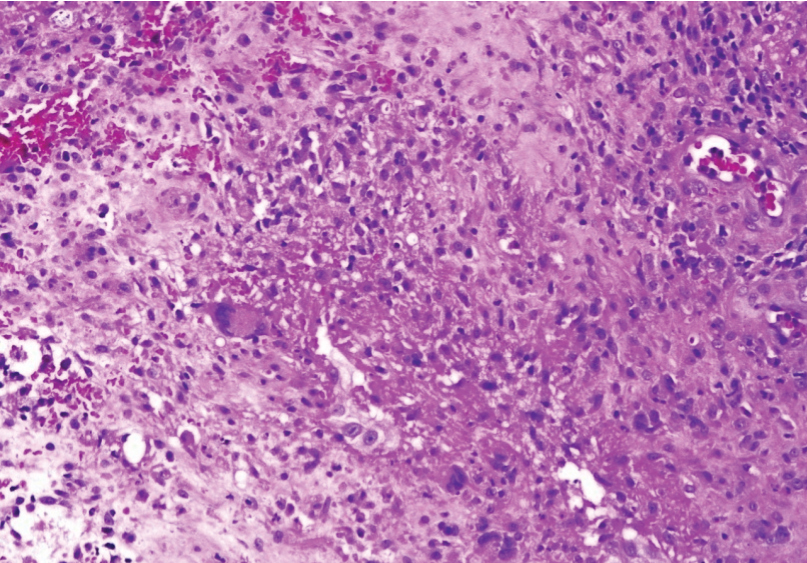
She had consulted a local dermatologist two years back when the disease started. Skin biopsies taken two years back from the left ear lesion which showed features of Lupus Vulgaris and Periodic Acid Schiff (PAS) stain, Zeihl Neelsen (ZN) stain and Fite Faraco stain were negative. She was treated as a case of Lupus Vulgaris with Antituberculer Treatment (ATT) by the same doctor with oral rifampicin 450 mg, isoniazid 300 mg, ethambutol 800 mg with no response after three months. At this time (after three months of ATT), a repeat skin biopsy was taken from similar site, as advised by the treating dermatologist, which showed suppurative granulomatous inflammatory lesion with yeast cells resembling Sporothrix schenkii which was PAS positive. Fungal culture showed growth of Sporothrix schenkii. The patient was reluctant to undergo further treatment due to which she stopped visiting her previous doctor and was not under any medication for a year. After one year, she was advised itraconazole 100 mg twice daily for three months, by another dermatologist whom she consulted, with minimal response after which she discontinued it on her own after taking for three months.
When the patient reported to our Department, general physical examination was normal. Cutaneous examination revealed scaly, erythematous, 2.5x1cm, verrucous plaque with hemorrhagic crusts and scarring over left ear lobule and hypopigmented patch and scar over the left pre-auricular area [Table/Fig-1]. There was no lymphadenopathy. Systemic examination was normal. Routine investigations were within normal limits. Skin biopsy and fungal culture were repeated which confirmed the diagnosis of sporotrichosis [Table/Fig-2]. She was started on oral terbinafine 250 mg/day with fair response at one month which was gradually increased to 1g/day following which there was a dramatic improvement. The dose was then tapered to 500 mg/day after complete clinical resolution, as the patient experienced mild nausea and abdominal discomfort, and continued for another six weeks, with a total duration of eight months [Table/Fig-3]. Liver function test was monitored six weekly and was within normal limits. There was no relapse. Eight months later, the treatment was discontinued.
Verrucous plaque left ear.

HPE showing suppurative granuloma (H&E x 10).
At four months follow-up.

Case 2
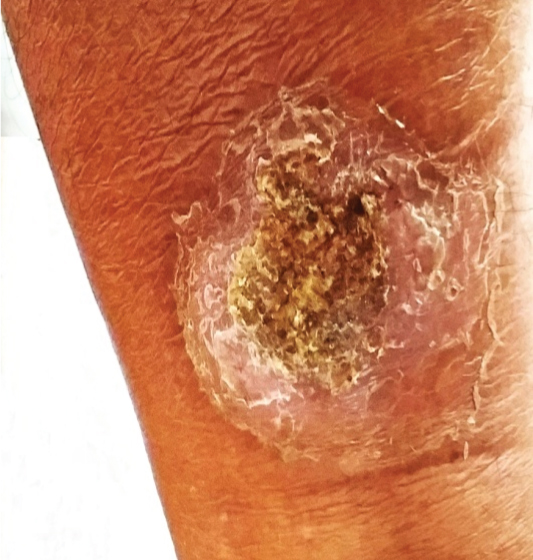
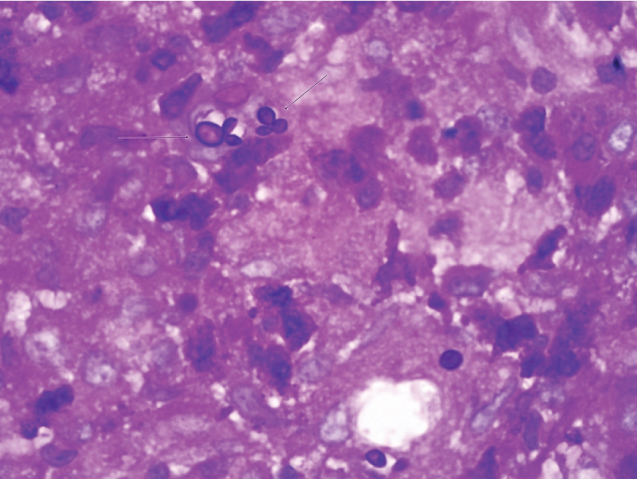
A 70-year-old married Hindu male from rural Manipur presented with mildly itchy skin lesion, gradually increasing in size, over right lower leg for the last five months. There was no history of prior treatment for the same and there was no history of trauma and he was a known case of diabetes mellitus for the last one year on 45 units of insulin per day. General physical examination was normal. Cutaneous examination revealed an annular verrucous plaque, 5 x 4 cm, with central crusting and peripheral scaling over the right lower leg [Table/Fig-4]. Systemic examination was normal. Histopathological examination of skin biopsy showed suppurative ill-formed granulomas in the dermis with budding yeast cells of a fungus, morphologically resembling Sporothrix schenckii, highlighted by special stain (PAS) with moderate mixed inflammatory cell infiltration and mildly hyperplastic epidermis [Table/Fig-5]. Fungal culture was however, negative. Routine investigations were normal. Due to unaffordability of itraconazole, he was started on terbinafine 250mg/day with significant improvement at four weeks and complete clinical resolution with mild scarring and post inflammatory hyperpigmentation at four months [Table/Fig-6]. Liver function test was monitored six weekly and was within normal limits. He was advised to continue the medication for one more month. However, he was lost to follow-up.
Verrucous plaque right leg.
PAS Stain showing budding yeasts (arrow).
At four months follow-up.

Case 3
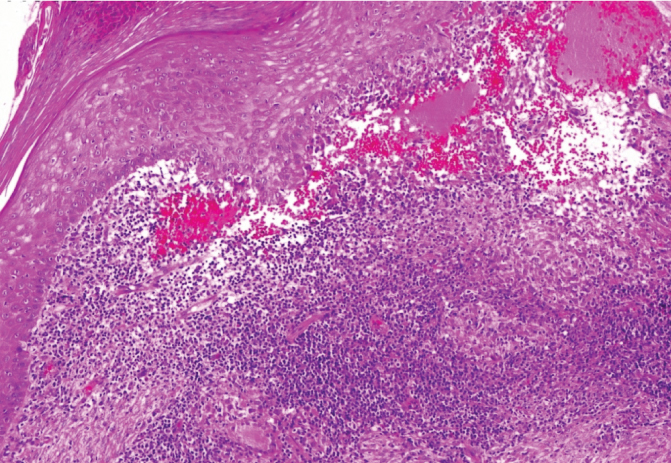
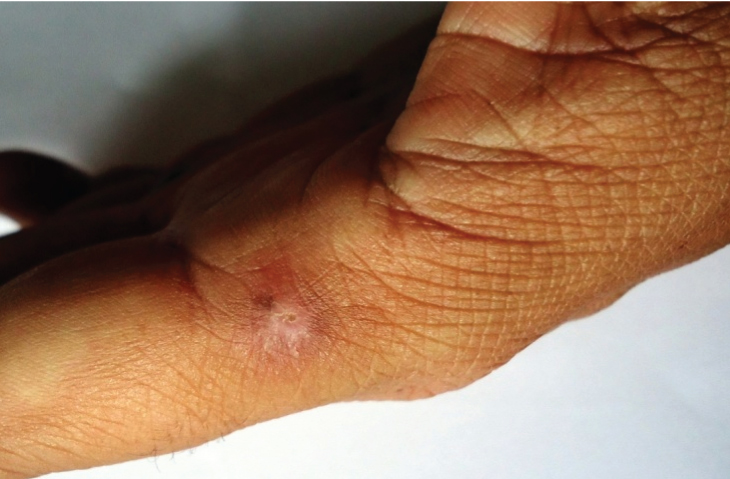
A 42-year-old married Hindu male farmer from rural Manipur presented with a non-healing wound over left index finger of five months duration. There was history of prick with the thorn of a plant grown near the field. It was started as a cut which resolved and after about a month, he noticed a papule which became pustular and then became ulcerated. General physical examination was normal. Cutaneous examination revealed an ill-defined erythematous, edematous, non-tender plaque 1.5 x 1 cm, with central erosion and mild induration over the base of left index finger [Table/Fig-7]. Systemic examination was normal. Histopathological examination of the skin biopsy showed well-formed epithelioid granulomas in the dermis with scattered Langhans cells with central suppuration, pseudoepitheliomatous hyperplasia of the epidermis and budding yeast cells morphologically resembling Sporothrix schenckii highlighted by PAS stain [Table/Fig-8]. Fungal culture revealed no growth. Due to inability to afford itraconazole, he was started on terbinafine 500 mg/day with complete clinical resolution with mild scarring after three months [Table/Fig-9]. Fungal culture at three months was also negative. Liver function test was monitored six weekly and was within normal limits. He was advised to continue the medication for another six weeks and is still on regular follow-up.
Plaque with central erosion over left index finger.

HPE showing Pseudoepitheliomatous hyperplasia (H&Ex10).
At four months follow-up.
Discussion
Sporotrichosis is a chronic granulomatous mycotic infection caused by thermally dimorphic fungus, Sporothrix schenckii. Infection generally occurs by traumatic inoculation of soil and plants contaminated with the fungus [1]. Fixed cutaneous sporotrichosis often poses diagnostic challenges due to its varied modes of presentation. It may present as an ulcer or a vegetative verrucous plaque, infiltrated or tuberous without lymphatic involvement. Infection usually appears after minor trauma to the skin, with disruption of the integrity of the epidermis after which the fungus converts into the yeast form and remain localised in the subcutaneous tissue constituting the fixed type. Sporotrichosis can be diagnosed through a correlation of clinical, epidemiological, and laboratory data. Laboratory analysis for the determination of sporotrichosis includes direct examination of specimens such as tissue biopsy specimens or pus from lesions and in case of disseminated infections, sputum, urine, blood, and cerebrospinal and synovial fluids, can be analysed, depending on the affected organs. The fungus is evident as budding yeasts in both human and animal tissues. There are few reports on the mycosis following animal bites or scratches by cats and squirrels, insect bites, and other injuries [1,2]. Our first case also gave a history of being scratched by a domestic cat which may support this finding.
There are various treatment options for sporotrichosis like itraconazole, terbinafine, amphotericin B, Saturated Solution of Potassium Iodide (SSKI), etc. Itraconazole is an orally active triazole antifungal agent which inhibits the fungal cytochrome P450 enzyme ‘lanosterol 14-demethylase’ and thus, impair ergosterol synthesis leading to a cascade of membrane abnormalities in the fungus [3]. In our first case who failed to respond to itraconazole 200 mg/day, terbinafine was started as she was reluctant to continue with the same medicine at a higher dose. Terbinafine was also given in our second and third cases due to higher cost of itraconazole as affordability was an issue. The response in all the three cases was quite remarkable with non-serious adverse effects in the first and third cases. Adverse effects were not observed in our second case till complete resolution of the lesion.
Terbinafine is an orally and topically active drug against dermatophytes and Candida which belongs to a new synthetic allylamine class of antifungals. It acts as a non-competitive inhibitor of squalene epoxidase, an early step enzyme in ergosterol biosynthesis by fungi. Accumulation of squalene within fungal cells appears to be responsible for the fungicidal action. Oral terbinafine is usually well tolerated [3,4]. Intravenous amphotericin B is the treatment of choice for mucormycosis and is used for initial treatment of severe histoplasmosis, blastomycosis, penicilliosis and extracutaneous sporotrichosis [5]. Cutaneous and subcutaneous involvement in sporotrichosis is more common than disseminated forms. It can be treated readily; with oral itraconazole 200 mg/day for 2–4 weeks after all lesions have healed, usually for a total duration of 3–6 months. Patients not responding to this regimen should be given oral itraconazole 200 mg twice daily, oral terbinafine 500 mg twice daily, or SSKI in standard dosing schedule [6].
The geographic distribution of Sporothrix schenckii strains also appears to play an important role in antifungal susceptibility [1]. Terbinafine is well absorbed after oral administration with low binding to microsomal cytochrome P450 enzyme, and has no effect on bioavailability of other drugs metabolised by this enzyme system. Since, it is highly lipophilic, its antifungal activity is maintained from adipose tissue depots few weeks after discontinuation of treatment [6]. In in-vitro studies terbinafine was the most active drug compared to itraconazole, ketoconazole, or posaconazole against human and animal isolates of S. schenckii [7]. Terbinafine 250 mg/day was found to be an effective and well tolerated alternative to treatment of cutaneous sporotrichosis in patients where itraconazole use was not possible [8]. In another study, terbinafine 250 mg/day was found to be comparable in terms of effectiveness and tolerability to that of itraconazole 100 mg/day in the treatment of cutaneous sporotrichosis [9]. S. schenckii is regarded as a complex of different phylogenic species with different geographic distribution, virulence, and in vitro susceptibility to antifungal agents has helped in understanding variability of therapeutic response observed across antimicrobial agents. This perhaps will form the basis for future research particularly in therapeutics that remains under studied and lacks well-designed controlled clinical trials [6].
Conclusion
This case series highlight the importance of oral terbinafine as an effective drug for sporotrichosis in situations where response to itraconazole is poor or higher price of itraconazole may lead to poor patient compliance, especially in a developing country like ours. Randomised controlled trials with more number of patients are being recommended as terbinafine is well tolerated and is also relatively safer, due to fewer drug interactions as compared to itraconazole.
[1]. Barros MBDL, Paes RDA, Schubach AO, Sporothrix schenckii and sporotrichosisClin Microbiol Rev 2011 24(4):633-54.10.1128/CMR.00007-1121976602 [Google Scholar] [CrossRef] [PubMed]
[2]. Borrego JAB, Mayorga J, Martınez VMT, Simultaneous bilateral lymphangitic sporotrichosisRev Iberoam Micol 2009 26(4):247-49.10.1016/j.riam.2009.06.00219818662 [Google Scholar] [CrossRef] [PubMed]
[3]. Tripathi KD, Essentials of Medical Pharmacology 2013 7thedNew DelhiJaypee Brothers Medical Publishers (P) Ltd:787-97.10.5005/jp/books/12021_61 [Google Scholar] [CrossRef]
[4]. Meinerz ARM, Xavier MO, Cleff MB, Madrid IM, Nobre MO, Meireles MCA, Efficacy of terbinafine and itraconazole on an experimental model of systemic sporotrichosisBraz J Microbiol 2008 39:734-37.10.1590/S1517-8382200800040002524031298 [Google Scholar] [CrossRef] [PubMed]
[5]. Bennett JE, Antifungal Agents. In: Brunton LL, Chabner BA, Knollman BC, editorsThe pharmacological basis of therapeutics 2011 12th edNew YorkThe Mc Graw Hill Companies:1237-73. [Google Scholar]
[6]. Mahajan VK, Sporotrichosis: An overview and therapeutic optionsDermatol Res Prat 2014 :1-13.10.1155/2014/27237625614735 [Google Scholar] [CrossRef] [PubMed]
[7]. Marimon R, Serena C, Gene J, Cano J, Guarro J, In vitro antifungal susceptibilities of five species of SporothrixAntimicrobial Agents and Chemotherapy 2008 52(2):732-34.10.1128/AAC.01012-0718039919 [Google Scholar] [CrossRef] [PubMed]
[8]. Francesconi G, Valle AC, Passos S, Reis R, Galhardo MC, Terbinafine 250mg/day: an effective and safe treatment of cutaneous sporotrichosisJ Eur Acad Dermatol Venereol 2009 23(11):1273-76.10.1111/j.1468-3083.2009.03306.x19573026 [Google Scholar] [CrossRef] [PubMed]
[9]. Francesconi G, Francesconi dV AC, Passos SL, Paes R dA, Curi AL, Liporage J, Comparative study of 250mg/day terbinafine and 100mg/day itraconazole for the treatment of cutaneous sporotrichosisMycopathologia 2011 171(5):349-54.10.1007/s11046-010-9380-821103938 [Google Scholar] [CrossRef] [PubMed]