Visual Outcome and Complications of Manual Sutureless Small Incision Cataract Surgery with Foldable IOL-A Teaching Hospital Based Study
Ajit Kamalakar Joshi1, Sakshi Ravikant Patil2, Navneet Tajendersingh Chhabda3, Abhishek Kumar Tripathi4
1 Professor and Head, Department of Ophthalmology, Bharati Vidyapeeth (Deemed to be University) Medical College and Hospital, Sangli, Maharashtra, India.
2 Associate Professor, Department of Ophthalmology, Bharati Vidyapeeth (Deemed to be University) Medical College and Hospital, Sangli, Maharashtra, India.
3 Resident, Department of Ophthalmology, Bharati Vidyapeeth (Deemed to be University) Medical College and Hospital, Sangli, Maharashtra, India.
4 Resident, Department of Ophthalmology, Bharati Vidyapeeth (Deemed to be University) Medical College and Hospital, Sangli, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ajit Kamalakar Joshi, Abhang, 248,9/A, An and park road no 2, Abhaynagar, Sangli-416416, Maharashtra, India.
E-mail: ajit_jshi@rediffmail.com
Introduction
Manual Small Incision Cataract Surgery (SICS) is an effective alternative to phacoemulsification surgery. SICS with single piece foldable Intraocular Lens (IOL) implantation ensures compulsory in the bag placement of IOL due to Continuous Curvilinear Capsulorrhexis (CCC). It is also associated with less chances of complications like after cataract because of the foldable lens implanted, giving it an upper edge over the SICS with rigid IOL implantation.
Aim
To assess best spectacle corrected visual acuity at one month postoperative in cases who underwent SICS with foldable IOL and also to evaluate their complications.
Materials and Methods
Prospective study conducted on 30 patients in Department of Ophthalmology, Bharati Medical College Deemed to be University and Hospital, Sangli for one month from August 2017 to September 2017. Preoperative examination of patients consisted of autokeratorefractometry, visual acuity, detailed slit lamp examination to rule out any significant anterior segment pathologies, type of cataract on the basis of morphology on slit lamp and applanation tonometry. A-scan was done by contact method and Fundus examination was done to rule out any posterior segment pathologies. At all follow-up visits i.e., at one week and one month patients underwent autorefractometry, visual acuity with corrected refractive correction, anterior and posterior segment evaluation on slit lamp to rule out any postoperative complications. The statistical analysis by Z-test was performed comparing the unaided visual acuity of patients preoperatively and postoperatively at one month.
Results
The number of patients at post-operative one month were significantly less than preoperative for the visual acuity of (6/60-6/36). The Z-Score was 2.3355. The p-value was 0.01928. The result was significant at p<0.05.
Conclusion
This study showed that manual SICS patients can have good visual outcome at the end of one month and when combined with the benefits of acrylic IOL it can be a long term solution to affordability issues related to the cataract surgery. Thus, the use of this combination technique can be a good tool in eliminating cataract from the developing world.
Autorefractometry, A-scan, Phacoemulsification, Posterior capsular opacification
Introduction
Globally, cataract still remains the number one cause for blindness [1]. WHO’s Visual Impairment and Blindness report 2010 reveals that 285 million people are affected by visual impairment. Out of which, 20 million people are affected by bilateral cataracts. This poses one of the greatest public health challenge for 21st century [2].
Manual SICS involves creating sclerocorneal tunnel, anterior capsulotomy, hydrodissection, dislodging nucleus into anterior chamber, viscoexpression of nucleus from the tunnel, removal of cortex and implantation of IOL. Major complications include tunnel related problems, posterior capsular rent, iridodialysis etc. As compared to phacoemulsification, Manual SICS is safer in hard cataracts and in cataracts associated with phacolytic and phacomorphic glaucoma due to its short operative time giving excellent visual outcomes on one month follow-up. This assumes more significance in developing countries like India where such cases are more commonly seen. As compared to phacoemulsification, Manual SICS can be done at affordable rates [3,4].
Foldable IOLs because of their in the bag placement and less incidence of postoperative Posterior Capsular Opacification (PCO) are preferred over rigid IOLs [5,6].
In a semi-urban area like ours, majority of cataract patients undergo Manual SICS with rigid IOLs as it is cost effective. It is found that the chances of PCO is higher with rigid IOL [7] subjecting the patients to early YAG laser capsulotomy.
As many patients could not afford the benefits of phacoemulsification and foldable IOL, we thought of modifying this procedure by putting foldable IOLs after Manual SICS. This gave a comparable visual outcome with less chances of PCO.
Different studies have been done comparing advantages and disadvantages, cost effectiveness, visual results, surgical time and complications between phacoemulsification with rigid IOL and SICS [5,8,9]. Singh K et al., in their study on Manual SICS has suggested that in affordable patients and where incision size is <5mm SICS can be done with foldable IOLs [10].
We are reporting here a series of 30 patients who underwent SICS with foldable IOLs, in view of highlighting the benefits of SICS with foldable IOLs.
This study was undertaken with the aim to assess final best corrected visual acuity at one month postoperative and also to determine complications of manual sutureless SICS with foldable IOL.
Materials and Methods
Prospective study was conducted on 30 eyes of 30 patients with cataract who were subjected to Manual SICS with Acrylic foldable IOL implantation under local anaesthesia in a teaching hospital between the period from August 1, 2017 to September 1, 2017. Written and informed consent was taken from all the patients. All patients were followed-up for a period of one month postoperative for visual acuity.
The patient with immature cataract, mature cataract and nuclear cataract were included in the study. The patients with any posterior segment pathologies, glaucoma, uveitis, dry eye, developmental cataract, traumatic cataract, corneal opacity affecting vision, nuclear sclerosis more than grade 4 were excluded from the study. Preoperative examination of patients was done to assess the various parameters and calculate exact IOL power. It included auto-refractokeratometry to find out refractive status of eye and corneal curvature to rule out keratoconus, visual acuity testing by Snellens’s chart [11]. Detailed slit lamp examination to determine the type of cataract and to rule out any significant anterior segment pathologies like corneal pathologies or uveitis. Applanation tonometry was done to rule out glaucoma. A-scan biometry was done by contact method to calculate accurate intraocular lens power. Fundus examination was done to rule out any posterior segment pathologies like vascular occlusions, age-related macular degeneration etc., At all follow-up visits i.e., at (one week and one month): Autorefractokeratometry was done for finding out objective postoperative refractive error along with surgically induced astigmatism, visual acuity by Snellens’s chart to check unaided visual acuity and BCVA with pinhole, detailed slit lamp examination for any post-op surgical complication like AC reaction, DM detachment, hyphema etc., and fundus examination to rule out cystoid macular oedema. At one month follow-up, refraction was given.
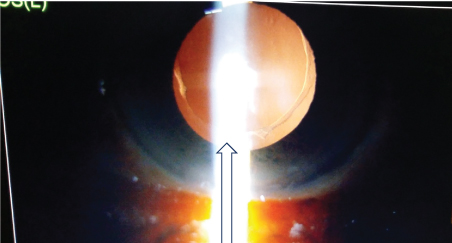
Preoperatively in wards, xylocaine sensitivity testing was done. In operation theatre: Peribulbar block was given by using local anaesthetics i.e., Xylocaine 2% with adrenaline 1:100000. All the surgeries were performed by same surgeon with same surgical technique. The eye and periocular area was painted with povidone iodine solution and draped. Universal eye speculum was applied and superior rectus suture was taken. After doing conjunctival peritomy from 11 to 1o’clock, frown incision of 5-6 mm width was taken at a distance of 2 mm from limbus with a 15 number blade. Sclero-corneal tunnel was made with a crescent knife. A side port was made at the limbus at 9o’clock position at right angle to the plane of approach with the 15 degree sideport entry blade. Through the sideport, trypan blue dye was injected in the anterior chamber and washed after 30 seconds. CCC was done with the help of a cystitome made from 26 no. needle [Table/Fig-1]. Entry into the anterior chamber was done with a 3.2 mm keratome and internal opening of the sclerocorneal incision was widened, so as to facilitate the nucleus delivery. Hydrodissection and hydrodelination was performed and nucleus was delivered by viscoexpression. Cortical matter was aspirated with Simcoe’s cannula and a foldable single piece hydrophilic acrylic IOL was implanted within the bag [Table/Fig-2]. Visco-elastic material was removed. Intracameral moxifloxacin was injected into the anterior chamber. Scleral wound was then checked for its self sealing character. Subconjunctival injection gentamycin and dexamethasone was given to approximate conjunctival incision flap. After putting chloramphenicol eye ointment, the eye was padded.
Image showing Continuous Curvilinear Capsulorrhexis (CCC).
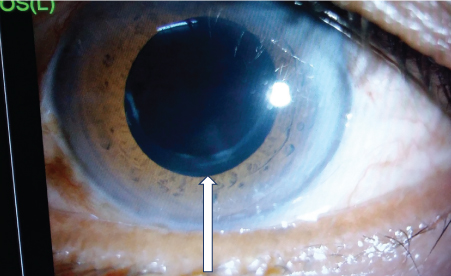
Image showing in the bag placement of foldable IOL after SICS.
Appropriate approval was taken from the Ethical committee to conduct the study.
Statistical Analysis
A statistical analysis was performed comparing the visual acuity of patients measured preoperatively, at postoperative one week as well as at postoperative one month. Frequency and percentages were obtained. Z-test (Standard error of difference between proportions is used to compare the visual acuity of patients) with MS Excel and SPSS-22 were used for the statistical analysis.
Age groups of the patients ranged from 41-80 years and above, of which 14 patients were male and 16 were female [Table/Fig-3]. The preoperative visual acuity in the patients was significantly low. Out of the total 30 patients, seven had the visual acuity of Perception of Light (PL), Projection of Rays (PR) and Hand Movements (HM). Majority of patients i.e., 14 had visual acuity ranging from counting finger 1-6 meters. Nine patients had visual acuity of 6/60-6/36.
Distribution of patients according to age.
| Age of the patient | No. of patients | Percentage |
|---|
| 41-50 years | 5 | 16.66% |
| 51-60 years | 14 | 46.66% |
| 61-70 years | 8 | 26.66% |
| 71-80 years and above | 3 | 10% |
| Total | 30 | |
No patient had visual acuity more than 6/36 preoperatively [Table/Fig-4]. Postoperatively, the number of patients decreased significantly after one month for the visual acuity of 6/60-6/36 as none of the patients had uncorrected visual acuity <6/36 [Table/Fig-4]. Postoperatively there was immense improvement in visual acuity of patients with a majority i.e.,10 patients having uncorrected visual acuity of 6/9 [Table/Fig-4].
Distribution of patients according to unaided visual acuity.
| Unaided visual acuity | No. of patientspreoperatively | No. of patientspostoperativelyat one week | No. of patientspostoperatively at one month |
|---|
| Perception of light,projection of raysin all quadrant,hand movementsclose to face | 7 | 0 | 0 |
| Counting fingerfrom 1m-6m | 14 | 0 | 0 |
| 6/60 -6/36 | 9 | 5 | 2 |
| 6/24- 6/9 | 0 | 22 | 23 |
| 6/6 | 0 | 3 | 5 |
| Total | 30 | 30 | 30 |
Postoperative no. of patients are significantly less than preoperative for the visual acuity, 6/60 – 6/36. (or number of postoperative patients is decreased significantly after one month for the visual acuity, 6/60 – 6/36.) The Z-Score is 2.3355. The p-value is 0.01928. The result is significant at p <0.05
The best corrected visual acuity with pinhole at one week being 6/6 in 25 patients out of the 30 [Table/Fig-5]. Postoperative best corrected visual acuity with pinhole at one month showed most significant results with vision being 6/6 in 27 patients out of the 30 [Table/Fig-6].
Distribution of patients according to postoperative best corrected visual acuity with pin hole at one week.
| Visual acuity with pinhole | No. of patients | Percentage |
|---|
| 6/9 | 5 | 16.66% |
| 6/6 | 25 | 83.33% |
Distribution of patients according to postoperative best corrected visual acuity with pin hole at one month.
| Visual acuity with pinhole | No. of patients | Percentage |
|---|
| 6/9 | 3 | 10% |
| 6/6 | 27 | 90% |
Three patients who developed complications had the best corrected visual acuity with pinhole of 6/9 [Table/Fig-7]. The postoperative complications were very less and presented only in three patients. These included Descemet’s detachment in one patient, postoperative corneal oedema in one patient and postoperative anterior chamber collapse in one patient. All three of them were managed conservatively.
Distribution of occurrence of postoperative complication.
| Complication | No. of patients | Percentage |
|---|
| Yes | 3 | 10% |
| No | 27 | 90% |
In one patient who on postoperative day one had shallow AC with Siedels’ test positive was diagnosed as having wound leak. Patient was given pad bandage for two days. Mydriatics along with steroids and oral tablet acetazolamide 250 mg was given to the patient. Anterior Chamber was formed on the 3rd day and the BCVA in this patient improved to 6/9. Surgery in rest of the patients was uneventful.
Discussion
We achieved excellent visual outcomes in 27 cases i.e., 6/6 and three cases had a visual acuity of 6/9. The BCVA results in our study are comparable with the results reported from other studies on manual SICS [12-14]. Many patients in our study had satisfactory near vision due to surgically induced myopic astigmatism. Gogate P et al., in his study also noticed uncorrected BCVA for near satisfactory in patients with SICS [15].
Out of 27 patients, seven cataracts included in our study were white cataract (vision of PL and PR). Postoperatively all had a good visual outcome as reported above. In a comparative study by Venkatesh R et al., authors have concluded that SICS may be a more appropriate technique in eyes with mature cataract in the developing world [16].
We had three cases of complications of which one had intraoperative small Descemet’s membrane detachment during main incision and air bubble was put in the anterior chamber. It settled after 15 days post surgery. The BCVA in this patient remained 6/9. Patil MS et al., in her study on intraoperative complications of SICS, reported DM detachment in 1.2% which was settled by pneumatic descemetopexy [17].
In our case series, one patient had corneal oedema due to transient secondary glaucoma. Oedema resolved within a week with tablet acetazolamide and topical steroid eyedrops. Hennig A et al., in his study also noted a case of postoperative corneal oedema which was treated with steroid drops [18].
As the study was conducted in a semiurban area with low income groups, the preference was given to SICS over phacoemulsification because of its affordability and easy learning curve for the surgeons. Our experience of SICS has shown it to be faster, effective as phaco and less expensive. Venkatesh R et al., in his study has also concluded that SICS is significantly faster, less expensive, and less technology dependent than phacoemulsification [16]. Similar to our findings, Ruit S et al., has also observed that SICS may be the more appropriate surgical procedure for the treatment of advanced cataracts in the developing world [19].
We could not notice a single case of PCO (Posterior capsular Opacification) in our study as the follow-up duration of our patients was less. Deepankar UP and Jain B, in his study has quoted that foldable acrylic IOLs have lower rate of capsular opacity than rigid PMMA lenses [20].
Limitation
Small sample size was the main limitation of this study. Also, short duration of follow-up in our study prevented us from commenting on long term complications and foldable IOLs like after cataract.
Conclusion
Cataract, the major cause of avoidable blindness in the developing world, needs to be treated upfront with the surgical tools available. For this aim, using the manual SICS technique is an affordable and readily available tool at hand. Combining this technique with the advantage offered by the acrylic IOL increases the visual prognosis in patients and decreases the risk of long term complications of posterior capsular opacification.
This study showed that manual SICS patients can have good visual outcome at the end of one month and when combined with the benefits of acrylic IOL, it can be a long term solution to affordability issues related to the cataract surgery. Thus, the use of this combination technique can be a good tool in eliminating cataract from the developing world.
Postoperative no. of patients are significantly less than preoperative for the visual acuity, 6/60 – 6/36. (or number of postoperative patients is decreased significantly after one month for the visual acuity, 6/60 – 6/36.) The Z-Score is 2.3355. The p-value is 0.01928. The result is significant at p <0.05
[1]. Pascolini D, Mariotti SP, Global estimates of visual impairment: 2010British Journal of Ophthalmology 2012 96:614-18.10.1136/bjophthalmol-2011-30053922133988 [Google Scholar] [CrossRef] [PubMed]
[2]. Global data on Visual Impairment 2010. Available at: (http://www.who.int/blindness/GLOBALDATAFINALforweb.pdf?ua=1) [Google Scholar]
[3]. Rajkumari V, Kaminibabu KS, Bhabanisana RD, Victor R, Manual small incision cataract surgery in phacomorphic glaucoma: surgical technique and outcome in north-eastern IndiaJ Current Glau Prac 2013 7(2):43-48.10.5005/jp-journals-10008-113626997781 [Google Scholar] [CrossRef] [PubMed]
[4]. Venkatesh R, Chang DF, Muralikrishnan R, Hemal K, Gogate P, Sengupta S, Manual small incision cataract surgery: a reviewAsia Pac J Ophthalmol (Phila) 2012 1(2):113-19.10.1097/APO.0b013e318249f7b926107133 [Google Scholar] [CrossRef] [PubMed]
[5]. Hennig A, Puri LR, Sharma H, Evans JR, Yorston D, Foldable vs rigid lenses after phacoemulsification for cataract surgery: a randomised controlled trialEye 2014 28(5):567-75.10.1038/eye.2014.2624556879 [Google Scholar] [CrossRef] [PubMed]
[6]. Pandey SK, Apple DJ, Werner L, Maloof AJ, Milverton EJ, Posterior capsule opacification:are view of aetiopathogenesis, experimental and clinical studies and factors for preventionIndian J Ophthalmol 2004 52:99-112. [Google Scholar]
[7]. Cheng JW, Wei RL, Cai JP, Xi GL, Zhu H, Li Y, Efficacy of different intraocular lens materials and optic edge designs in preventing posterior capsular opacification: a meta-analysisAm J Ophthalmol 2007 143(3):428-36.10.1016/j.ajo.2006.11.04517224119 [Google Scholar] [CrossRef] [PubMed]
[8]. Meta-Analysis_SICS vs PHACO_23032012KN_Review. Available at:(https://pdfs.semanticscholar.org/7b88/cea5372e108a602703bacf64dccdfdcf2a13.pdf) [Google Scholar]
[9]. Devendra J, Agarwal S, Singh PK, A comparative study of clear corneal phacoemulsification with rigid IOL versus SICS; the preferred surgical technique in low socio-economic group patients of rural areasJ Clin Diagn Res 2014 Nov 8(11):VC01-VC03.10.7860/JCDR/2014/10717.520825584291 [Google Scholar] [CrossRef] [PubMed]
[10]. Singh K, Misbah A, Saluja P, Singh AK, Review of manual small-incision cataract surgeryIndian J Ophthalmol 2017 65:1281-88.10.4103/ijo.IJO_863_1729208807 [Google Scholar] [CrossRef] [PubMed]
[11]. Macky TA, Mohamed AM, Emarah AM, Osman AA, Gado AS, Predicting postoperative visual outcomes in cataract patients with maculopathyIndian J Ophthalmol 2015 63:775-78.10.4103/0301-4738.17150726655002 [Google Scholar] [CrossRef] [PubMed]
[12]. Balent LC, Narendran K, Patel S, High volume sutureless intraocular lens surgery in a rural eye camp in IndiaOphthalmic Surg Lasers 2001 32:446-55. [Google Scholar]
[13]. Gogate PM, Deshpande M, Wormald RP, Extracapsular cataract surgery compared with manual small incision cataract surgery in community eye care setting in western India: a randomised controlled trialBr J Ophthalmol 2003 87:667-72.10.1136/bjo.87.6.66712770957 [Google Scholar] [CrossRef] [PubMed]
[14]. Gogate PM, Small incision cataract surgery: complications and mini-reviewIndian J Ophthalmol 2009 57:45-49.10.4103/0301-4738.4451219075410 [Google Scholar] [CrossRef] [PubMed]
[15]. Gogate P, Optom JB, Deshpande S, Naidoo K, Meta-analysis to compare the safety and efficacy of manual small incision cataract surgery and phacoemulsificationMiddle East African Journal of Ophthalmology 2015 22(3):362-69.10.4103/0974-9233.15976326180478 [Google Scholar] [CrossRef] [PubMed]
[16]. Venkatesh R, Das M, Prashanth S, Muralikrishnan R, Manual small incision cataract surgery in eyes with white cataractsIndian J Ophthalmol 2005 53:173-76.10.4103/0301-4738.1667516137961 [Google Scholar] [CrossRef] [PubMed]
[17]. Patil MS, Balwir DN, Dua S, Study of intraoperative complications in small incision cataract surgery, its management and visual outcomeMVP journal of Medical Sciences 2016 3(1):52-59.10.18311/mvpjms/2016/v3/i1/719 [Google Scholar] [CrossRef]
[18]. Hennig A, Kumar J, Yorston D, Sutureless cataract surgery with nucleus extraction: outcome of a prospective study in NepalBr J Ophthalmol 2003 87:266-70.10.1136/bjo.87.3.26612598434 [Google Scholar] [CrossRef] [PubMed]
[19]. Ruit S, Tabin G, Chang D, A prospective randomized clinical trial of phacoemulsification vs manual sutureless small incision cataract surgery in NepalAm J Ophthalmolo 2007 143:32-38.10.1016/j.ajo.2006.07.02317188040 [Google Scholar] [CrossRef] [PubMed]
[20]. Deepankar UP, Jain B, Comparison between rigid and foldable intraocular lenses regarding postoperative complication and visual rehabilitationsJ Evolution Med Dent Sci 2016 5(95):7000-04.10.14260/Jemds/2016/1583 [Google Scholar] [CrossRef]