Last few years has seen a major revolution taking place in the management of lung cancer. With the advent of targeted therapies against specific molecular alterations seen in lung cancer as well as breakthroughs in cancer immunotherapy, the role of pathologist has also considerably changed, not only with respect to diagnosis but also regarding management of the tissue.
Therapeutic advances in lung cancer have shown increased response to Epidermal Growth Factor Receptor (EGFR) and Tyrosine Kinase Inhibitors (TKIs) in adenocarcinoma patients harbouring EGFR mutations. Also, now it is necessary to exclude a diagnosis of squamous cell carcinoma because these patients respond better to pemetrexed and there is a risk of toxicity if these patients are treated with bevacizumab [1].
Addressing these changes, International Association for the Study of Lung Cancer (IASLC), the American Thoracic Society (ATS), and the European Respiratory Society (ERS) published a new classification with several recommendations. One of the major issues addressed in this classification was the importance of small samples, that is biopsies and cytology specimens, which comprise majority of the diagnostic material in the evaluation of lung cancer.
They recommended that for small biopsies and cytology, NSCLC should be further classified into a more specific histologic type, such as adenocarcinoma or squamous cell carcinoma, whenever possible and the term NSCLC-NOS (Not Otherwise Specified) should be used as little as possible, and applied only when a more specific diagnosis is not possible by morphology and/or special stains. This is owing to clear therapeutic benefits of tyrosine kinase and Anaplastic Lymphoma Kinase (ALK) inhibitors in lung adenocarcinoma patients [1].
The present study is an attempt to integrate the above mentioned recommendations and protocols in the routine histopathology and cytology practice in a tertiary care centre with an objective of directly benefiting the patient management and also to study the clinico-radiological features of the disease.
Materials and Methods
This was a prospective study carried out at a tertiary care centre, between 1 January 2014 and 30 June 2015, after approval by the hospital’s ethics committee (Ref:D-1213181-181). Fifty two clinically and radiologically suspected cases of lung cancer having non-small cell morphology on biopsy and/or cytology were included in the study whereas cases showing clear cut morphological features of small cell lung carcinoma were excluded. Also, cases having known primary elsewhere and showing metastatic lung involvement on High-resolution Computed Tomography (HRCT) lung were excluded. Clinical and radiological findings of included cases were noted.
NSCLCs were further classified into the subtypes based on morphology.
A limited immunohistochemistry panel comprising of TTF1/Napsin A (Adenocarcinoma), P63 (Squamous cell carcinoma) and NCAM (small cell carcinoma in discordant cases) was used in those cases which could not be subtyped based on morphology alone. The antibodies used were as follows:
Napsin A (Clone IP64)-Biogenex, prediluted;
TTF-1 (Clone 8G7G3/1)-Biogenex, prediluted;
P63 (Clone 4A4)-Biogenex, prediluted;
NCAM (Clone 123C3)-Dako, prediluted;
Calretinin (Polyclonal)-Biogenex, prediluted;
Pan-CK (Clone AE1/AE3) Biogenex, prediluted.
Results
The present study included 52 cases of NSCLC received in surgical pathology and cytology section as bronchoscopic biopsy and cytology samples (brushings, BAL, FNAC).
Population at risk admitted during the study period of 1.5 years was 29261. Number of new cases of NSCLC during that period was 52. Using this data, incidence rate was calculated as 1.78 per 1000 per 1.5 years.
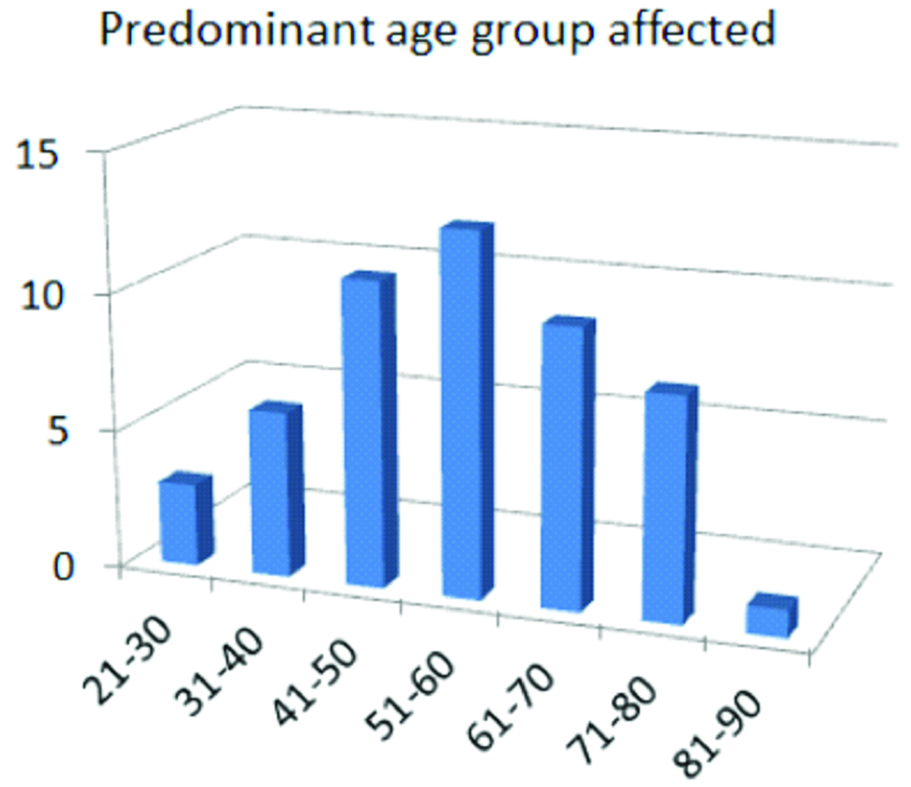
The age range of patients was found to be 25-85 years with an average age of 56.13 years. The average age for males (61.36 years) was found to be higher than that of females (49 years). Predominant age group affected was 51-60 years followed by 41-50 years [Table/Fig-1].
Age distribution of cases of NSCLC (X axis-age groups, y axis-number of cases).
Of the total 52 cases, there were 30 males and 22 females. Male to Female ratio was 1.36:1, indicating slight male preponderance.
History of past or present tobacco addiction was found among 29 out of 52 cases of NSCLC. In those with tobacco addiction, most common NSCLC was squamous cell carcinoma (n=14, 48%), closely followed by adenocarcinoma (n=12, 41%). In those without tobacco addiction, adenocarcinoma cases (n=15, 65%) far exceeded squamous cell carcinoma cases (n=7, 30%).
Cough, dyspnea and weight loss were the most frequent findings. Clinical findings are summarised in the [Table/Fig-2]:
Clinical features of NSCLC cases.
| Clinical Feature | Frequency | Percentage (%) |
|---|
| Dyspnea, breathlessness | 44 | 85 |
| Weight loss | 42 | 81 |
| Cough | 42 | 81 |
| Fever | 28 | 54 |
| Chest pain | 26 | 50 |
| Haemoptysis | 19 | 37 |
| Clinically detectable lymphadenopathy | 19 | 37 |
| Pleural effusion | 18 | 35 |
| Clubbing | 6 | 12 |
| Superior vena cava syndrome | 4 | 8 |
| Endocrine symptoms | 3 | 6 |
All the cases presented with solid nodule or mass lesion, no ground-glass opacity was encountered. A total of 80.76% of cases (n=42) showed a single lesion in one lobe. A total of 15.38% of cases (n=8) showed multiple nodules in the same lobe whereas 3.84% (n=2) showed involvement of contralateral lung.
Right side of lung (n=36) was more frequently affected than left (n=14) with right to left ratio of 2.6:1. Two cases were reported having involvement of two lobes. On HRCT (High-Resolution Computed Tomography chest), all tumours were found to be more than 2 cm in size. 90% of tumours (n=47) were between 2 cm to 7 cm in size and 10% (n=5) of tumours exceeded 7 cm in size. 60% of tumours (n=31) were peripheral in location while 40% (n=21) were centrally located.
All tumours showed involvement of ipsilateral hilar/intrapulmonary nodes. 65% of cases (n=34) showed extrapulmonary lymph node involvement. Apart from lymph nodes, features suggestive of metastasis were found in following organs: Liver (n=4), Vertebrae (n=3), Adrenals (n=2) and CNS (n=1). Features suggestive of lymphangitis carcinomatosa were seen in two cases (one squamous cell carcinoma and one adenocarcinoma).
Histology and cytology were used as complementary methods. 42 out of 52 cases were subclassified based on morphology alone. 46% of cases (n=24) showed obvious features of adenocarcinoma and were classified as such, whereas 34% of cases (n=18) could be classified as squamous cell carcinoma based on their morphological features. Ten cases showed poorly differentiated morphology, hence were subjected to immunohistochemistry. After IHC, three out of those ten cases showed positivity for P63 and were negative for Napsin-A. Hence they were classified as NSCLC favour squamous cell carcinoma. Three cases showed positivity for Napsin A and negativity for p63. Two out of these three cases were positive for TTF-1. They were classified as NSCLC-favour adenocarcinoma. Two cases which could not be put into either subgroup had a poorly differentiated morphology and showed negativity for P63, Napsin-A and had only focal weak positivity for TTF-1. NCAM was used to rule out small cell carcinoma. Both cases gave strong membranous positivity for NCAM and hence were classified as small cell carcinoma. Two cases were negative for all the markers (P63, Napsin-A, TTF-1, Calretinin, and NCAM) except Pan-CK which confirmed their epithelial origin. They were classified as NSCLC-NOS [Table/Fig-3,3,4,5,6,7,8 and 9].
Adenocarcinoma: cytology (A-H&E, 40x) and biopsy (B-H&E, 40x). Brush cytology smears showing clusters of cells with hyperchromatic crowded nuclei, showing acinar formation at places, set in a mucinous background. Biopsy shows adenocarcinoma with evidence of mucin production.

Squamous cell carcinoma: cytology (A-PAP, 40x) and biopsy (B-H&E, 40x). FNAC shows irregular clusters of keratinized malignant cells showing hyperchromatic angular and elongated oval nuclei. Biopsy shows a well differentiated squamous cell carcinoma.

Non-small cell carcinoma favour squamous cell carcinoma. Biopsy (A-H&E, 40x) shows a tumour with poorly differentiated morphology requiring IHC. IHC for P63 (B, 40x) shows nuclear positivity. Napsin A was negative in this case.

Non-small cell carcinoma favour adenocarcinoma. Biopsy (A-H&E, 40x) shows a tumour obscured by crush artefact requiring IHC for subtyping. Tumour showed positivity for Napsin A (B, 40x) while negativity for P63.

Small cell carcinoma. Biopsy (A-H&E, 40x) shows a poorly differentiated tumour. Tumour showed positivity for NCAM (B, 40x) while negativity for Napsin A. TTF-1 was focally positive. P63 was negative.

Non-small cell carcinoma-NOS. Biopsy (A-H&E, 40x) shows a poorly differentiated tumour. Tumour showed positivity for Pan-CK (B-40x) while negativity for Napsin A, TTF-1, P63, NCAM and Calretinin.

Distribution of cases according to subtype.

Discussion
Non-small cell carcinoma has gained much attention from the scientific community in the last few years. The shift towards personalised therapy has significantly changed the approach of the pathologist towards lung biopsies and cytology both in terms of diagnosis and tissue management. The demographic and epidemiological profile of the tumour is also constantly changing due to changes in the environmental factors, genetic factors and personal habits. Lung cancer is no longer a disease exclusive to the smokers or the elderly and more and more data is being gathered regarding its prevalence among non-smokers [2].
This study found a higher percentage of patients younger than 40 years of age (17.3%) as compared to the findings of other prominent Indian studies like Rawat J et al., (9.86%) and Malik PS et al., (8.92%) [3,4]. Mean age of 56.13 years matched closely with that obtained by Malik PS et al (55 years) [4] and Dubey N et al (58.6 years) [3,5]. The most common age group was 51-60 years which matched closely with most of the studies [3-5].
Present study showed only a slight male preponderance of 1.36:1. Some studies, most notably those done by Rawat J et al., and Dubey N et al., reported a much higher male preponderance with ratios of 8.2:1 and 4.2:1 respectively [3,5].
History of past or present tobacco use was observed in 55.76% of patients which is considerably less when compared to the findings of Rawat J et al., (81.77%), Malik PS et al., (68%) and Dubey N et al., (78.7%) [3-5]. Many recent worldwide studies have reported a spike in the reported cases among non-smokers and lung cancer is no longer considered a ‘smoker’s disease’. Adenocarcinoma was the commonest carcinoma among ‘never-smokers’ [2]. One large study by Yang P et al., found Adenocarcinoma to be commonest carcinoma among both smokers and never-smokers [6].
Dyspnea was the commonest symptom observed in the study (85%) followed by cough and weight loss (both 81%). These were the most frequently observed symptoms in most of the studies [3,5].
On radiological examination, right side of lung was more frequently involved than the left with right to left ratio of 2.6:1. This correlated well with most of the studies. Bilateral involvement of lungs seen in 3.84% of cases which was only slightly higher than the findings of Rawat J et al., (2.96%) [3].
In the present study, all the cases presented as solid nodule or mass lesion. Many studies including Dubey N et al., Alamoudi OS. reported mass lesion to be most common finding on radiology [5,7].
Apart from lymph node which was the commonest site of metastasis, liver was the most common site of extra-thoracic metastasis.
Adenocarcinoma (51.92% including NSCLC favour adenocarcinoma) was the commonest NSCLC encountered which correlated closely with the findings of Malik PS et al., (37.3%) and Yang P et al., (45.3%) [4,6]. Rawat J et al., and Gunjaliya A et al., reported higher incidence of squamous cell carcinoma at 62.5% and 44.83% respectively [3,8].
All these studies grouped some cases under large cell carcinoma. The latest classification by IASLC/ATS/ERS has discouraged the use of this terminology and instead advocated the use of NSCLC–Not Otherwise Specified for tumours without clear-cut morphological features or IHC profile of either adenocarcinoma or SCC [1]. In the present study, only 3.84% of cases were reported as NSCLC NOS after they showed negativity to all the markers except Pan-CK. Two unusual cases which had a poorly differentiated morphology showed positivity for CD56 and negativity for Napsin A and P63. These were classified as small cell carcinoma. However, overt morphological features of small cell carcinoma like nuclear moulding, crush artefacts, high mitotic rate and necrosis were missing. This can be considered a limitation of small biopsies where only a small area can be sampled which may not be representative of the entire tumour mass.
In this study a combination of Napsin-A and TTF-1 was used for more accurate diagnosis of lung adenocarcinoma. Napsin A is reported to have a higher sensitivity and specificity as compared to TTF-1 for diagnosis of primary lung adenocarcinoma [9] and many studies have advocated the use of combination of these two markers [10,11]. In the present study out of three adenocarcinoma cases which were diagnosed using this combination, two cases showed positivity for both markers while in one case TTF-1 was negative. Focal TTF-1 positivity was also seen in cases which were eventually diagnosed as small cell carcinomas due to NCAM positivity, highlighting the fact that using TTF-1 alone can sometimes be misleading.
Limitation
Although the study could subtype majority of the cases of NSCLC, further molecular studies like EGFR mutation studies and testing for EML4-ALK fusion gene were not attempted as part of the study due to financial constraints.
Many cases belonging to remote and rural areas were unfortunately lost to follow-up; hence no comment could be made on the overall prognosis in different subtypes of NSCLC.
Conclusion
In our experience in a tertiary care centre, using the latest classification and guidelines proposed by International association for the study of lung cancer, American thoracic society and European respiratory society, it was possible to subtype all the cases of non-small cell lung carcinoma in bronchoscopic biopsies while restricting the subgroup of NSCLC-NOS to just two cases, using routine diagnostic procedures and a limited immunohistochemistry panel and also saving the tissue for molecular studies.