Duplication of Superior Vena Cava with Atrial Termination of Right Hepatic Vein in Tetralogy of Fallot: A Rare Association
Ansul Kumar1, Ajit Padhy2, Vijay Gupta3, Arpita Rai4
1 Assistant Professor, CTVS/RIMS, RANCHI, Jharkhand, India.
2 Assistant Professor, CTVS/VMMC/SJH, New Delhi, India.
3 Professor and Head, CTVS/RML/PGIMER, New Delhi, India.
4 Assistant Professor, OMR/Faculty of Dentistry/JMI, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ansul Kumar, Flat No-68, D;DDA Flats, Pocket A, Sukhdev Vihar, New Delhi-110025, India.
E-mail: docansul@gmail.com
Anomalous hepatic venous drainage into the right atrium in association with Tetralogy of Fallot (TOF) is a rare presentation. Here, authors present a very interesting case of anomalous hepatic venous drainage into the right atrium. A 23-year-old patient presented with vascular combination of duplication of Superior Vena Cava (SVC) with an atrial termination of Right Hepatic Vein (RHV) in TOF. Separate cannulation and looping were required to have a better venous drainage while performing the intracardiac procedures through right atrium on cardiopulmonary bypass. This was the first case of this kind reported in the literature.
Cyanosis, Hepatic venous drainage, Persistent left sided superior vena cava
Case Report
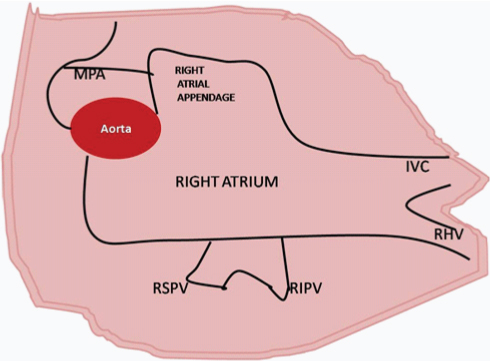
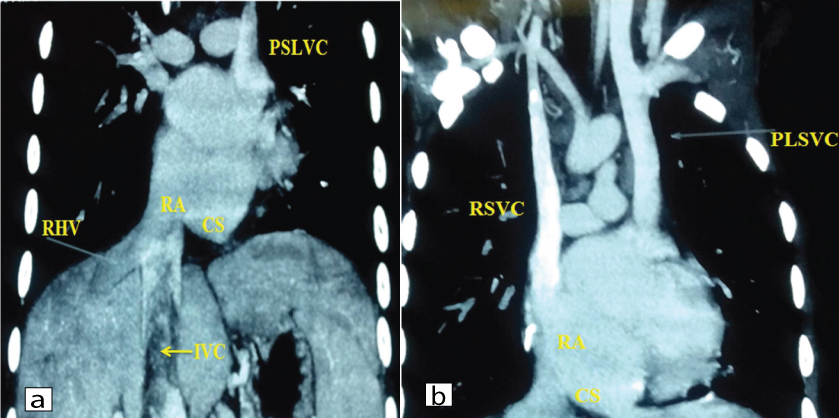
A 23-year-old male presented with cyanosis and reduced physical activity since childhood. The patient complained of breathlessness/dyspnea on exertion for the last two months. On examination the patient had a silent precordium with a loud pulmonary component of a second heart sound (P2). Chest radiograph showed a normal sized heart, dilated superior mediastinum and normal lung parenchyma. A 2-D ECHO and cath study affirmed TOF with abnormal Persistent Left Sided Superior Vena Cava (PLSVC) draining into the coronary sinus. Intracardiac repair was planned for the patient. On the operating table, there was an additional vessel on the left side, apart from PLSVC, which was presumed to be left Inferior Vena Cava (IVC). This vessel detected intraoperatively had a smaller lumen than the right IVC and was draining directly into the right atrium as two separate opening adjacent to the dilated coronary sinus [Table/Fig-1]. All four cavae (both side SVC and IVC) were cannulated and looped separately during intracardiac repair. The patient had an uneventful recovery and discharged on 5th postoperative day. In the follow-up, he was further investigated for the anomalous venous drainage into the right atrium. High-resolution ultrasonography of the whole abdomen and contrast-enhanced computed tomography of the abdomen and thorax ruled out double IVC, however surprisingly, revealed an anomalous RHV draining directly into Right Atrium (RA) and a massive dilation of the coronary sinus at the inferior surface of heart with a presence of PLSVC [Table/Fig-2]. Thus, the anomalous vessel detected intraoperatively was not left IVC but, in fact, the RHV draining into the right atrium.
Diagram showing intraoperative finding of draining of Right Hepatic Vein (RHV) and Inferior Vena Cava (IVC) into the Right Atrium (RA) through two separate openings.
MPA: Main Pulmonary Artery; RSPV: right superior pulmonary vein; RIPV: Right Inferior Pulmonary Vein
a) CECT thorax showing the RHV draining directly into RA and a massive dilation of the CS at the inferior surface of heart with a presence of PLSVC; b) Coronal reformatted Maximum Intensity Projection (MIP) view showing PLSVC and RSVC draining into RA.
Discussion
Venous anomalies mainly result from errors of the embryological development. Such anomalies associated with congenital heart disease are common and have been described extensively by anatomists, radiologists and surgeons operating in this region. The presence of anomalous right hepatic vein draining directly into the right atrium in TOF has not been reported previously.
Anomalous hepatic venous drainage into the right atrium is known to coexist with atrial isomerism, abdominal heterotaxy, and absence of the IVC however, its association with TOF is a unique finding [1]. TOF is previously reported in association with pulmonary artery atresia, right-sided aortic arch (25% of cases), atrial septal defect (10% of cases) and coronary artery abnormalities (10% of cases) [2]. TOF has less commonly been reported in association with PLSVC and aberrant right subclavian artery [3]. The indexed case seems to be the first reported vascular combination of duplication of SVC with an atrial termination of RHV in TOF.
These anomalies have plenty of clinical implications from the surgical point of view. Placement of a central venous catheter through the PLSVC poses difficulties like possible perforation of the LSVC wall, hypotension, cardiogenic shock, cardiac tamponade or cardiac arrest [4]. Cardiac surgery in such patients may be associated with complications. To avoid the risk at surgery, the PLSVC may be reanastomosed to the right atrium, or clamped or ligated. In our case, we selectively cannulated the LSVC and drained it to venous reservoir. Also, the RHV had to be selectively cannulated so that venous drainage is not compromised and there is no postoperative hepatic congestion or right ventricular dysfunction.
PLSVC is seen in 3-5% of congenital heart disease patients [5]. PLSVC has been reported in association with congenital heart defects like atrial septal defects, ventricular septal defects, D-transportation of the great vessels, pulmonary stenosis/atresia, mitral atresia, anomalous pulmonary drainage, tetralogy of fallot, coarctation of the aorta, absent right SVC, situs inversus, coronary sinus atresia/enlargement, subaortic stenosis [6]. The anterior cardinal veins, draining the head, neck, and arm, unite with the posterior cardinal vein in the early embryonic stage and enter the heart as the right and left horns of the sinus venosus [7]. Only the coronary sinus and a remnant known as the ligament of Marshall (oblique vein of left atrium) remains after embryonic development is complete. PLSVC results from failure of obliteration of the left anterior cardinal vein and drains into the right atrium via the coronary sinus.
Inferior vena cava develops from three pairs of postcardinal, supracardinal, and subcardinal veins. These veins give rise to IVC as well as hepatic veins, bilateral vitelline and umbilical veins [3]. Aberration in the drainage of the right vitelline hepato cardiac vein may lead to right hepatic vein drainage into the right atrium since it normally forms a terminal portion of IVC, and receives right and left hepatic veins [5].
Similar cases of aberrant hepatic drainage into the right atrium has been previously reported [6,8-11]. Duplication of the SVC, associated with an aberrant Left Hepatic Vein (LHV), has been reported in one of the 58 dissected specimens by Milisavljevic M et al., [12].
TTE is the mainstay tool for diagnosing PLSVC and anomalous venous drainage into the right atrium. It also rules out associated cardiac anomalies. Echo was poor at delineating the insertion site of the PLSVC. Agitated saline bubble study via the left brachial vein is often necessary to establish the diagnosis [7,13]. A contrast chest CT scan offers more information in delineating the anatomy and aids in surgical planning. As demonstrated by the present case, a contrast chest CT contributed the important finding of drainage of RHV directly into RA and a massive dilation of the Coronary Sinus (CS) at the inferior surface of heart with the presence of PLSVC. Computed tomography, angiography and magnetic resonance angiography show the complete extent of the vascular anomaly.
Conclusion
Anomalous venous drainage into the right atrium is common; however, they are sometimes discovered on the operating table only. A contrast chest CT helps in planning the operation. Separate cannulation and looping was required to have a better venous drainage while performing the intracardiac procedures through right atrium on cardiopulmonary bypass. Duplication of the superior vena cava with the atrial termination of the right hepatic vein in tetralogy of fallot is a rare association.
[1]. D’Cruz I, Smith K, Echocardiographic appearances of direct drainage of hepatic vein into right atrium in adultsEchocardiography 1995 12(5):465-68.10.1111/j.1540-8175.1995.tb00837.x [Google Scholar] [CrossRef]
[2]. Boechat M, Ratib O, Williams P, Gomes A, Child J, Allada V, Cardiac MR imaging and MR angiography for assessment of complex tetralogy of Fallot and pulmonary atresiaRadioGraphics 2005 25:1535-46.10.1148/rg.25604505216284133 [Google Scholar] [CrossRef] [PubMed]
[3]. Dabizzi R, Teodori G, Barletta G, Caprioli G, Baldrighi G, Baldrighi V, Associated coronary and cardiac anomalies in the tetralogy of Fallot: an angiographic studyEur Heart J 1990 11:692-704.10.1093/oxfordjournals.eurheartj.a0597842397733 [Google Scholar] [CrossRef] [PubMed]
[4]. Erdogan M, Karakas P, Uygur F, Mese B, Yamak B, Bozkir MG, Persistent left superior vena cava. The anatomical and surgical importanceWest Indian Med J 2007 56:72-76.10.1590/S0043-3144200700010001317621848 [Google Scholar] [CrossRef] [PubMed]
[5]. Embryology, vitello umbilical veins and cardinal venous complexes. In Gray’s anatomy. Williams P, Warwick R, Dyson M, Bannister L. Churchill Livingstone (1989), 37th edition, 222 [Google Scholar]
[6]. Buehler M, Abdullah A, Lewis TJ, Left hepatic vein and persistent left superior vena cava drainage into the coronary sinus with subaortic valve stenosisThe International Journal of Angiology: Official Publication of the International College of Angiology, Inc 2011 20(4):243-46.10.1055/s-0031-128420423204826 [Google Scholar] [CrossRef] [PubMed]
[7]. Dearstine M, Taylor W, Kerut E, Persistent left superior vena cava: chest X-ray and echocardiographic findingsEchocardiography 2000 17:453-55.10.1111/j.1540-8175.2000.tb01164.x10979021 [Google Scholar] [CrossRef] [PubMed]
[8]. Bhatti S, Hakeem A, Ahmad U, Malik M, Kosolcharoen P, Chang SM, Persistent left superior vena cava (PLSVC) with anomalous left hepatic vein drainage into the right atrium: role of imaging and clinical relevanceVasc Med 2007 12(4):319-24.10.1177/1358863X0708485918048468 [Google Scholar] [CrossRef] [PubMed]
[9]. Azuma C, Tohno Y, Tohno S, Moriwake Y, Utsumi M, Yamada M, Persistent left hepatic venous connection with the right atrium and the ductus venosusAnat Sci Int 2002 77(2):124-27.10.1046/j.0022-7722.2002.00001.x12418092 [Google Scholar] [CrossRef] [PubMed]
[10]. Stoller JK, Hoffman RM, White RD, Mee RB, Anomalous hepatic venous drainage into the left atrium: an unusual cause of hypoxemia: Case reportRespir Care 2003 48:58-62. [Google Scholar]
[11]. Masuko S, Inoue K, A case of the double superior venae cavae and an anomalous left hepatic vein opening directly into the right atriumKaibogaku Zasshi 1982 57:169-74. [Google Scholar]
[12]. Milisavljevic M, Marinkovic S, Radak D, Cetkovic M, Vucurevic G, Trifunovic D, Duplication of the superior vena cava associated with atrial termination of the left hepatic veinPhlebology 2013 28(7):369-74.10.1258/phleb.2012.01115622865421 [Google Scholar] [CrossRef] [PubMed]
[13]. Sarodia B, Stoller J, Persistent left superior vena cava: case report and literature reviewRespir Care 2000 45:411-26. [Google Scholar]