Hepatic Hydrothorax without Apparent Ascites and Dyspnea - A Case Report
Jing He1, Rasha Haykal2, Hongchuan Coville3, Jaya Prakash Gadikota4, Christopher Bray5
1 Resident, Department of Internal Medicine, University of Central Florida College of Medicine, Graduate Medical Education, Orlando, FL, U.S. 32827.
2 Senior Resident, Department of Internal Medicine, University of Central Florida College of Medicine, Graduate Medical Education, Orlando, FL, U.S. 32827.
3 Resident, Department of Internal Medicine, University of Central Florida College of Medicine, Graduate Medical Education, Orlando, FL, U.S. 32827.
4 Attending Physician, Department of Internal Medicine, North Florida Regional Medical Center, Internal Medicine Residency Program, Gainesville, FL, U.S. 32605.
5 Professor, Department of Internal Medicine, University of Central Florida College of Medicine, Graduate Medical Education, Orlando, FL, U.S. 32827.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jing He, 1505 Fort Clarke Blvd, Apt 14204, Gainesville, FL 32606.
E-mail: jing.he@hcahealthcare.com
A 78-year-old female with a past medical history of alcoholic cirrhosis was hospitalised with recurrent lower gastrointestinal bleeding due to rectal ulcers. The ulcers were successfully treated with cautery and placement of clips. However, a recurrent large right-sided pleural effusion without apparent ascites and dyspnea were found incidentally during the hospitalisation. The initial fluid analysis was exudate based on Light’s criteria with high protein. The fluid analysis was repeated five days later, after rapid reaccumulation which revealed transudates. Other causes of pleural effusion like heart failure, renal failure or primary pulmonary diseases were excluded. Hepatic hydrothorax was considered and the patient was started with the treatment of Furosemide and Spironolactone. The atypical presentation of hepatic hydrothorax may disguise the diagnosis and delay the treatment. Therefore, for a patient with recurrent, unexplained unilateral pleural effusions, even with atypical fluid characterisation and in the absence of ascites, hepatic hydrothorax should still remain on the top differential with underlying cirrhosis to ensure optimal treatment.
Cirrhosis, Light criteria, Liver, Pleural effusion
Case Report
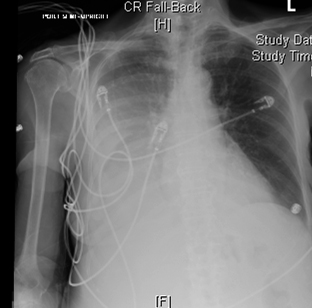
A 78-year-old Caucasian female, with a past medical history of alcoholic cirrhosis, admitted for recurrent rectal bleeding secondary to rectal ulcers and was successfully treated with cautery and placement of clips. However, a recurrent massive right-sided pleural effusion without apparent ascites or dyspnea was found incidentally during the hospitalisation [Table/Fig-1]. Liver ultrasound findings were consistent with cirrhosis. Chest and abdominal CT were performed as a follow-up, which confirmed a large right-sided pleural effusion. There were no additional abnormal findings identified on CT, no acute infiltration, pulmonary oedema, pleural thickening or malignant disease, nor ascites. Oxygen saturation was 98% on room air for the patient. She had no leukocytosis or elevated hepatic transaminases [Table/Fig-2]. Renal function and electrolytes were also in the normal range [Table/Fig-2]. Hepatitis B and hepatitis C tests were negative. Coagulation tests were normal [Table/Fig-3]. The Echocardiogram showed normal heart function with Left Ventricular Ejaculation Fraction (LVEF) of 60% with no evidence of pericardial effusion. NT-proBNP was in the normal range.
An ultrasound-guided diagnostic thoracentesis was performed. Pleural fluid profile was consistent with an exudate based on Light’s criteria, with apleural protein of 4.9 mg/dL and pleural/serum protein ratio of 0.66. Gram stain and fluid culture were negative. Cytology did not reveal any malignant cells. A right-sided chest tube was placed with evacuation of about 1.35 L of fluid. However, the massive pleural effusion reaccumulated 5 days later. An ultrasound-guided chest tube was again placed based on prior diagnostics. The pleural effusion was drained, producing 4L. Repeated fluid analysis showed a protein level of 2.2 mg/dL, fluid /serum protein ratio of 0.42, pleural/serum LDH ratio of 0.53, cholesterol < 50, serum-ascites albumin gradient >1.2 g/dL [Table/Fig-4]. The repeat fluid was a transudate via Light’s criteria. Hepatic hydrothorax was considered and she was started on treatment with sodium restriction along with Furosemide 20mg and Spironolactone 50mg. She was maintained on diuretics at discharge. Four months later her chest X-ray showed stable small to moderated effusion but not as large as before. Since she had been asymptomatic, she was advised for palliative thoracentesis if she has shortness of breath.
Large right pleural effusion. The cardiomediastinal silhouette is within normal limits. Boney structure is unremarkable.
Complete blood count and blood chemistry.
| Haemogram | Levels | Normal range |
|---|
| WBC | 6.9 | (4.5-11.0 thousands/mm3) |
| Neutrophils % | 78 H | (50.0-75.0 %) |
| Lymphocytes % | 11.6 L | (17.0-42.0 %) |
| Monocytes % | 7.6 | (4.0-11.0 %) |
| Eosinophils % | 1.7 | (0.4-6.0 %) |
| Basophils % | 1.1 | (0.0-2.0 %) |
| Absolute Neutrophil Count | 5.4 | (1.5-8 thousands/mm3) |
| RBC | 2.56 | (3.80-5.20 million cells/uL) |
| Hgb | 7.6 L | (12.0-15.0 g/dL) |
| Hct | 22.3 L | (35.0-49.0 %) |
| MCV | 86.8 | (80.0-100.0 fL) |
| MCH | 29.7 | (26.5-34.0 pg) |
| MCHC | 34.3 | (32.0-36.0 %) |
| RDW | 17.1 | (<17.0 %) |
| Platelet Count | 80 L | (150 - 450 thousands/mm3) |
| MPV | 8.8 | (6.6-10.2 fL) |
| Chemistry | | |
| Sodium | 141 | (136-145 mmol/L) |
| Potassium | 4.2 | (3.5-5.1 mmol/L) |
| Chloride | 114 H | (98-107 mmol/L) |
| Carbon Dioxide | 19 L | (21-32 meq/L) |
| Total Bilirubin | 1.8 H | (0.2-1.0 mg/dL) |
| AKP | 46 | (45-117 units/L) |
| AST | 14 L | (15-37 units/L) |
| ALT | 12 | (13-56 units/L) |
| Total Protein | 4 | (6.4-8.2 g/dL) |
| Albumin | 1.8 | (3.4-5.0 g/dL) |
| Globin | 2.2 | (2.8-4.4 g/dL) |
| A/G Ratio | 0.8 | (1.3-2.8) |
| BUN | 20 H | (7-18 mg/dL) |
| Creatinine | 1.13 | (0.60-1.30 mg/dL) |
| Glucose | 129 H | (74-106 mg/dL) |
| Calcium | 7.5 L | (8.5-10.1 mg/dL) |
| Phosphorus | 3.7 | (2.5-4.9 mg/dL) |
| Magnesium | 1.8 | (1.8-2.4 mg/dL) |
| NT-Pro-BNP | 228 | (0-900 pg/mL) |
| GFR | 46 | 90-120 mL/min/1.73 m2 |
| BUN/CREA | 17.7 | (9.3-24.4 ratio) |
Abbreviations: WBC: White Blood Cell Count; RBC: Red Blood Cell Count; Hbg: Haemoglobin; Hct: Hematocrit; MCV: Mean Corpuscular Volume; MCH: Mean Corpuscular Haemoglobin; MCHC: Mean Corpuscular Haemoglobin Concentration; RDW: Red Cell Distribution Width; MPV: Mean Platelet Volume; BUN: Blood Urea Nitrogen; GFR: Glomerular Filtration Rate;
| Coagulation |
|---|
| PT | 12.4 | (9-12.5 SEC) |
| INR | 1.2 | |
| APTT | 25 | (21-35 SEC) |
Abbreviations: PT: Prothrombin Time, INR: International Normalized Ratio, APTT: Activated Prothrombin Time
| 1st fluid analysis | 2nd fluid analysis | Transudate | Exudate |
|---|
| Color | Yellow, clear | Yellow, clear | Clear | Cloudy |
| PH | 7.41 | 7.36 | 7.40 to 7.55 | <7.40 |
| WBC | 106 | 126 | < 1000 | > 1000 |
| SEG Neutrophils | 2 | 2 | | |
| Lymphocytes | 26 | 26 | | |
| Eosinophils | - | 4 | | |
| Basophils | - | 1 | | |
| Monocyte/Macrophage | 72 | 67 | | |
| Glucose | - | 101mg/dL | > 60 mg/dL | < 60 mg/dL |
| Protein mg/dL | 4.9 | 2.2 | < 3 g/dL | > 3 g/dL |
| Pleural protein /serum protein | 0.66 | 0.42 | < 0.5 | > 0.5 |
| SAAG | - | 1.4 | > 1.2 g/dL | < 1.2 g/dL |
| Pleural LDH /serum LDH | 0.54 | 0.42 | < 0.6 | > 0.6 |
| Cholesterol | - | < 50 | <50 | >50 |
| Pathology | No malignant cells | No malignant cells | | |
Abbreviations: LDH: Lactate dehydrogenase;
SAAG: serum-ascites albumin gradient
Discussion
Hepatic hydrothorax occurs in approximately 5% to 10% of patients with cirrhosis, and the outcome is usually very poor [1]. A few cases of hepatic hydrothorax in the absence of ascites were reported before [2,3]. Here, we presented a rare case with an incidental finding of recurrent massive right-sided pleural effusion in the absence of ascites. The initial fluid analysis was exudate based on Light’s criteria. These atypical presentations made the diagnosis and treatment even more challenging.
The diagnosis of hepatic hydrothorax is based on the presence of a pleural effusion (usually >500 mL) in a patient with cirrhosis by excluding other underlying primary cardiopulmonary causes [4]. The pleural effusion probably results from diaphragmatic defects, allowing the ascites to move from the peritoneal cavity into the pleural cavity [5]. However, the presence of ascites is not necessary for the diagnosis. This may be due to the negative intrathoracic pressure generated during inspiration [6]. An intraperitoneal injection of 99mTc-sulphur colloid or 99mTc-human serum albumin may be helpful if the diagnosis is unclear [7].
Diagnostic thoracentesis of the pleural fluid is required, which is classically found to be a transudate. Light’s criteria are the most widely used criteria for fluid analysis. Although the sensitivity of Light’s criteria for a diagnosis of exudates is as high as 98%, the specificity is only about 80% [8]. Furthermore, it was reported that about 18% of hepatic hydrothorax was misclassified as exudates based on the Light’s criteria [9]. Thus, clinical judgment is required when evaluating patients with borderline test results. With respect to the patient we presented here, the first fluid analysis was an exudative process via Light’s criteria with high protein level, although the other biochemistry markers including LDH ratio, glucose level, cell counts and pH indicated a transudate. More recent studies have examined other characteristics of pleural fluid that may help to determine whether the effusion is exudate or transudate, like Serum-Ascites Albumin Gradient (SAAG). The combined use of Light criteria and the albumin gradient may significantly increase the specificity [9,10].
Chest tube placement is a common treatment for large pleural effusion, however, it was reported that patients with hepatic hydrothorax who were treated with chest tube actually had higher mortality and longer length of stay compared to those who underwent thoracentesis [11,12]. Chest tube placement is associated with many severe complications in patients with hepatic hydrothorax, like acute kidney injury, pneumothorax, haemothorax, empyema, unilateral pulmonary oedema due to the rapid removal of fluid. Therefore, a chest tube is a relative contraindication for the treatment of hepatic hydrothorax and should be avoided whenever feasible.
The initial therapy for hydrothorax includes low sodium diet and diuretics. Furthermore, therapeutic thoracentesis can be attempted if diuretics are not effective. Transjugular Intrahepatic Portosystemic Shunt (TIPS) placement can be considered for refractory hepatic hydrothorax [13]. Eventually, all patients with confirmed hepatic hydrothorax should be considered for evaluation of liver transplantation.
Conclusion
We presented a rare case of hepatic hydrothorax in the absence of ascites. The absence of ascites may be due to the negative intrathoracic pressure generated during inspiration. This atypical presentation may disguise the underlying diagnosis. Therefore, for patients with underlying cirrhosis presented with unexplained unilateral pleural effusions, hepatic hydrothorax should always remain on the top differential to provide optimal treatment. Currently, initial treatment of hepatic hydrothorax includes sodium restriction and diuretics to increase kidney excretion. Refractory pleural effusion may require serial thoracentesis. Indeed, chest tube for prolonged aspiration should be avoided due to the complications and poor outcome in these patients.
Disclaimer: This research was supported (in whole or in part) by HCA and/or an HCA affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA or any of its affiliated entities.
Abbreviations: WBC: White Blood Cell Count; RBC: Red Blood Cell Count; Hbg: Haemoglobin; Hct: Hematocrit; MCV: Mean Corpuscular Volume; MCH: Mean Corpuscular Haemoglobin; MCHC: Mean Corpuscular Haemoglobin Concentration; RDW: Red Cell Distribution Width; MPV: Mean Platelet Volume; BUN: Blood Urea Nitrogen; GFR: Glomerular Filtration Rate;
Abbreviations: PT: Prothrombin Time, INR: International Normalized Ratio, APTT: Activated Prothrombin Time
Abbreviations: LDH: Lactate dehydrogenase;
SAAG: serum-ascites albumin gradient
[1]. Garbuzenko DV, Arefyev N, Hepatic hydrothorax: An update and review of the literatureWorld J Hepatol 2017 9(31):1197-204.10.4254/wjh.v9.i31.119729152039 [Google Scholar] [CrossRef] [PubMed]
[2]. John S, Paul M, Murthy U, An unusual presentation of cirrhotic pleural effusion in a patient with no ascites: a case reportCases J 2009 2013:676710.4076/1757-1626-2-676719918541 [Google Scholar] [CrossRef] [PubMed]
[3]. Kim JS, Kim CW, Nam HS, Cho JH, Ryu JS, Lee HL, Hepatic hydrothorax without ascites as the first sign of liver cirrhosisRespirol Case Rep 2016 4(1):16-18.10.1002/rcr2.14026839695 [Google Scholar] [CrossRef] [PubMed]
[4]. Kinasewitz GT, Keddissi JI, Hepatic hydrothoraxCurr Opin Pulm Med 2003 9(4):26110.1097/00063198-200307000-0000312806237 [Google Scholar] [CrossRef] [PubMed]
[5]. Huang PM, Chang YL, Yang CY, Lee YC, The morphology of diaphragmatic defects in hepatic hydrothorax: thoracoscopic findingJ Thorac Cardiovasc Surg 2005 130(1):141-45.10.1016/j.jtcvs.2004.08.05115999054 [Google Scholar] [CrossRef] [PubMed]
[6]. Rubinstein D, McInnes IE, Dudley FJ, Hepatic hydrothorax in the absence of clinical ascites: diagnosis and managementGastroenterology 1985 88(1):18810.1016/S0016-5085(85)80154-2 [Google Scholar] [CrossRef]
[7]. Benet A, Vidal F, Toda R, Siurana R, De Virgala CM, Richart C, Diagnosis of hepatic hydrothorax in the absence of ascites by intraperitoneal injection of 99m-Tc-Fluor colloidPostgrad Med J 1992 68(796):15310.1136/pgmj.68.796.1531570266 [Google Scholar] [CrossRef] [PubMed]
[8]. Porcel JM, Peña JM, Vicente de Vera C, Esquerda A, Reappraisal of the standard method (Light’s criteria) for identifying pleural exudatesMedicina Clinica 2006 126(6):211-13.10.1157/1308487016510093 [Google Scholar] [CrossRef] [PubMed]
[9]. Bielsa S, Porcel JM, Castellote J, Mas E, Esquerda A, Light RW, Solving the Light’s criteria misclassification rate of cardiac and hepatic transudatesRespirology 2012 17(4):721-26.10.1111/j.1440-1843.2012.02155.x22372660 [Google Scholar] [CrossRef] [PubMed]
[10]. Tarn AC, Lapworth R, Biochemical analysis of pleural fluid: what should we measure?Ann Clin Biochem 2001 38:311-22.10.1258/000456301190081211471871 [Google Scholar] [CrossRef] [PubMed]
[11]. Ridha A, Al-Abboodi Y, Fasullo M, The outcome of thoracentesis versus chest tube placement for hepatic hydrothorax in patients with cirrhosis: a nationwide analysis of the national inpatient sampleGastroenterology Research and Practice 2017 2017:587206810.1155/2017/587206829317865 [Google Scholar] [CrossRef] [PubMed]
[12]. Orman ES, Lok ASF, Outcomes of patients with chest tube insertion for hepatic hydrothoraxHepatol Int 2009 3(4):582-86.10.1007/s12072-009-9136-z19669710 [Google Scholar] [CrossRef] [PubMed]
[13]. Dhanasekaran R, West JK, Gonzales PC, Subramanian R, Parekh S, Spivey JR, Transjugular intrahepatic portosystemic shunt for symptomatic refractory hepatic hydrothorax in patients with cirrhosisAm J Gastroenterol 2010 105(3):635-41.10.1038/ajg.2009.63419904245 [Google Scholar] [CrossRef] [PubMed]