Characterisation of Multidrug-resistant Alcaligenes faecalis Strain AF1 Isolated from Patient of RUTIs: A Study from Bangladesh
Farhana Momtaz1, MD Hazrat Ali2, MD Nazmul Hossain3, MD Javed Foysal4, Mariya Kibtiya Sumiya5, Kamrul Islam6
1 Postgraduate, Department of Microbiology, University of Chittagong, Bangladesh.
2 Assistant Professor, Department of Genetic Engineering and Biotechnology, Shahjalal University of Science and Technology, Sylhet, Bangladesh.
3 Assistant Professor, Department of Microbial Biotechnology, Sylhet Agricultural University, Sylhet, Bangladesh.
4 PhD Research Fellow, School of Molecular and Life Sciences, Curtin University, Perth, WA, Australia.
5 Postgraduate, Department of Microbiology, Jahangirnagar University, Savar, Bangladesh.
6 Professor, Department of Genetic Engineering and Biotechnology, Shahjalal University of Science and Technology, Sylhet, Bangladesh.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Md Javed Foysal, PhD Research Fellow, School of Molecular and Life Sciences, Curtin University, WA-6845, Perth, WA, Australia.
E-mail: mjfoysal-geb@sust.edu; mdjaved.foysal@postgrad.curtin.edu.au
Introduction
Alcaligenes faecalis is a common environmental bacterium that often infects human as an opportunistic pathogen. It rarely causes Urinary Tract Infection (UTI) in human; however, infection brings severe outcomes. Also, the treatment of A. faecalis associated infections with common antibiotics can be difficult due to a high level of antibiotic resistance.
Aim
Molecular characterisation of A. faecalis isolate from women suffering from Recurrent Urinary Tract Infections (RUTIs).
Materials and Methods
The study was conducted in the USDA-laboratory of the Department of Genetic Engineering and Biotechnology, Shahjalal University of Science and Technology, Sylhet, Bangladesh. The present study conducted from July 2017 to December 2017, characterised an A. faecalis strain from the women suffering from RUTIs by applying 16s rRNA gene sequencing and phylogenetic analysis. Antibiogram profiling was done by means of disk diffusion assay. Analysis of in-silico SNP variants was done using Geneious software.
Results
The isolates were resistant to seven out of ten commercial antibiotics used to treat UTI in Bangladesh. Phylogenetic and evolutionary distance data analysis revealed a close proximity of the study AF1 strain with other A. faecalis strains identified from the environment, especially from a previously characterised water sample. In-silico variants search found nine potentials of Single Nucleotide Polymorphism (SNPs) in the studied strain compared to other environmental A. faecalis bacteria characterised from India, South-Korea, Japan, Mexico and Brazil.
Conclusion
The present study revealed the transmission of environmental opportunistic pathogens to human and cause chronic infections in Bangladesh.
16s rRNA gene sequencing, Multidrug-resistant strain, Phylogenetic analysis
Introduction
Urinary tract infection is the major health concern worldwide. In women, the percentages of UTI are enormously higher as the bacteria can easily travel through the shorter urethra in quick time [1]. A number of bacteria responsible for UTI, including species of Escherichia coli, Klebsiella pneumoniae, Salmonella sp., Shigella sp., Proteus sp., Citrobacter sp., and some others from the Enterobacteriaceae group [2,3]. A. faecalis, an opportunistic pathogen from Alcaligenaceae family, commonly found in water and soil, that rarely infects human [4]. It is reported to be associated with UTI but plentiful research data is yet to be available to strongly support the statement [5,6]. Recently, a large number of multidrug-resistant A. Faecalis and Enterococcus faecalis isolates were identified from hospitalised patients in India [7,8]. In Bangladesh; however, attention only paid to the identification of E. coli and K. pneumoniae from UTI samples [9,10]. Reinfections in UTI are very common and the term is called RUTIs, caused by the same pathogen that originally causes UTI. Research reports suggested that at least 27% of women face RUTIs where 2.7% are likely to be reinfected for third time in their life [11]. RUTIs often make treatment process complicated and challenging due to re-intake of same drugs for prolonged periods, as the bacteria can produce drug resistance [12,13]. In addition, having more frequent and unsafe sexual intercourses makes women more vulnerable to RUTIs [14].
Multidrug-resistant strains produce further complicacies to UTI and RUTIs patients. A bacteria can be defined as multidrug-resistant when it shows resistance to at least three commercial antibiotics [15]. In Bangladesh, clinical bacteria have emerged as multiple drugs resistant in the last couple of decades [16]. Recently, the problem embarked when most of the commercial drugs failed to show sensitivity against many clinical isolates, including those associated with UTI [10]. Frequent use of antibiotics and improper drug doses are responsible for the evolution of more virulent isolates in this region [17]. Moreover, culture-based detection method used in Bangladesh often gives false positive results thus misleading the whole treatment and recovery process [10]. Therefore, many of the UTI causing bacteria remains uncharacterised in the culture plate.
In recent time, several molecular techniques have been successfully applied for the detection of clinically significant bacteria. Among them, 16S rRNA gene sequencing now widely used for the identification of bacterial genera due to its reliability and robustness [18]. The advancement of computer aided biological data analysis tools makes it further easy for more fast and accurate identification of bacterial species [19,20]. In spite of its worldwide acceptance, in Bangladesh, the application of 16s rRNA gene sequencing still remains at the preliminary stage. Hence, the present study was undertaken to identify one of the uncharacterised bacteria from a RUTIs patient from Sylhet city in Bangladesh.
Materials and Methods
Collection of the Bacterial Isolate
The present study was conducted from July 2017 to December 2017. The isolate was collected from Popular Medical and Diagnostic Centre, Sylhet, Bangladesh. They supplied the isolate as an uncharacterised bacteria in Nutrient Agar (NA) plate collected from women of 35 years age suffering from RUTIs, Cystitis and pregnancy complicacies. The isolate was transported immediately to USDA project laboratory of Shahjalal University of Science and Technology, Sylhet 3114, Bangladesh by maintaining the cool chain. Here, authors re-cultured the isolate in both Nutrient Broth (NB) and Nutrient Agar NA and incubated at 37°C for overnight in a rotatory shaker.
Antibiogram Assay
Antibiotic sensitivity assay was done using 10 commercial antibiotics by disk diffusion assay [21]. An overnight bacterial broth culture (30 μL) was spread in NA plate and antibiotics discs were aseptically added onto the plate and incubated overnight at 37°C. The drugs used in the study were ampicillin (AMP, 10 μg/disk), cephradine (CEP), chloramphenicol (CHL, 10 μg/disk), ciprofloxacin (CIP, 10 μg/disk), cotrimoxazole (10 μg/disk), erythromycin (ERY, 15 μg/disk), gentamycin (GEN, 10 μg/disk), streptomycin (STP, 10 μg/disk), sulphamethoxazole (SXT, 10 μg/disk) and tetracycline (TET, 10 μg/disk). The zone of inhibition was measured according to the previously described standard method [10].
DNA Extraction and PCR Amplification of 16s rRNA Gene Sequence
Bacterial genomic DNA was extracted from the overnight NB culture using the commercial DNA extraction kit (Bio Basic Inc.; Ontario, Canada). All the steps were carefully monitored and Proteinase K and RNase A were added according to manufacturer’s instructions in order to get purified DNA product. The DNA was quantified by gel electrophoresis using lambda DNA as a marker and also in a spectrophotometer as protein-DNA absorbance. PCR amplification of 16s rRNA sequences of target bacteria was done by previously stated standard method [22]. PCR master mixture was prepared for 50 μL final concentration using 2X prepared mixture (Fermentus, Gene RullerTM, USA). Others chemicals and reagents were optimised as follows: 2.5 μL of each forward (27F, 5’-AGAGTTTGATCCTGGCTCAG-3’) and reverse (1492R, 5’-GGATACCTTGTTACGACTT-3’) universal sequencing primers, 5 μL of template DNA and 15 μL of nuclease-free PCR water. A total of 30 cycles of reactions were performed in a MultiGene gradient thermal cycler (Labnet International Inc., USA). Amplified PCR product was separated by gel electrophoresis technique and visualised in a gel documentation system. The PCR product was then purified using PureLinkPCR purification kit (Thermo Scientific, USA) by following the manufacturer’s instructions. The purified product was then sent to “1st BASE” sequencing centre, Malaysia for 16s rRNA sequencing using the Sanger di-deoxy method.
Sequence Analysis Tools
After sequencing, the raw sequence was extracted and checked for quality in Chromas (v2.01). The sequence was edited in Bioedit tool (v7.0.4), assembled in SeqMan Pro (v15.0) and removed chimeras using DECIPHER (v9.20). BLASTn search tool at NCBI was used for getting highly similar nucleotide sequences of the studied strain. Other A. faecalis sequences were downloaded from NCBI nucleotide database in FASTA format for further analysis. Multiple alignments were done using muscle alignment in MEGA 7.0 and a phylogenetic tree was constructed using neighbour-joining method following Chimura-J model with 1,000 bootstrap replicates. Evolutionary divergence was calculated as p-distances in MEGA 7.0 using both transitions and trans-versions, homogenous lineages, avoiding gaps and missing data and keeping sequence uniformity.
Results
Antibiotic Sensitivity Tests
The present study found seven antibiotics were completely resistant to A. faecalis. Those are ampicillin, cephradine, erythromycin, gentamycin, streptomycin, sulphamethoxazole, and tetracycline. Chloramphenicol, cotrimoxazole and ciprofloxacin were the sensitive to A. Faecalis strain. Among these, ciprofloxacin showed highest level of sensitivity with a zone of inhibition 18 mm, followed by cotrimoxazole (14 mm) and chloramphenicol (12 mm), respectively.
Sequence Analysis
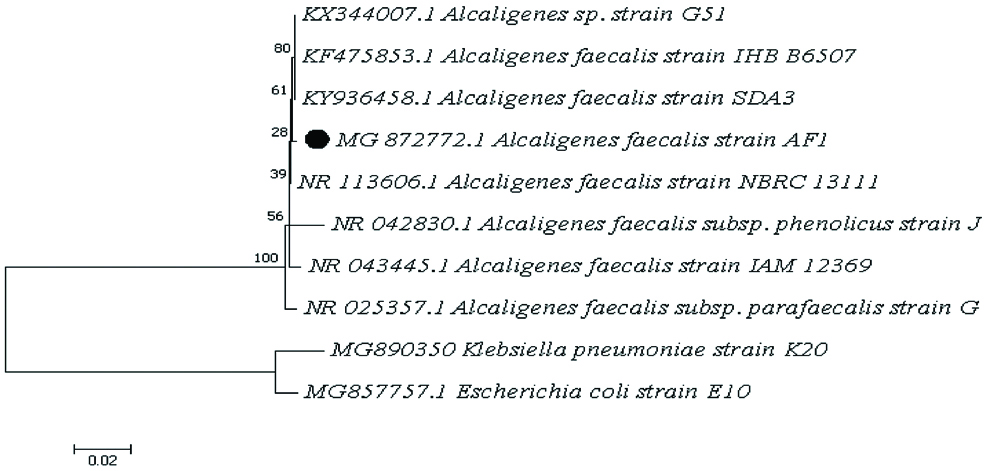
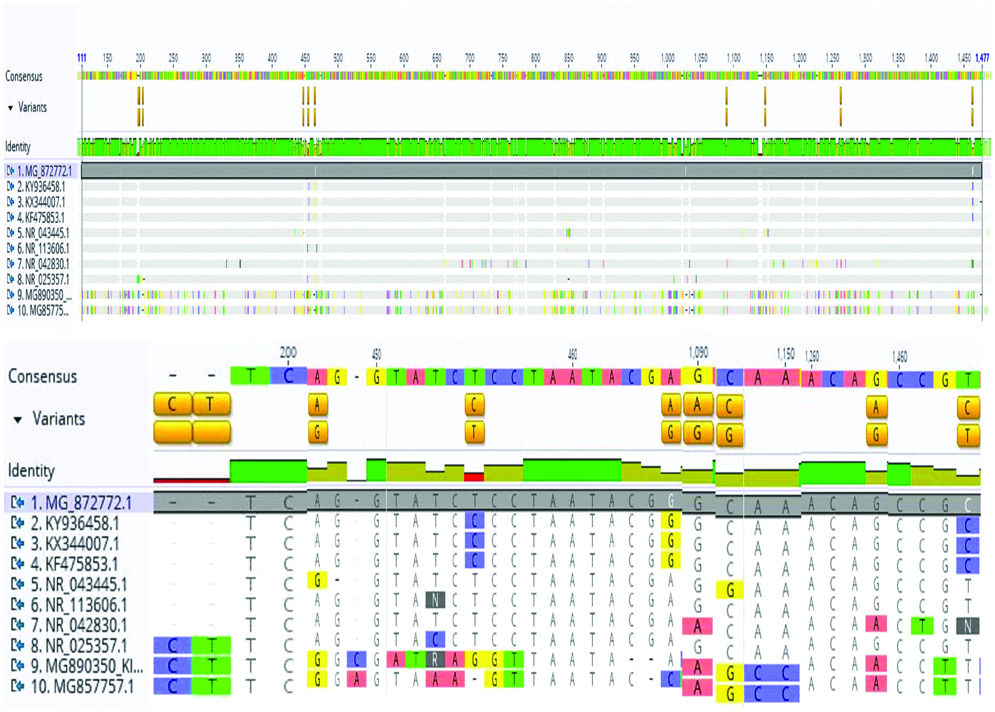
NCBI BLASTn found 99.7% sequence homology (both coverage and identity) of present study isolate with A. faecalis bacteria. Phylogenetic tree found close clustering of the study isolate with other A. faecalis strains previously found in soil and waste water [Table/Fig-1]. Evolutionary divergence data revealed that A. faecalis strain AF1 has negligible distance score (0.002) to four of the A. faecalis strains characterised from rhizosphere soil and polluted water. However, significant evolutionary divergence (0.179 and 0.186) exists among A. faecalis strain AF1 and two other outgroup bacteria Klebsiella pneumoniae and Escherichia coli [Table/Fig-2]. Genome-wide variants study in AF1 strain found nine SNPs, abundant in position 200 bp, 450 bp and after 1000 bp [Table/Fig-3]. The present study sequence can be found in GeneBank databank of NCBI under the accession number of MG872772.1.
Evolutionary relationships of A. faecalis with other Enterobacteriaceae bacterial group found in soil water and associated with UTI in Bangladesh. The evolutionary history was inferred using the Neighbour-Joining method. The percentage of replicate trees in which the associated taxa clustered together in the bootstrap test (1000 replicates) is shown next to the branches. The evolutionary distances were computed using the Kimura 2-parameter method and are in the units of the number of base substitutions per site. Evolutionary analyses were conducted in MEGA 7.0.
Estimates of evolutionary divergence among sequences. The number of base differences per site from between sequences is shown. The much similar sequences to the study strain AF1 are bolded in the table.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|
| 1 | - | | | | | | | | | |
| 2 | 0.002 | | | | | | | | | |
| 3 | 0.002 | 0.000 | | | | | | | | |
| 4 | 0.002 | 0.000 | 0.000 | | | | | | | |
| 5 | 0.007 | 0.006 | 0.006 | 0.006 | | | | | | |
| 6 | 0.002 | 0.002 | 0.002 | 0.002 | 0.005 | | | | | |
| 7 | 0.014 | 0.014 | 0.014 | 0.014 | 0.017 | 0.012 | | | | |
| 8 | 0.008 | 0.007 | 0.007 | 0.007 | 0.010 | 0.005 | 0.017 | | | |
| 9 | 0.186 | 0.185 | 0.185 | 0.185 | 0.187 | 0.185 | 0.193 | 0.186 | | |
| 10 | 0.179 | 0.178 | 0.178 | 0.178 | 0.180 | 0.178 | 0.186 | 0.179 | 0.024 | - |
Here number denotes for below species:
(1) MG_872772.1 A. Faecalis AF1; (2) KY936458.1 A. faecalis SDA3; (3) KX344007.1 Aacaligenes sp. G51; (4) KF475853.1 A. faecalis IHB6507; (5) NR043445.1 A. faecalis IAM12369; (6) NR113606.1 A. faecalis NRBC13111; (7) NR042830.1 A. faecalis sub. phenolicus J; (8) NR025357.1 A. faecalis sub. parafaecalis J; (9) MG890350 Klebsiellapneuminiae K20; and (10) MG857757.1 Escherichia coli E10.
SNPs heat-map of the study A. faecalis strain AF1 (MG872772.1) with other environmental strains found nine variants (highlighted in yellow) in different regions (first image), and a more close view of all the SNPs (second image). Genome-wide SNPs search was conducted in Genenious (v11.0.5) by taking the study strain as reference.
Discussion
The enormous increase in the percentages of UTI and the emergence of antibiotic-resistant isolates are two sparking problems in the health and medical sectors worldwide. Addressing UTI and RUTIs by common antibiotics are no longer effective in Bangladesh due to frequent and mal-administration of drugs. In addition, poor diagnostic technologies, region-based antibiotic activity and sometimes patient negligence make recovery process challenging and time-consuming [9]. Therefore, identification of precise bacterial species by proper diagnosis method and inspecting drug resistance pattern in selected regions are some of the prior pre-requisites before selecting the treatment strategies against UTI and RUTIs.
A. faecalis, an environmental bacterium although not frequently associated with diseases, may result in serious outcomes when causing chronic infections [23]. The present study strain was isolated from a urine sample of 35 years women patient suffering from UTI for the third time in her life. Initially, the patient was treated with antibiotics by assuming the bacteria as Escherichia coli. However, authors failed to characterise the bacteria by means of morphological and biochemical analysis for E. coli. After 16S rRNA sequencing and analysis, authors characterised the uncultured isolate as A. faecalis, for the first time from urine the sample, reported from Bangladesh. The strain AF1 had strong sequence homology, coverage, and negligible evolutionary distances, thus neighbouring close to other A. faecalis strains characterised from soil and water in India and Japan. Recently, A. faecalis associated UTI and cystitis infections have been reported in India where the majority of isolates were resistant to a large group of antibiotics [7,23]. Here, authors found a slightly higher percentage of drug resistance than the previous study in India [7]. This is probably due to incremental drug resistant graph in Bangladesh. E. coli alone gained 5%-7% more drug-resistance within the last five years [10].
The mystery behind the constant changing of habitat and colonisation of bacteria is yet to be explained properly. Previous research stated bacterial polymorphism as a common reason for changing microbial colonisation from one habitat to another [24]. Many SNPs in bacterial gene sequence lead to loss of common functions associated with bacterial virulence [25]. In this study, authors found nine SNPs in the 16S rRNA sequence of strain AF1 compared to other circulating A. faecalis bacteria found in India, Japan, South Korea, Mexico and Brazil. Those nine SNPs are probably responsible for sifting A. faecalis colonisation from environment to human. Therefore, opportunistic pathogen from the environment and hospital surfaces have emerged as major health threats in developing countries.
Limitation
The sample size was not sufficient enough in the study to conclude any significant remarks. Financial restraints and resources limitations restrict the study to be completed within a short time-frame. In addition, the study was completely regional, collected sample from a single hospital from the Eastern part of Bangladesh; therefore, it may not reflect the global scenario. In the future, long-term surveys required to analyse the multidrug-resistant A. faecalis bacterial isolates from UTI patients.
Conclusion
Environmental opportunistic pathogen like A. faecalis could be a potential source of UTI in Bangladesh. The incidence of mutations and high level of drug resistance in A. faecalis may predispose human to other types of chronic infections.
[1]. Vasudevan R, Urinary tract infection: An overview of the infection and the associated risk factorsJ Microbiol Exp 2014 1(2):01-15.10.15406/jmen.2014.01.00008 [Google Scholar] [CrossRef]
[2]. Behzadi P, Behzadi E, Yazdanbod H, Aghapour R, Cheshmeh A, Omran DS, A survey on urinary tract infections associated with the three most common uropathogenic bacteriaMaedica A J Clin Med 2010 5(67):111-15. [Google Scholar]
[3]. Malmartel A, Ghasarossian C, Bacterial resistance in urinary tract infections in patients with diabetes matched with patients without diabetesJ Diabetes Complications 2016 30(4):705-09.10.1016/j.jdiacomp.2016.01.00526851821 [Google Scholar] [CrossRef] [PubMed]
[4]. Tena D, Fern C, Lago MR, Alcaligenes faecalis: an unusual cause of skin and soft tissue infectionJapan J Infect Dis 2015 68(1):128-30.10.7883/yoken.JJID.2014.16425420652 [Google Scholar] [CrossRef] [PubMed]
[5]. Dubois V, Arpin C, Coulange L, Andre C, Noury P, Quentin C, TEM-21 extended-spectrum b-lactamase in a clinical isolate of Alcaligenes faecalis from a nursing homeJ Antimicrob Chemother 2005 57(2):368-69.10.1093/jac/dki45016344284 [Google Scholar] [CrossRef] [PubMed]
[6]. Mordi RM, Yusuf EO, Onemu SO, Igeleke CL, Odjadjare EE, The prevalence of Alcaligenes faecalis in bacteremia, meningitis and wound sepsis in a tertiary health care institutions in western part of NigeriaInt J Biotechnol 2013 2(7):123-29. [Google Scholar]
[7]. Khajuria A, Praharaj AK, Kumar M, Grover N, Emergence of VIM-6 metallo-beta-lactamase-producing Alcaligenes faecalis clinical isolates in a hospital in IndiaJ Infect Dev Ctries 2013 7(6):494-96.10.3855/jidc.355623771294 [Google Scholar] [CrossRef] [PubMed]
[8]. Raeisi J, Saifi M, Pourshafie MR, Habibi M, Mohajerani HR, Akbari N, Rapid identification of vancomycin resistant Enterococcus faecalis clinical isolates using a sugar fermentation methodJ Clin Diagnostic Res 2017 11(3):DC14-DC17.10.7860/JCDR/2017/19017.956828511382 [Google Scholar] [CrossRef] [PubMed]
[9]. Fuad MMH, Ferdowsy H, Hossain MN, Foysal MJ, Rahman MM, In-vitro antibacterial activity of common antibiotics and herb extracts to clinical isolates of Escherichia coli collected from UTI patientInt J Res Pharm Biomed Sci 2012 3(2):987-92. [Google Scholar]
[10]. Mahmudunnabi G, Majlish ANK, Momtaz F, Foysal MJ, Rahman MM, Islam K, Molecular detection and PCR-RFLP analysis using Pst1 and Alu1 of multidrug-resistant Klebsiella pneumoniae causing urinary tract infection in women in the eastern part of BangladeshJ Genet Eng Biotechnol 2018 16(1):77-82.10.1016/j.jgeb.2017.12.00430647708 [Google Scholar] [CrossRef] [PubMed]
[11]. Hooton TM, Recurrent urinary tract infection in womenInt J Antimicrob Agents 2001 17:259-68.10.1016/S0924-8579(00)00350-2 [Google Scholar] [CrossRef]
[12]. Pallett A, Hand K, Complicated urinary tract infections: practical solutions for the treatment of multiresistant Gram-negative bacteriaJ Antimicrob Chemother 2010 65:25-33.10.1093/jac/dkq29820876625 [Google Scholar] [CrossRef] [PubMed]
[13]. Nickel JC, Urinary tract infections and resistant bacteriaRev Urol 2007 9(2):78-80. [Google Scholar]
[14]. Badr AA, Shaikh G, Recurrent urinary tract infections management in womenSultan Qaboos Univ Med J 2013 13(8):359-67.10.12816/000325623984019 [Google Scholar] [CrossRef] [PubMed]
[15]. Nikaido H, Multidrug resistance in bacteriaAnnu Rev Biochem 2010 78(2):119-46.10.1146/annurev.biochem.78.082907.14592319231985 [Google Scholar] [CrossRef] [PubMed]
[16]. Rabbee M, Begum M, Islam M, Chowdhury P, Chowdhury O, Zohora F, Multidrug resistance phenotype and plasmid profiling of Escherichia coli isolates causing urinary tract infections in north east part of BangladeshBr Microbiol Res J 2016 15(6):01-11.10.9734/BMRJ/2016/27393 [Google Scholar] [CrossRef]
[17]. Fair RJ, Tor Y, Antibiotics and bacterial resistance in the 21st centuryPerspect Medicin Chem 2014 6:25-64.10.4137/PMC.S1445925232278 [Google Scholar] [CrossRef] [PubMed]
[18]. Srinivasan R, Karaoz U, Volegova M, MacKichan J, Kato-Maeda M, Miller S, Use of 16S rRNA gene for identification of a broad range of clinically relevant bacterial pathogensPLoS One 2015 10(2):1-22.10.1371/journal.pone.011761725658760 [Google Scholar] [CrossRef] [PubMed]
[19]. Koboldt DC, Steinberg KM, Larson DE, Wilson RK, Mardis E, The next-generation sequencing revolution and its impact on genomicsCell 2014 155:27-38.10.1016/j.cell.2013.09.00624074859 [Google Scholar] [CrossRef] [PubMed]
[20]. Sedlar K, Kupkova K, Provaznik I, Bioinformatics strategies for taxonomy independent binning and visualization of sequences in shotgun metagenomicsCoputational Struct Biotechnol J 2017 15:48-55.10.1016/j.csbj.2016.11.00527980708 [Google Scholar] [CrossRef] [PubMed]
[21]. Balouiri M, Sadiki M, Ibnsouda SK, Methods for in vitro evaluating antimicrobial activity: A reviewJ Pharm Anal 2016 6(2):71-79.10.1016/j.jpha.2015.11.00529403965 [Google Scholar] [CrossRef] [PubMed]
[22]. Miyashita A, Mochimaru H, Kazama H, Ohashi A, Yamaguchi T, Nunoura T, Development of 16S rRNA gene-targeted primers for detection of archaeal anaerobic methanotrophs (ANMEs)FEMS Microbiol Lett 2009 297(1):31-37.10.1111/j.1574-6968.2009.01648.x19486160 [Google Scholar] [CrossRef] [PubMed]
[23]. Ertem GT, Sari T, Hatipoglu CA, Yildiz E, Zarakolu P, Oral B, First reported case of Alcaligenes faecalis peritonitisPerit Dial Int 2010 30:112-21.10.3747/pdi.2008.0027420056995 [Google Scholar] [CrossRef] [PubMed]
[24]. Blaser MJ, Musser JM, Blaser MJ, Musser JM, Bacterial polymorphisms and disease in humansJ Clin Invest 2001 107:391-92.10.1172/JCI1199311181636 [Google Scholar] [CrossRef] [PubMed]
[25]. Bryant J, Chewapreecha C, Bentley SD, Developing insights into the mechanisms of evolution of bacterial pathogens from whole-genome sequencesFuture Microbiol 2014 7(11):1283-96.10.2217/fmb.12.10823075447 [Google Scholar] [CrossRef] [PubMed]