Ureteric Avulsion Following Blind Attempts at Retrieval of Intrauterine Contraceptive Device: A Clinical Lesson to Primary Care Givers
Divya Shrimal1, Akhila Vasudeva2, Shripad Hebbar3, Arun Chawla4
1 Junior Resident, Department of Obstetrics and Gynaecology, KMC, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Professor and Head of Unit, Department of Obstetrics and Gynaecology, KMC, Manipal Academy of Higher Education, Manipal, Karnataka, India.
3 Professor and Head of Unit, Department of Obstetrics and Gynaecology, KMC, Manipal Academy of Higher Education, Manipal, Karnataka, India.
4 Professor and Head, Department of Urology, KMC, Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Akhila Vasudeva, Professor and Head of Unit, Department of Obstetrics and Gynaecology, KMC, Manipal Academy of Higher Education, Manipal, Udupi, Karnataka, India.
E-mail: akhilavasudeva@gmail.com
Intra Uterine Contraceptive Device (IUCD) is the most popular method of reversible contraception in India because of their high efficacy for fertility regulation, low-risk, low-cost, and lack of required maintenance. Uterine perforation remains one of the most serious complications, with an incidence 0.87 per 1000 insertions. The IUCD strings are used to monitor and remove the device. Missing IUCD strings are observed in about 5% of the users. Such patients require localisation of the device using Transvaginal Scan (TVS) and X-Ray, and combined hysterolaparoscopic approach for its retrieval. Hereby we report a case of young primipara, who consulted a local practitioner requesting IUCD removal, as she was planning to conceive her second child. On examination, Cu-T threads were not found. A plain X-Ray of the pelvis was reported as: Cu-T limbs seen in the left side of the pelvis, “in the region of uterus”. Blind attempts led to damage to ovary and uterus along with the ureter. By reporting this case, we hope to raise awareness on the management of misplaced IUCD, among primary care givers; and the need for set protocols on the management of such cases.
IUCD, Retrieval, Missing, Ureter injury, Uterine perforation
Case Report
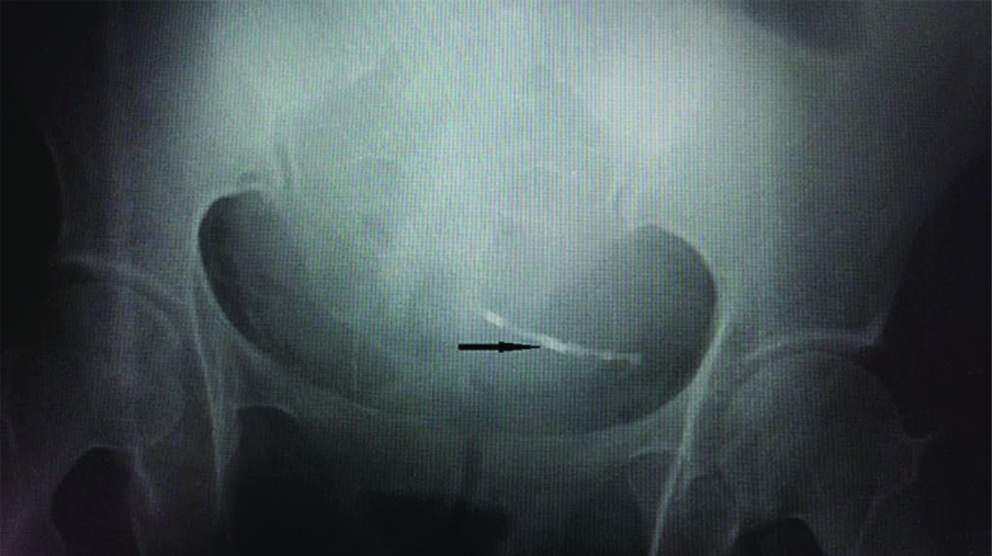
A 27-year-old female, primipara, presented with complaints of abdominal distension and pain, increased in intensity since five days, associated with vomiting. Lady had Intrauterine Copper Device (IUCD) inserted during her lactational amenorrhea, four months after her caesarean section. There were no symptoms suggestive of perforation at that time such as pain, abnormal uterine bleeding etc. Five years later, she went to a primary health care set up for its removal, as she was planning her second conception. On examination, Cu-T (copper-T) threads were missing. A plain X-Ray of the pelvis showed Cu-T limbs on the left side of the pelvis, “in the region of uterus” [Table/Fig-1]. Under spinal anaesthesia, attempts were made to locate and remove the IUCD, which were unsuccessful. She developed some abdominal distension, pain abdomen, and on and off vomiting for a few days following this procedure for which she was treated with analgesics, antacids, antiemetics and laxatives. She improved symptomatically and was discharged on 10th postoperative day. She was readmitted after 3-4 days, was treated symptomatically for “gastritis’ and discharged. After a week, she developed severe backache and her symptoms worsened, hence she was referred to our tertiary care centre for further management. On arrival, general examination revealed significant tachycardia of 120 beats/minute. Abdomen was grossly distended with free fluid in the abdomen, but non tender. On speculum examination, Cu-T threads were not visible. There was mild tenderness while performing bimanual examination. Routine preoperative investigations, including renal function were normal. Abdominal Ultrasound revealed a huge amount of turbid free fluid. Cu-T was seen displaced and embedded to the region of the caesarean scar on the left side of the uterus. Paracentesis was done which revealed blood stained fluid in the abdominal cavity.
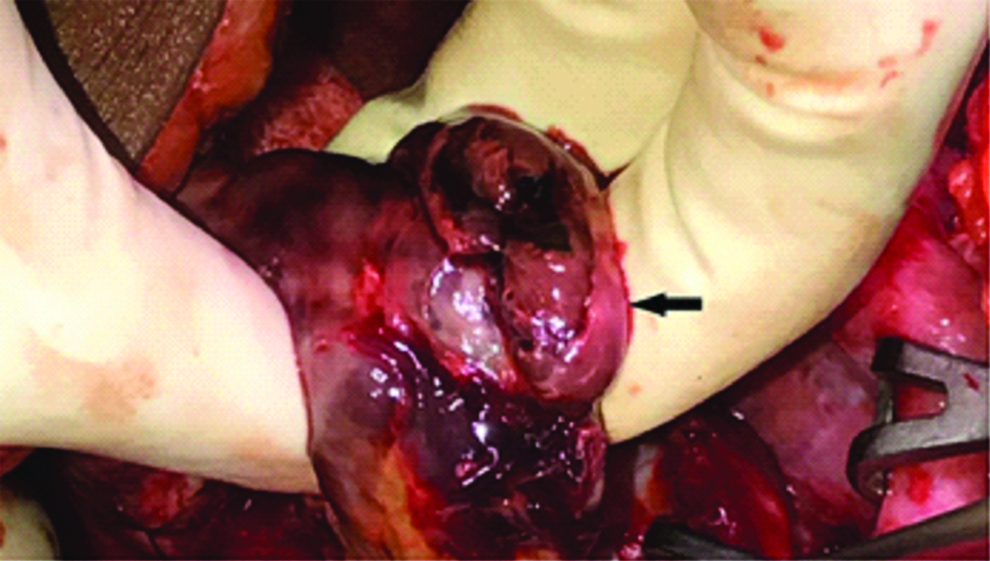
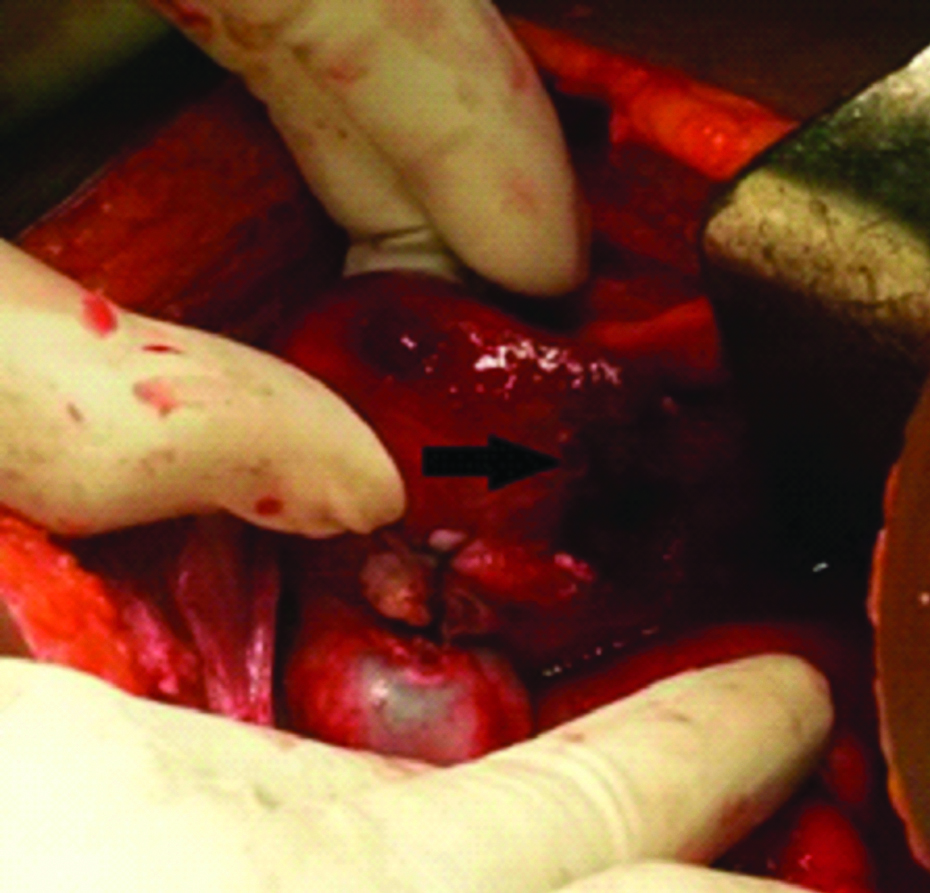
Emergency laparotomy was performed after starting broad spectrum antibiotics. Four litres of thin blood stained fluid was drained from the peritoneal cavity. On biochemical analysis of the fluid, creatinine level of 4 mg/dL was noted, which was suggestive of urinary ascites. Cu-T was found near isthmus on the left side of the uterine scar. It was lying on the posterior fold of broad ligament, probably after complete perforation through the uterine scar area as a result of blind manipulations. Right ovary was found completely necrotic and gangrenous [Table/Fig-2], avulsed from all its attachments, lying loosely on the posterior surface of the uterus. It was removed and sent for histopathology where it was reported as infarcted right ovary. Large irregular rent was found on the right lateral wall/posterior surface of uterus near right uterine artery [Table/Fig-3], which was sutured.
A plain X Ray of pelvis: Arrow pointing to Cu-T limbs seen in the left side of pelvis, “in the region of uterus”.
Arrow showing gangrenous right ovary, found avulsed from all its attachments, lying loosely on the posterior surface of uterus.
Arrow pointing towards large irregular rent found on the right lateral wall/posterior surface of uterus near right uterine artery.
Throughout the surgery, it was observed that peritoneal cavity was slowly getting pooled by clear fluid trickling down the right paracolic gutter into the pelvis. Therefore, ureters were traced and mobilised from the bifurcation of common iliac artery downwards. Left ureter was normal. On the right side, six centimetres of distal ureter was found to be gangrenous [Table/Fig-4] with urine leaking from the proximal end. Because of inflammatory reaction, ureter was densely adhere to the retroperitoneum.
Arrow pointing to gangrenous distal ureter, which was later excised.
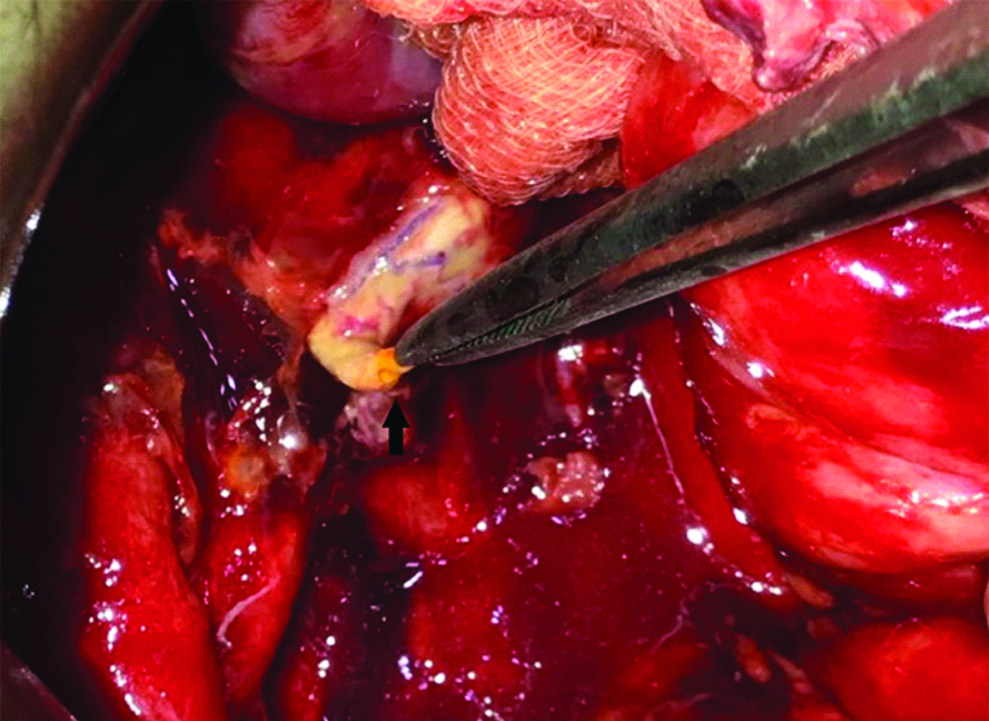
Urologists were called for help. Gangrenous end of ureter was excised. The proximal end of ureter was mobilised for two inches. Boari flap was taken from the bladder and anastomosed to the spatulated ureteric end over a 6 Fr ureteric D-J Stent [Table/Fig-5]. She received two units each of packed RBCs and Fresh Frozen Plasma. Two pelvic drains were placed.
Picture Uretero vesical anastomosis with Boari’s flap. A: Urinary bladder; B: Boari’s flap; C: Proximal ureter

Her postoperative recovery was smooth. Urinary catheter was removed after 14 days. D-J stent was removed after six weeks. She was asked to follow up after three months. Currently she is doing fine.
Discussion
IUCD is a widely used method for contraception. About one out of five women in reproductive age all over the world use IUCD while in India, it corresponds to about three in 100 women, copper devices being the most popular [1]. It remains the most commonly used method of reversible contraception in India because of its high efficacy for fertility regulation, low-risk, low-cost, and lack of required maintenance [2]. Its usage has proven beneficial despite the short term adverse effects such as menorrhagia, dysmenorrhoea etc. However, serious complications may arise, either due to IUCD itself or due to inappropriate management of the complications.
Silent perforation of IUCD is known to cause visceral injury. Several such complications have been reported including ureteric stricture/injury, hydronephrosis, bladder perforation, bladder stone formation, intestinal obstruction/stricture, urinary and bowel fistulas [3-6]. Ureteric strictures have occurred due to pelvic inflammatory disease resulting from long forgotten IUD [7].
In a retrospective analysis of 18 patients with misplaced IUCDs [8], inadequate pelvic examination and inexperience of the operator were important risk factors for uterine perforation at the time of insertion. In addition, a small sized uterus as seen in lactating women/nulliparous women and the caesarean scar may also predispose to uterine perforation.
Another retrospective analysis, which included 75 patients with missing intrauterine device who required surgical intervention [9] stated that the diagnosis of IUD/IUS perforation was usually straightforward after suspicion of a misplaced device. A combination of vaginal US and abdominal X-ray is usually sufficient to diagnose a perforation. A combined hysterolaparoscopic approach is always ideal to retrieve IUCD whenever there is a suspicion of perforation [10,11].
However, in this case, uterine perforation is unlikely to have occurred at the time of insertion as she was completely asymptomatic and there was no history suggestive of pregnancy as a result of Cu-T failure. There is a possibility of silent perforation of caesarean scar leading to IUCD migration near the left broad ligament. We presume that uterine perforation was a result of inappropriate manipulation done for Cu-T removal. Blind attempts at its retrieval have resulted in uterine perforation, avulsion of the ovary and loss of a segment of ureter and its infarction and urinary ascites. To the best of our knowledge, this is the first case of such a ureteric damage and its unusual extent, resulting from an attempt at IUCD retrieval.
Ureteric injuries can be managed using different approaches depending upon the length of ureteric segment involved. Various available options are ureteric reimplantation, psoas hitch, Boari flap, ileal replacement of ureter. The importance of ensuring good vascular supply, complete excision of pathological lesions, good drainage and a wide spatulated and tension-free anastomosis of mucosa to mucosa remain paramount [12]. In this case, after excising the gangrenous distal ureter, about 10 cm of the ureteric segment was lost which could be bridged using Boari flap. Ureteric reconstruction in fresh injuries is a comfortable exercise. However, delayed presentation/detection contaminates the retroperitoneum and peritoneal planes making ureteric reconstruction a difficult and challenging exercise.
Conclusion
In a case of misplaced IUCD; an ultrasound examination and a pelvic X-Ray must be interpreted carefully so as to know its location. Whenever, there is suspicion of uterine perforation, a combined hystero laparoscopic approach is always ideal to safely retrieve the IUCD and inspect for visceral injury. Blind attempts at its retrieval should never be performed at the primary care. This case highlights the need for appropriate training and protocol based management of misplaced IUCD. This is important, as one such case may discourage many women from using IUCD, which remains one of the most efficient, affordable and safe methods of contraception in developing countries.
[1]. IUD guidelines for family planning service programme by JH Piego USAID. 2006 [Google Scholar]
[2]. Aggarwal S, Jindal RP, Deep A, Intravesical migration of intrauterine contraceptive devices with stone formationJ Family Med Prim Care 2014 3(4):449-51.10.4103/2249-4863.14814725657964 [Google Scholar] [CrossRef] [PubMed]
[3]. Priyadarshi V, Sehgal N, Sen D, Ureteric erosion and obstruction: A rare but dreaded complication of intrauterine contraceptive deviceUrol Ann 2017 9(1):103-06.10.4103/0974-7796.19883928216944 [Google Scholar] [CrossRef] [PubMed]
[4]. Tosun M, Celik H, Yavuz E, Cetinkaya MB, Intravesical migration of an intrauterine device detected in a pregnant womanCan Urol Assoc 2010 4(5):E141-E143.10.5489/cuaj.93820944794 [Google Scholar] [CrossRef] [PubMed]
[5]. Ozcelik B, Serin IS, Basbug M, Aygen E, Ekmekcioglu O, Differential diagnosis of intra-uterine device migrating to bladder using radiographic image of calculus formation and review of literatureEur J Obstet Gynecol Reprod Biol 2003 108(1):94-96.10.1016/S0301-2115(02)00240-3 [Google Scholar] [CrossRef]
[6]. Yang X, Duan X, Tao W, Ureteric obstruction caused by a migrated intrauterine deviceUrol Case Rep 2017 10:33-35.10.1016/j.eucr.2016.11.01127920988 [Google Scholar] [CrossRef] [PubMed]
[7]. Yonemura S, Moriya M, Hori Y, Arima K, Toyoda N, Sugimura Y, Ureteral obstruction associated with pelvic inflammatory disease in a long-term intrauterine contraceptive device userInt J Urol 2006 13(3):315-17.10.1111/j.1442-2042.2006.01280.x16643637 [Google Scholar] [CrossRef] [PubMed]
[8]. Balci O, Mahmoud AS, Capar M, Colakoglu MC, Diagnosis and management of intra-abdominal, mislocated intrauterine devicesArch Gynecol Obstet 2010 281(6):1019-22.10.1007/s00404-010-1374-820157719 [Google Scholar] [CrossRef] [PubMed]
[9]. Kaislasuo J, Suhonen S, Gissler M, Lähteenmäki P, Heikinheimo O, Uterine perforation caused by intrauterine devices: clinical course and treatmentHuman Reprod 2013 28(6):1546-51.10.1093/humrep/det07423526304 [Google Scholar] [CrossRef] [PubMed]
[10]. Behtash N, Akhavan S, Mokhtar S, Pelvic mass due to transmigrated IUDActa Med Iran 2010 48(2):125-26. [Google Scholar]
[11]. Aydogdu O, Pulat H, Asymptomatic far-migration of an intrauterine device into the abdominal cavity: A rare entityCan Urol Assoc J 2012 6:E134-36.10.5489/cuaj.1110022709887 [Google Scholar] [CrossRef] [PubMed]
[12]. Png JC, Chapple CR, Principles of ureteric reconstructionCurrent Opinion in Urology 2000 10(3):207-12.10.1097/00042307-200005000-0000410858898 [Google Scholar] [CrossRef] [PubMed]