Prevention of Severe Tongue Biting in a Mentally Challenged Patient: A Clinical Report
Filiz Aydoğan1, Aynur Medine Şahin Sağlam2
1 Faculty of Dentistry, Department of Orthodontics, University of Suleyman Demirel, Isparta, Turkey.
2 Faculty of Dentistry, Department of Orthodontics, University of Suleyman Demirel, Isparta, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Filiz Aydoğan, Department of Orthodontics, Faculty of Dentistry, University of Suleyman Demirel, Isparta, Turkey.
E-mail: filizydgn03@mail.com
Orofacial dysfunctions and habits are the main factors which influence the development of malocclusion and perioral disease. In this context, Orthodontics, a field of Dentistry, is closely associated with the diagnosis and treatment of injuries stemming from oral habits and parafunctions. This rare case report presents the treatment of a mentally challenged 23-year-old male patient who had a tongue biting habit for four years. Underlying causes of tongue biting must be investigated and the most appropriate treatment should be performed.
Habit breaking appliance, Parafunctions, Malocclussion, Removable appliance, Self injurious behaviour
Case Report
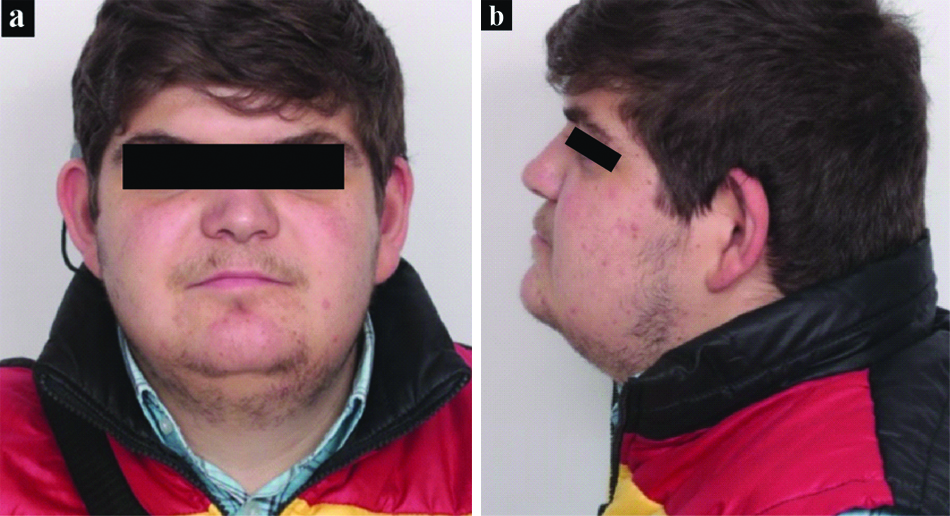
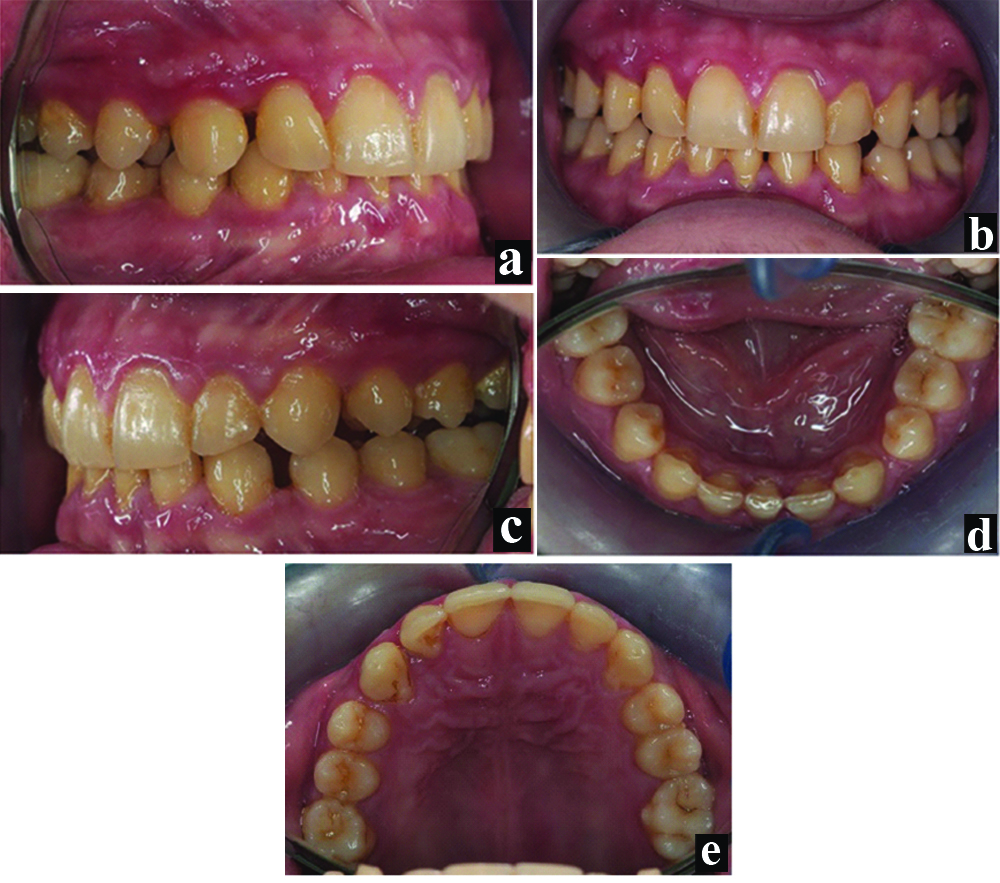
A 23-year-old white male patient presented with a four-year history of tongue biting. The patient stated that he did not know when and how often he bites his tongue. The patient’s main complaints were pain, swelling and continuous large ulceration on the right posterior side of the tongue [Table/Fig-1]. The patient and his mother revealed that the traumatic ulceration appeared suddenly and progressively worsened, which affected the feeling. Due to these complaints, he had received Orthodontic treatment with fixed appliance without tooth extraction at another Orthodontic clinic. This treatment ended five months ago. However, as the problem did not come to a solution at the end of the treatment, the patient visited the Department of Orthodontics, University of Suleyman Demirel. The patient’s medical reports indicated mental retardation (IQ:72-75 borderline intellectual functioning). Furthermore, the patient had been wearing a hearing aid because of his sensorineural hearing loss (52%). Extraoral examination revealed a symmetrical face with a concave profile [Table/Fig-2a,b]. Intraoral examination showed Class III subdivision malocclusion with one congenitally missing mandibular incisor [Table/Fig-3a-e]. There were mildly increased overbite and overjet as well as diastemas in the lower and upper arches [Table/Fig-3a-e]. On intraoral examination, a swollen, painful ulcerative lesion of approximately 1 cm×2 cm in size was seen on the right lateral surface of the tongue [Table/Fig-1]. Mental retardation-related low tongue-movement control was considered the reason behind his tongue-biting habit. However, tongue biting is associated with many neurological and psychiatric disorders, so the patient was redirected to the relevant departments. Unfortunately, the patient’s family have denied our consultation, saying that his son has no complaints other than the stated.
Pretreatment photograph of the tongue.

Extra oral photographs of the patient.
Intra oral photographs of the patient.
The swelling caused by repeated biting makes it easier to traumatise the same area again. Thus, the patients’ treatment plan was to protect the tongue from being bitten. A modified Hawley appliance was designed to prevent the right lateral region of the tongue from entering between the teeth. Maxillary and mandibular alginate impressions for the patient were taken. The impressions were disinfected (DETROXDetrosept AF, Medical Device Disinfectant, DetroksChem and Health Products Co., Ltd. İstanbul, Turkey) and poured with Type IV dental stone. An interocclusal record was taken with pink baseplate wax. We did not take a new x-ray because the patient stated that he had an x-ray at the end of the first orthodontic treatment (As Low As Reasonably Achievable).
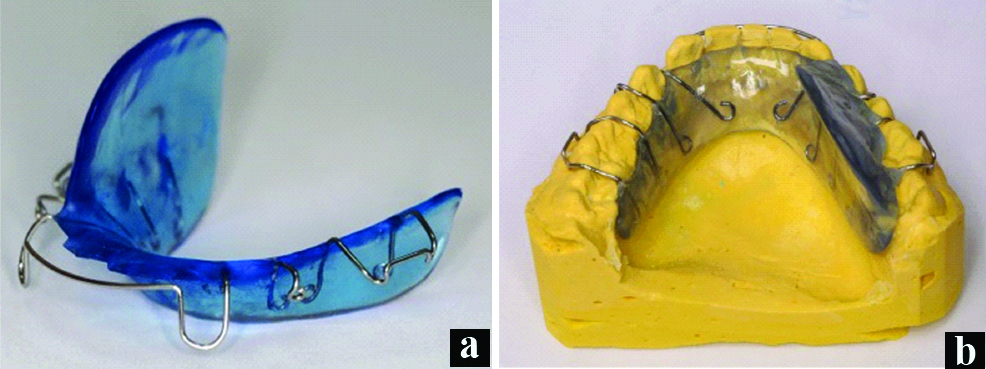
The modified mandibular Hawley appliance was designed to help eliminate tongue biting. The appliance’s right side was extended from the mandibular lingual sulcus to the maxillary gingival margin of the teeth to prevent the tongue from entering between the teeth [Table/Fig-4a,b]. A round stainless steel wire (0.7 mm diameter) was used to prepare two Adam’s clasps on the molars, two ball clasps between the first and second premolars and a labial bow from canine to canine for clasp construction of the appliance. While constructing the appliance, the undercut areas were blocked with wax to allow easy removal and placement of the appliance. The acrylic base of the appliance was made on the dental cast model with the layering technique, using cold-cured acrylic powder and monomer liquid. After polymerisation, the appliance was trimmed with burs and polished with pumice. The prepared appliance was disinfected and rinsed before it was tried in the patient’s mouth.
View of the modified mandibular Hawley appliances with/without patient cast.
The appliance was fitted by tightening the clasps in the patient’s mouth and the acrylic was seated on the soft tissues without any irritation [Table/Fig-5]. It was recommended for use throughout the day and did not need to be taken off while eating and sleeping. The patient was advise to clean his appliance twice a day with a soft brush and hand soap or mild dish washing liquid. The ulceration rapidly healed and completely recovered after three weeks, thanks to the patient’s compliance [Table/Fig-6]. The patient and his mother were called two months later, but they did not want to come to the control appointment because of the healing of the patient’s tongue.
Intraoral photographs of a modified mandibular Hawley appliance with a patient-centric relation.

Post-treatment photographs of the patient’s tongue.

Discussion
The tongue is a muscular organ in the mouth that is instrumental in several functions, such as taste recognition, speech, swallowing and mastication. These functions considerably affect quality of life. In rare conditions, the tongue may be traumatised by abnormal teeth biting, which causes discomfort to the patient. Tongue biting is usually associated with occlusal, neurological or psychiatric diseases; therefore, the treatment should be applied based on its aetiology. Some authors have described tongue biting as an important and definitive clinical finding of epilepsy [1]. Tongue biting has also been associated with fainting, psychogenic seizures, nocturnal tongue biting and pathological diseases [2-5].
Tongue biting, when severe enough to cause extensive ulceration in a person with a mental retardation, is distressing for both the patient and his or her parents. In mentally challenged patients, self-destructive behaviour such as hand, tongue and cheek biting may be observed [6-8]. Self-destructive behaviours may or may not be epileptic. EEG and video EEG monitoring are widely used to diagnose the aforementioned diseases [9,10]. Although the underlying cause of tongue biting in our patient could not be identified because his mother did not consent to our tests, it can be treated with local precautions. However, the problem may recur if the cause is not associated with occlusion.
In the literature review, we searched for research published in English in May/2018 or earlier on Google Scholar, PubMed, ProQuest, SCOPUS, EBSCOhost, and EMBASE using various terms, such as tongue bite, tongue biting, tongue chewing, tongue biting habit, tongue chewing habit, tongue biting epilepsy, tongue biting seizure, tongue biting removable appliance and treatment of tongue bite. Consequently, we found several cases which had reported the use of ‘tongue biting prevention device’ (for a patient having undergone a partial glossectomy) [5], ‘thermoplastic split’ (for infants) [11] and ‘tongue stent’ (for a comatose patient) [12] to treat tongue biting. The treatment type can be modified according to the patient’s mental status, the patient’s age and the site of the bite and occlusion. Metal plates or flanges could be soldered to molar bands as an alternative treatment option.
The mechanism of action of removable appliances is to remove the cause similar to that of our modified Hawley appliance [5,11,12]. In other words, the tongue could be retained in its normal space within the oral cavity and kept from coming into contact with the teeth due to removable appliances. The long-term use of removable appliances typically should be avoided, as it may affect oral hygiene, chewing, talking and swallowing. Although the continuous use of these preventive appliances is not necessarily recommended, in some rare cases, clinicians should recommend continuous use of the appliance because of the high chance of the recurrence of dental pathologies without it.
Conclusion
Tongue bites can be a severe concern and may cause extensive ulceration in patients; this is an unsettling condition for both the patients and their relatives. Notably, tongue biting is often seen in patients with psychiatric and neurological problems. The tongue biting habit is widely considered helpful in diagnosing certain neurological diseases. Furthermore, the appliance in this paper could be usefully applied to other situations such as accidental damage and other oral auto-destructive behaviours. The underlying causes of tongue bites should be diagnosed and treated appropriately. Multidisciplinary treatments from the perspectives of neurology, psychiatry and dentistry have proved success until now.
[1]. Bendadid SR, Tongue biting as a lateralizing sign in partial epilepsySeizure-European Journal of Epileps 1996 5(3):175-76.10.1016/S1059-1311(96)80032-X [Google Scholar] [CrossRef]
[2]. Brigo F, Nardone R, Bongiovanni LG, Value of tongue biting in the differential diagnosis between epileptic seizures and syncopeSeizure-European Journal of Epilepsy 2012 21(8):568-72.10.1016/j.seizure.2012.06.00522770819 [Google Scholar] [CrossRef] [PubMed]
[3]. Brigo F, Storti M, Lochner P, Tezzon F, Fiaschi A, Bongiovanni LG, Tongue biting in epileptic seizures and psychogenic events: an evidence-based perspectiveEpilepsy & Behaviour 2012 25(2):251-55.10.1016/j.yebeh.2012.06.02023041172 [Google Scholar] [CrossRef] [PubMed]
[4]. Seneviratne U, Facio-mandibular myoclonus: a rare cause of nocturnal tongue bitingEpileptic Disorders 2011 13(1):96-98.10.1684/epd.2011.041421393099 [Google Scholar] [CrossRef] [PubMed]
[5]. Pigno MA, Funk JJ, Prevention of tongue biting with a removable oral device: a clinical reportJ Prosthet Dent 2000 83(5):508-10.10.1016/S0022-3913(00)70005-9 [Google Scholar] [CrossRef]
[6]. Willette JC, Lip-chewing: another treatment optionSpecial Care in Dentistry 1992 12(4):174-76.10.1111/j.1754-4505.1992.tb00440.x1440138 [Google Scholar] [CrossRef] [PubMed]
[7]. Symons FJ, Thompson T, Self-injurious behaviour and body site preferenceJournal of Intellectual Disability Research 1997 41(6):456-68.10.1111/j.1365-2788.1997.tb00737.x9430049 [Google Scholar] [CrossRef] [PubMed]
[8]. Mehta V, Oral self-injury: report of a casewithreview of literatureDent Open Journal 2015 2(3):77-79.10.17140/DOJ-2-115 [Google Scholar] [CrossRef]
[9]. Arslan D, Outcome of Long-Term Video-EEG MonitoringJournal of the Turkish Chapter of ILAE 2017 23(3):118-22.10.14744/epilepsi.2017.18189 [Google Scholar] [CrossRef]
[10]. Erlichman M, Electroencephalographic (EEG) video monitoringHealth Technology Assessment Reports 1990 4:01-14. [Google Scholar]
[11]. Suchak A, Mars M, A unique presentation of severe tongue biting in 10 month-old twins with a novel approach to managementEuropean Archives of Paediatric Dentistry 2010 11(3):149-54.10.1007/BF0326273220507814 [Google Scholar] [CrossRef] [PubMed]
[12]. Hanson GE, Ogle RG, Giron L, A tongue stent for prevention of oral trauma in the comatose patientCritical Care Medicine 1975 3(5):200-03.10.1097/00003246-197509000-00007765061 [Google Scholar] [CrossRef] [PubMed]