A 24-year-old primigravid woman at 28 weeks of gestation was admitted to the hospital because of drug-refractory atrial tachycardia and heart failure. The arrhythmia did not respond to drug therapy and electrical cardioversion. Since tachycardia was intractable and had potentially life-threatening consequences for mother and foetus, it was decided to ablate the tachycardia after a multidisciplinary meeting. During the procedure, maternal hypotension occurred, consequently causing persistent foetal heart rate reduction. Radiofrequency ablation was immediately cancelled and emergency caesarean section was carried out. After 72 hours after the caesarean-section, successful RF ablation could be performed. Mother was discharged on the seventh postoperative day. The newborn was hospitalised until having reached 2500 g and he was discharged in good condition. Mother’s left ventricle systolic function significantly improved and no atrial tachyarrhythmia was observed on the sixth month follow-up visit.
Atrial tachyarrhythmia, Pregnancy, Radiofrequency ablation
Case Report
A 24-year-old primigravid woman at 28 weeks of gestation had palpitations and dyspnea which limited her physical activity for the last week. Her functional status was Class III-IV according to the NYHA scale. She was referred to our arrhythmia clinic for incessant supraventricular tachycardia for further investigation and treatment.
On the day of the admission her blood pressure was 90/60 mmHg and heart rate was between 160 and 180 beats per minute. A 3/6 pan systolic murmur at the apical area was noted and fine crepitations were present in the lung basal areas. Other than having had frequent tonsillitis attack throughout the childhood, her past medical history was uneventful. Abdominal examination was consistent with a 28-week pregnancy. The remaining examination was unremarkable.
Her initial 12-lead electrocardiogram showed a narrow QRS complex, tachycardia (SVT) at 160 beats per minute with P waves that were negative in the inferior limb leads, biphasic in V1 and positive in a VL [Table/Fig-1a]. She had mild anaemia (haemoglobin was 11.2 g/dL), leukocytosis (13.400/mm3) and normal range of platelet (311.000/mm3). Thyroid, kidney and liver function tests were all within the normal ranges. INR was 0.97 and her NTproBNP result was 2248 pg/mL. Obstetric assessment revealed a viable single fetus with Actual Ultrasound Age (AUA) 28 weeks. Non Stress Test (NST) results were reactive. Preeclampsia was ruled out.
a) The electrocardiography demonstrated the atrial tachycardia; b) Transthoracic echocardiographic examination showed decreased left ventricular systolic function and severe eccentric mitral valve insufficiency.
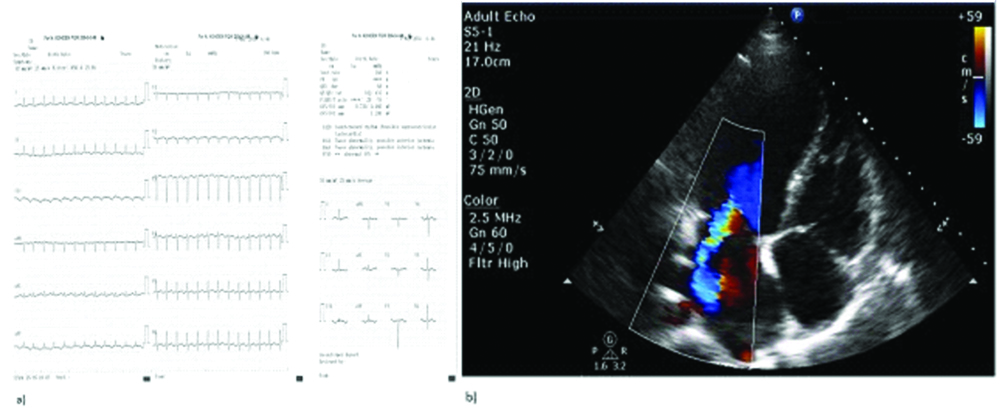
Transthoracic Echocardiographic Examination (TTE) showed decreased left ventricular systolic function (ejection fraction was 38%), global hypokinesia of left ventricle, dilatation of left atrium (4.5 cm), severe eccentric mitral valve insufficiency and mild tricuspid valve insufficiency. Mitral valve’s thickness was increased and estimated systolic pulmonary artery pressure was 34 mmHg on TTE examination [Table/Fig-1b].
The arrhythmia did not respond to intravenous adenosine, metoprolol and digoxin therapy and tachycardia continued with a 1:1 AV conduction. She was given intravenous amiodarone for this potentially life-threatening tachyarrhythmia. Although tachycardia rate decreased slightly, her haemodynamic condition got worse and amiodarone was stopped. Electric cardioversion was performed but failed so; she was referred for catheter ablation.
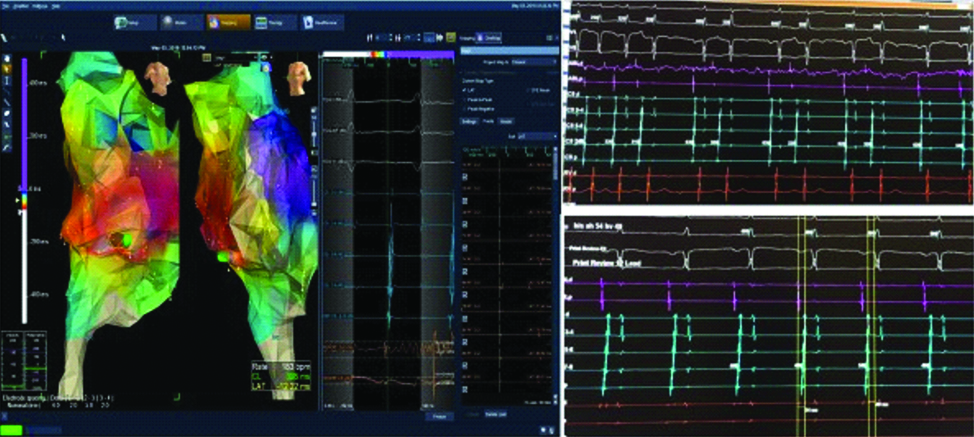
After written informed consent was obtained, the patient underwent procedure under general anaesthesia in a fasting state. The obstetrics team was ready and foetal cardiac monitorization was carried out throughout the procedure. By correct shielding, low frame rates and short fluoroscopy times, ionising radiation exposure was minimised. Three venous access was obtained on both femoral veins. One decapolar and one quadripolar catheter were advanced into the coronary sinus and His bundle. Mapping and RF ablation was performed with a 4-mm tip deflectable quadripolar ablation catheter (Medtronic Marinr TM 7 Fr. Diagnosis of focal atrial tachycardia was made according to standard electrophysiological criteria [1]. The earliest atrial activation during tachycardia was located in the low crista teminalis region. During RF ablation in this region, maternal hypotension occurred, consequently followed by foetal heart rate reduction. Foetal heart rate reduction was not resolved after augmentation of the maternal blood pressure and emergent cesarean delivery was carried out. The baby’s birth weight was 1260 grams and the APGAR scores at one and five minutes were two and four, respectively. He was transferred to the neonatal intensive care unit. At 72 hours after the caesarean section, a successful RF ablation could be performed with 3D mapping (Ensite Navx) systems. One reference catheter was placed in the coronary sinus and another catheter was placed in the right ventricle apex in case of a need to stimulate the ventricle. Right atrial anatomy was drawn with the RF ablation catheter. After localising the earliest site of activation (low crista terminalis region) during tachycardia, two RF applications were delivered. A normal sinus rhythm was achieved right after the successful atrial tachycardia ablation [Table/Fig-2].
Electrophysiological (EP) study images.
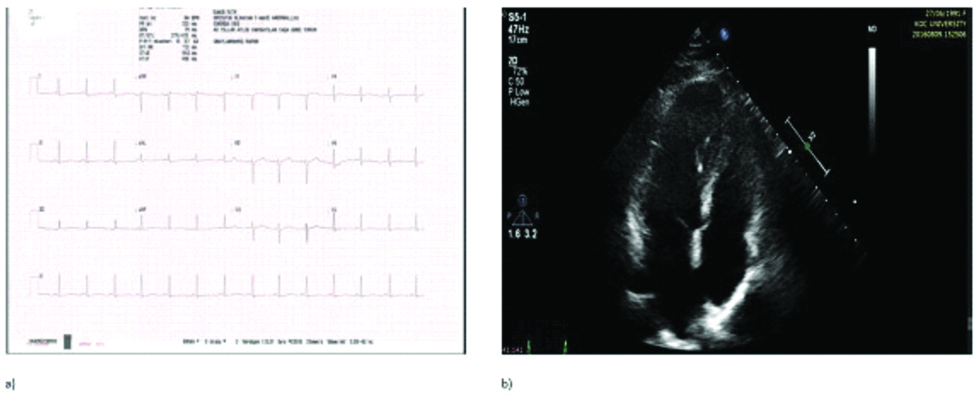
On follow-up the symptoms gradually decreased. Medical treatment was adjusted and the patient was discharged on the seventh postoperative day. The newborn was hospitalised until having reached 2500 grams. The left ventricle systolic function of mother significantly improved and no atrial tachyarrhythmia was observed and the baby boy was in a good general condition at the sixth month follow-up visit [Table/Fig-3a,b].
a) Control electrocardiography demonstrated the normal sinus rhythm at six months; b) Control transthoracic echocardiographic examination showed increased left ventricular systolic function and reduced mitral valve insufficiency at six months.
Discussion
The frequency of cardiac arrhythmias in pregnancy is not well established. In one large retrospective survey of cardiac arrhythmia during pregnancy, a relatively high frequency of SVT was reported (24/100 000) [2]. Some of these attacks can be severe or haemodynamically important and should be treated effectively and safely. Therapies may include pharmacological and non-pharmacological options.
The data on the efficacy and safety of antiarrhythmic drugs in pregnancy is generally based on small case series and experts reports. The majority of antiarrhythmic drugs are Food and Drug Administration category C class teratogens, meaning that there is chance of foetal harm but the potential benefits outweigh the risk. Li JM et al., reported that in their study, 90% of 33 episodes of SVT occurred in the third trimester, during labor and delivery, or immediately postpartum. Different interventions (adenosine in 17, procainamide in three, verapamil in two, metoprolol in one of 23 episodes) were all effective in terminating these tachycardia without adverse outcome [2]. Ten episodes terminated spontaneously without pharmacologic intervention. After the adenosine treatment, in two patients there was transient maternal bradycardia, one patient had a short lasting uterine contraction. In another patient, intravenous administration of digoxin and verapamil after failure to terminate SVT with adenosine resulted in foetal bradycardia and urgent cesarean delivery was needed.
In our patient Valsalva maneuver and carotid massage was not effective in terminating tachycardia. The arrhythmia did not respond to intravenous adenosine, metoprolol and digoxin therapy and tachycardia continued with a 1:1 AV conduction. She was given intravenous amiodarone for this potentially life-threatening tachyarrhythmia. Although tachycardia rate decreased slightly, maternal haemodynamic condition got worse and amiodarone was stopped immediately. During the drug treatment period, patient was followed more closely for side effects and haemodynamic status. It is possible that more severe or unexpected side effects of antiarrhythmic drugs could be exist in pregnant patient with structural heart disease and/or decreased baseline ejection fraction [3]. On the other hand, untreated maternal arrhythmias can lead to decreased cardiac output and congestive heart failure in the mother, and adverse foetal events. Adverse foetal events including prematurity, respiratory distress syndrome and small fetus for gestational age have been reported in up to 20% of pregnancies [4]. Considering them all, in our case electric cardioversion was performed after the drugs treatment failed but conversion to sinus rhythm did not occur. Electrical cardioversion has been performed with success in the treatment of various arrhythmia during pregnancy [5]. It is assumed safe for both mother and child. However, it cannot terminate the ectopic atrial tachycardia [6] and can lead to a sustained uterine contraction, causing foetal distress, necessitating emergency caesarean section [7].
In our case rate and rhythm control attempts failed, without causing foetal side effects. Since tachycardia was intractable and had potentially life-threatening consequences for mother and fetus, we decided to ablate the tachycardia. It was described in previous case reports that, pregnant patients with right atrial tachycardia underwent catheter ablation [8-11]. The indications for ablation are incessant tachycardia refractory medical therapy, tachycardiomyopathy, congestive heart failure and left ventricular systolic dysfunction. The ablation procedure used radiofrequency energy and there were no procedural complication. After giving birth, both mother and the child were healthy.
The P wave morphology is particularly useful in determining the likely localisation of the responsible focus for tachycardia and procedure time. In present case, ECG showed a right atrial origin with positive in a VL, negative in inferior leads, and a positive-negative pattern in V1. Diagnosis and RF ablation of focal atrial tachycardia was made according to standard electrophysiological criteria. During the procedure maternal hypotension occurred before the RF ablation had been completed. General anaesthesia, aortocaval compression by the gravid uterus, vagal reflex and rapid pacing might play role in the development of hypotension [10]. Foetal heart rate reduction occurred following maternal hypotension was not resolved after augmentation of the maternal blood pressure and emergent caesarean delivery had been performed. In a newly published literature, uterine contraction and reduced blood pressure were reported during RF catheter ablation of pregnant women with rapid arrhythmia [12]. Therefore, continuous foetal monitoring and facilities for emergency caesarean section should be considered during catheter ablation in pregnant patient within the 24 weeks or more of gestation [10].
Focal atrial tachycardia, especially incessant nature of focus, has been well described as an important cause of reversible left ventricular dysfunction [13]. After successful ablation of the ectopic foci, there was complete recovery of left ventricular function in this pregnant patient including presented case [9,11]. No recurrences were reported during follow-up period.
Conclusion
Catheter ablation can be performed in pregnant patients with highly symptomatic, recurrent, drug-refractory SVT using radiation reduction technologies although it can carry some risks for both the mother and the foetus. In the management of maternal and fetal risk conditions, approaches of multidisciplinary team are important. It is also worth to note that emergent availability of surgical delivery options should be part of the procedural planning.
[1]. Couchonnal LF, Knight B, How to rapidly diagnose supraventricular tachycardia in the electrophysiology lab. in: hands on ablation 2013 MinnesotaCardiotest Publishing [Google Scholar]
[2]. Li JM, Nguyen C, Joglar JA, Hamdan MH, Page RL, Frequency and outcome of arrhythmias complicating admission during pregnancy: experience from a high-volume and ethnically-diverse obstetric serviceClin Cardiol 2008 31(11):538-41.10.1002/clc.2032619006111 [Google Scholar] [CrossRef] [PubMed]
[3]. Lee MS, Evans SJ, Blumberg S, Bodenheimer MM, Roth SL, Echocardiographically guided electrophysiologic testing in pregnancyJ Am Soc Echocardiogr 1994 7(2):182-86.10.1016/S0894-7317(14)80126-0 [Google Scholar] [CrossRef]
[4]. Silversides CK, Harris L, Haberer K, Sermer M, Colman JM, Siu SC, Recurrence rates of arrhythmias during pregnancy in women with previous tachyarrhythmia and impact on fetal and neonatal outcomesAm J Cardiol 2006 97(8):1206-12.10.1016/j.amjcard.2005.11.04116616027 [Google Scholar] [CrossRef] [PubMed]
[5]. Enriquez AD, Economy KE, Tedrow UB, Contemporary management of arrhythmias during pregnancyCirc Arrhythm Electrophysiol 2014 7(5):961-67.10.1161/CIRCEP.114.00151725336366 [Google Scholar] [CrossRef] [PubMed]
[6]. Tromp CH, Nanne AC, Pernet PJ, Tukkie R, Bolte AC, Electrical cardioversion during pregnancy: safe or not?Neth Heart J 2011 19(3):134-36.10.1007/s12471-011-0077-521475392 [Google Scholar] [CrossRef] [PubMed]
[7]. Barnes EJ, Eben F, Patterson D, Direct current cardioversion during pregnancy should be performed with facilities available for fetal monitoring and emergency caesarean sectionBJOG 2002 109(12):1406-07.10.1046/j.1471-0528.2002.02113.x12504980 [Google Scholar] [CrossRef] [PubMed]
[8]. Szumowski L, Szufladowicz E, Orczykowski M, Bodalski R, Derejko P, Przybylski A, Ablation of severe drug-resistant tachyarrhythmia during pregnancyJ Cardiovasc Electrophysiol 2010 21(8):877-82.10.1111/j.1540-8167.2010.01727.x20158563 [Google Scholar] [CrossRef] [PubMed]
[9]. Berruezo A, Diez GR, Berne P, Esteban M, Mont L, Brugada J, Low exposure radiation with conventional guided radiofrequency catheter ablation in pregnant womenPacing Clin Electrophysiol 2007 30(10):1299-302.10.1111/j.1540-8159.2007.00858.x17897139 [Google Scholar] [CrossRef] [PubMed]
[10]. Driver K, Chisholm CA, Darby AE, Malhotra R, Dimarco JP, Ferguson JD, Catheter ablation of arrhythmia during pregnancyJ Cardiovasc Electrophysiol 2015 26(6):698-702.10.1111/jce.1267525828853 [Google Scholar] [CrossRef] [PubMed]
[11]. Zuberi Z, Silberbauer J, Murgatroyd F, Successful non-fluoroscopic radiofrequency ablation of incessant atrial tachycardia in a high risk twin pregnancyIndian Pacing Electrophysiol J 2014 14(1):26-31.10.1016/S0972-6292(16)30712-4 [Google Scholar] [CrossRef]
[12]. Chu L, Zhang J, Li YN, Long DY, Clinical analysis of 19 cases of pregnant women with rapid arrhythmia in the treatment of radiofrequency catheter ablationZhonghua Fu Chan Ke Za Zhi 2016 51(10):759-64. [Google Scholar]
[13]. Medi C, Kalman JM, Haqqani H, Vohra JK, Morton JB, Sparks PB, Tachycardia-mediated cardiomyopathy secondary to focal atrial tachycardia: long-term outcome after catheter ablationJ Am Coll Cardiol 2009 53(19):1791-97.10.1016/j.jacc.2009.02.01419422986 [Google Scholar] [CrossRef] [PubMed]