Etomidate, a carboxylated imidazole compound, is a rapidly acting non barbiturate non-opioid hypnotic agent causing minimal histamine release and very stable haemodynamic profile [1]. The haemodynamic stability seen with etomidate may be partly due to its unique lack of effect on sympathetic nervous system and on baroreceptor function [5]. The present study was designed to study and compare the haemodynamic response during induction and incidence of myoclonus with etomidate and propofol in adult patients of ASA Grade I and II posted for elective surgery.
Materials and Methods
The present study was conducted in prospective randomised controlled order at Government Medical College and Rajindra Hospital Patiala from September 2014 to July 2016 in which 100 adult patients of ASA Grade I and II in the age group of 18 to 60 years of either sex, scheduled for elective surgery under general anaesthesia were included. The sample size was calculated assuming a 5% two-tailed significance level (a=0.05) and power of 80% (b=0.20), to detect 10% absolute difference in the incidence of myoclonic movements (i.e., from 32% to 40%). An approval from Institution’s Ethical and Research Committee was taken. The exclusion criteria for the study was patients with history of epilepsy and seizure disorder, suspected or detected neurological, neuromuscular or psychiatric disorder, history of cardiovascular or respiratory abnormalities, severe hepatic or renal disease, gastro oesophageal reflux disease, full stomach patients, allergy/hypersensitivity to study drugs, known adrenal insufficiency and suppressed immune function. Written and informed consent was taken from all the patients who were included in the study.
The day before surgery, a detailed pre-anaesthetic check-up was carried out in every patient. History, general physical examination along with detailed systemic examination was done. Assessment of airway examination (movement of neck, loose tooth, artificial dentures, mallampati grading) was done. Investigations like haemoglobin, Total Leucocyte Count (TLC), Differential Leucocyte Count (DLC), Bleeding time, Clotting time, random blood sugar, liver function tests, renal function tests, urine for albumin and sugar, X-ray chest and Electrocardiography (ECG) were done. Patients were advised to stay fasting for eight hours before the surgery.
The patients were randomly allocated into two groups of 50 each. Random allocation was performed with a randomisation code with sealed envelope. Randomised procedure was applied by individual independent of the study where odd numbered case was assigned to Group P and even to Group E. Group P (n=50) received injection propofol 2 mg/kg body weight intravenously and Group E (n=50) received injection etomidate 0.3 mg/kg body weight intravenously for induction. The syringes containing either propofol or etomidate 20 mL each were prepared. On the day of surgery, each patient was given injection (inj.) Midazolam 2 mg Intramuscular (i.m) and inj. Phenergan 25 mg i.m half hour prior to surgery as premedication. Patients were shifted to operating room and multiparameter monitor was attached and monitoring was started. Baseline heart rate, SBP, DBP, MAP, SpO2 and EtCO2 were recorded before. Intravenous access was established using an 18 G cannula. Inj. glycopyrolate 0.004 mg/kg body weight i.v and inj. fentanyl 2 mcg/kg body weight i.v were given just before induction. Patients were preoxygenated with 100% oxygen via an anatomical facemask for five minutes. In Group P, the patients were given injection propofol 2 mg/kg body and in Group E, patients were given injection etomidate 0.3 mg/kg body weight intravenously for induction. Time taken to produce loss of eyelash reflex was taken as an induction time. inj. succinylcholine 1.5 mg/kg body weight i.v. was given to facilitate endotracheal intubation with appropriate size cuffed endotracheal tube, which was performed 60 seconds after giving the injection. After checking and securing the endotracheal tube, anaesthesia was maintained with intermittent positive pressure ventilation using Bains circuit with N2O and O2 (70:30), inhalational agent 0.5-2% isoflurane and using vecuronium bromide as muscle relaxant. At the end of surgery, the residual neuromuscular block was antagonised with neostigmine (0.05 mg/kg) and glycopyrrolate (0.01 mg/kg) i.v and extubation was performed when respiration was adequate and patient was able to obey verbal commands.
Monitoring
The haemodynamic parameters including HR, SBP, DBP, MAP, SpO2 and EtCO2 were continuously monitored and recorded before induction, immediately after induction, at intubation and then every 1 minute till 10 minutes and every 2 minutes till 20 minutes after intubation. Any myoclonus during induction was noted and documented.
Statistical Analysis
The data from the present study were analysed statistically to draw relevant conclusions. Unpaired t-test was used for continuous variables and chi-square test and Fisher-exact test was used for categorical variables. Statistical significance was taken as p<0.05. The observations were depicted in tables. EpiInfo software (7.1.0.6 version; Center for disease control, USA) and Microsoft Excel 2010 were used for analysing data.
Results
Demographic variables were comparable in both the groups [Table/Fig-1].
Demographic profile of patients.
| Patient profile | Group E | Group P | p-value | Significance |
|---|
| Age in years | 40.30±12.03 | 39.06±11.52 | 0.5998 | NS |
| Sex |
| Male | 13 | 15 | 0.6560 | NS |
| Female | 37 | 35 |
| Weight in kg | 60.48±4.20 | 61.16±7.46 | 0.6654 | NS |
| ASA grade |
| Grade I | 36 | 37 | 0.8218 | NS |
| Grade II | 14 | 13 |
NS: Non significant
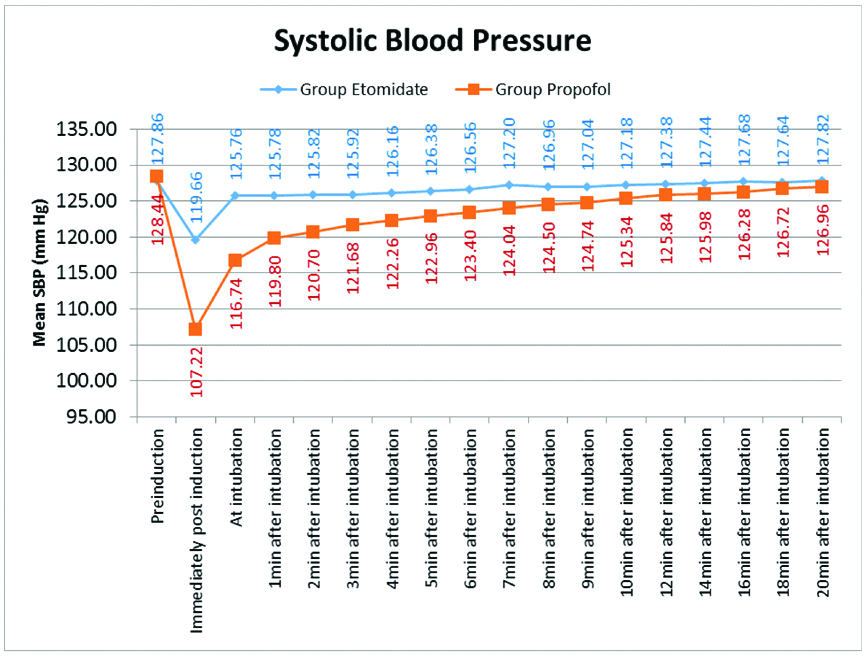
As shown in [Table/Fig-2], the baseline mean SBP of both the groups was comparable (p>0.05). Immediately post-induction, there was a significant (p<0.05) fall in mean SBP in Group P as compared to Group E. At intubation there was a rise in mean SBP from immediately post-induction value; however, it was still significantly lower in Group P (p<0.05). Then, the mean SBP was significantly lower in Group P at 1, 2, 3, 4, 5, 6, 7, 8, 9 and 10 minutes after intubation. However, after 10 minutes, the difference in mean SBP in both the groups was statistically insignificant (p>0.05)
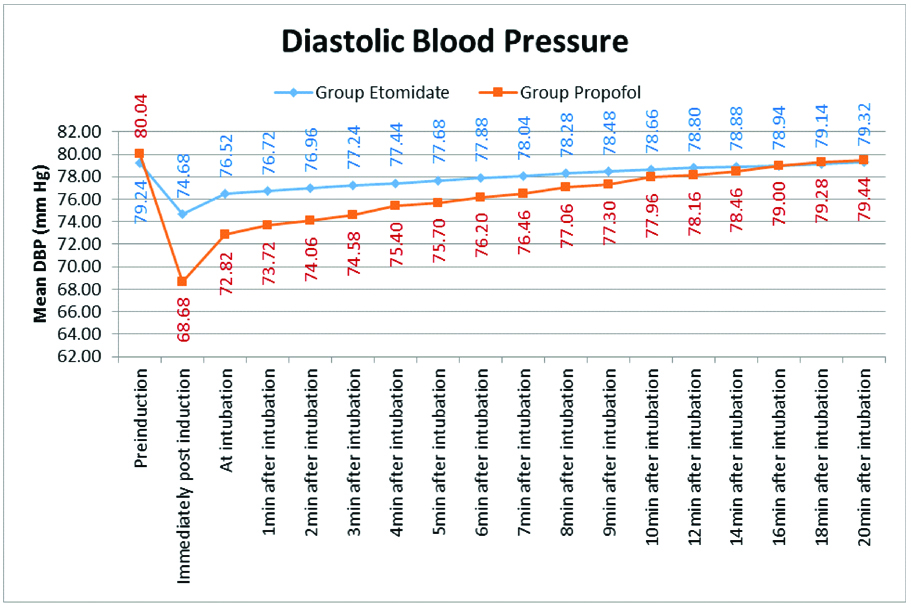
As shown in [Table/Fig-3], the baseline mean DBP of both the groups was comparable (p>0.05). Immediately post-induction, there was a significant (p<0.05) fall in mean DBP in Group P as compared to Group E. At intubation there was a rise in mean DBP from immediately post-induction value; however, it was still significantly lower in Group P (p<0.05). After intubation, the difference in mean DBP in both the groups was statistically insignificant (p>0.05).
Diastolic blood pressure.
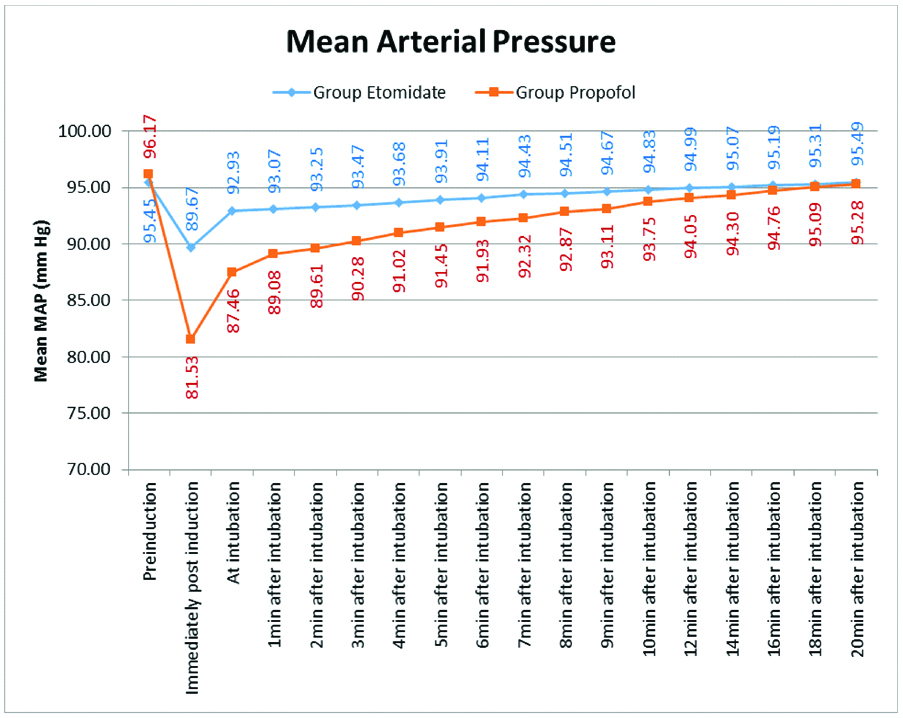
As shown in [Table/Fig-4,5], the baseline MAP of both the groups was comparable (p>0.05). Immediately post-induction, there was a significant (p<0.05) fall in MAP in Group P as compared to Group E. At intubation there a was rise in arterial blood pressure from immediately post-induction value but it was still significantly lower in Group P (p<0.05). Then the MAP was significantly lower in Group P at 1, 2, 3, 4, 5, 6 minute after intubation. But after six minutes, the difference in MAP in both the groups was statistically insignificant (p>0.05).
| Mean Arterial Pressure (mmHg) | Group Etomidate | Group Propofol | p-value Unpaired t Test | Significance |
|---|
| Intubation period | Mean | SD | Mean | SD |
|---|
| Pre-induction | 95.45 | 5.55 | 96.17 | 5.72 | 0.5204 | NS |
| Immediately post-induction | 89.67 | 5.44 | 81.53 | 5.29 | <0.0001 | S |
| At intubation | 92.93 | 5.56 | 87.46 | 5.10 | <0.0001 | S |
| 1 minute | 93.07 | 5.65 | 89.08 | 5.11 | 0.0004 | S |
| 2 minutes | 93.25 | 5.63 | 89.61 | 5.08 | 0.0010 | S |
| 3 minutes | 93.47 | 5.67 | 90.28 | 4.94 | 0.0035 | S |
| 4 minutes | 93.68 | 5.76 | 91.02 | 4.99 | 0.0153 | S |
| 5 minutes | 93.91 | 5.81 | 91.45 | 5.05 | 0.0261 | S |
| 6 minutes | 94.11 | 5.76 | 91.93 | 5.12 | 0.0490 | S |
| 7 minutes | 94.43 | 5.86 | 92.32 | 5.18 | 0.0598 | NS |
| 8 minutes | 94.51 | 5.66 | 92.87 | 5.18 | 0.1353 | NS |
| 9 minutes | 94.67 | 5.66 | 93.11 | 5.20 | 0.1563 | NS |
| 10 minutes | 94.83 | 5.66 | 93.75 | 5.31 | 0.3279 | NS |
| 12 minutes | 94.99 | 5.73 | 94.05 | 5.36 | 0.3992 | NS |
| 14 minutes | 95.07 | 5.71 | 94.30 | 5.30 | 0.4882 | NS |
| 16 minutes | 95.19 | 5.73 | 94.76 | 5.42 | 0.7030 | NS |
| 18 minutes | 95.31 | 5.62 | 95.09 | 5.48 | 0.8480 | NS |
| 20 minutes | 95.49 | 5.71 | 95.28 | 5.47 | 0.8537 | NS |
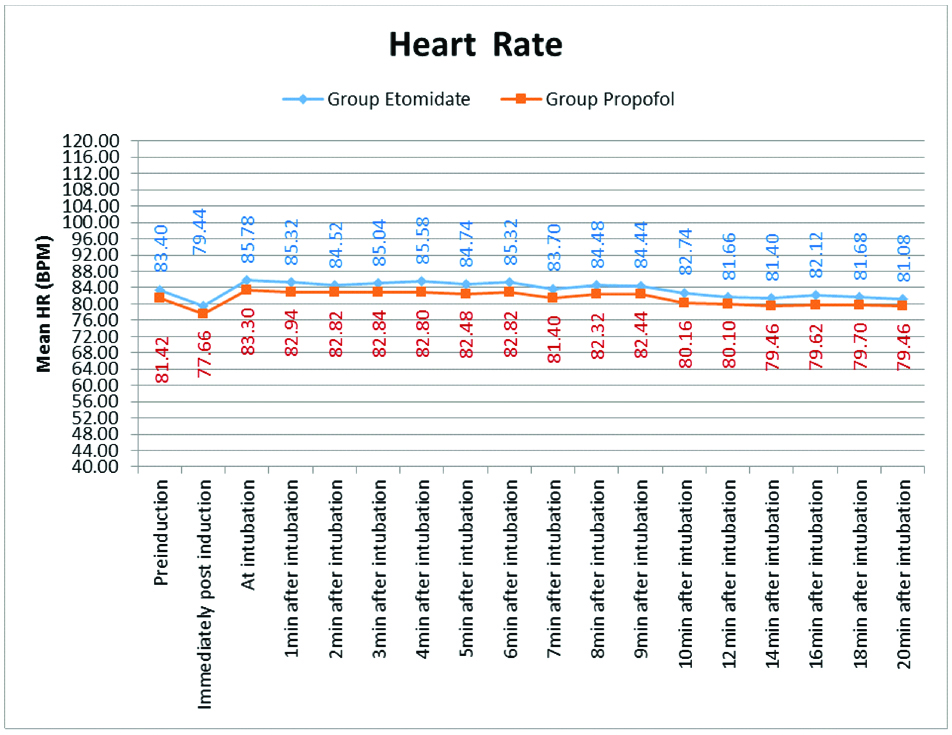
As shown in the [Table/Fig-6]. The mean heart rate was comparable in both the groups from pre-induction to 20 minute post-induction (p>0.05).
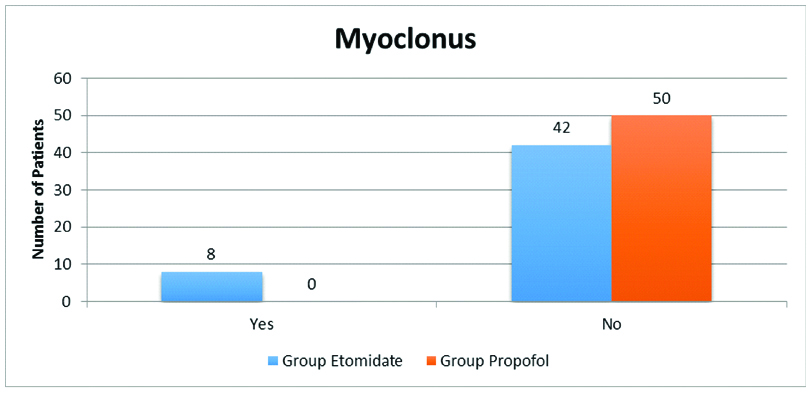
As shown in the [Table/Fig-7], myoclonus was significantly higher in Group E as compared to Group P (p<0.0029).
Discussion
General anaesthetic induction agents may decrease arterial blood pressure via myocardial depression, vasodilatation and attenuation of autonomic nervous activity [6]. Sudden hypotension, arrthymias and cardiovascular collapse are life threatening complications following injection of induction agent. It is desirable to use a safe agent with fewer cardiovascular effects [7]. In the present study, we observed that there was a statistically significant reduction in SBP, DBP and MAP at induction with propofol as compared to etomidate.
The mean SBP measured before induction was stable and comparable in two groups (p>0.05). Immediately after induction, SBP decreased in both the groups but fall was significantly (p<0.05) more in the propofol group (mean SBP 107.22±3.70) as compared to etomidate group (mean SBP 119.66±5.35) [Table/Fig-2]. Ebert TJ et al., also reported hypotension during induction with propofol. This study explained potential mechanisms leading to hypotension by recording cardiovascular responses [8]. Masoudifar M and Beheshtian E, also reported a significant fall in SBP with propofol (26.1%) as compared to etomidate (8%) in patients undergoing elective orthopedic surgeries [9]. Kaur S et al., and Shah SB et al., also reported a fall in SBP-value from baseline in both the groups post-induction but the fall in propofol group was significantly more than etomidate group [1,6].
In the present study, the mean DBP measured before induction was stable and comparable in two groups (p>0.05). Immediately after induction, DBP decreased in both the groups but fall was significantly (p<0.05) more in the propofol group (mean DBP 68.68±7.47) as compared to etomidate group (mean DBP 74.68±7.69) as shown in [Table/Fig-3]. Similar results were obtained by Kaur S et al., Mayer M et al., and Desai PM et al., [1,10,11]. They reported a significant fall in DBP on induction with propofol as compared to etomidate. Das M et al., reported that in etomidate group, post-induction and after intubation, DBP did not change significantly. However, in propofol group DBP decreased significantly after induction [12].
In the present study, MAP measured before induction was stable and comparable in two groups (p>0.05). Immediately after induction, MAP decreased in both the groups but fall was significantly (p<0.05) more in the propofol group (mean MAP 81.53±5.29) as compared to etomidate group (mean MAP 89.67±5.44) [Table/Fig-4,5]. Similar results were obtained by Aggarwal S et al., Desai PM et al., Toklu S et al., and Ghafoor HB et al., who reported a significant fall in MAP after induction with propofol. Etomidate shows less cardiovascular depression and minimise use of vasopressor agents [7,11,13,14]. Contrary to present results, Sharma A et al., reported that changes in MAP with both propofol and etomidate were statistically not significant [3].
The mean heart rate of all patients was comparable in both groups from preinduction to 20 minutes post-induction The difference in mean heart rate between the two groups was statistically insignificant (p>0.05) [Table/Fig-6]. Similar results were obtained by Sharma A et al., Desai PM et al., and Das M et al., [3,11,12]. However, Aggarwal S et al., reported a significant increase in heart rate from baseline at induction in propofol group (p>0.05). After that it became comparable to etomidate (p>0.05) [7]. Kapoor N et al., reported that propofol causes sustained decrease in heart rate compared to etomidate with p-value <0.05 at 60 and 80 seconds. The effect is because Propofol resets the baroreflexes to allow slower hearts at lower arterial pressures [15].
There was no statistical difference in SpO2 and EtCO2 of patients in the two groups at all times (p>0.05).
In the present study myoclonic movements were seen in 8 out of 50 patients given etomidate as induction agent whereas with propofol no myoclonic movements were seen. The difference was statistically significant (16% in etomidate group versus 0% in propofol group) [Table/Fig-5]. Miner JR et al., reported myoclonus with both propofol and etomidate but the incidence was significantly high in etomidate group (20%) as compared to propofol group (1.8%) [16]. Similar results were obtained by Aggarwal S et al., and Desai PM et al., [7,11]. Contradictory to present result, Sharma A et al., reported a statistically significant increased incidence of myoclonus with propofol (out of 30 patients 15 had myoclonus) as compared to etomidate (out of 30 patients 4 had myoclonus) [3]. The neurologic mechanism of myoclonus is unclear. It may be a disinhibition phenomenon presumably because large doses of etomidate depress cortical activity before they depress subcortical activity [17]. Various studies have been done to device methods to prevent myoclonus due to etomidate e.g., pretreatment with benzodiazepines (midazolam 0.03 mg/kg i.v), opiates (fentanyl 1 mcg/kg i.v), rocuronium (0.06 mg/kg i.v), dexmedetomidine (0.5 mcg/kg in 10 mL isotonic saline or 1 mcg/kg in 10 mL isotonic saline i.v), magnesium sulphate (60 mg i.v), small doses of etomidate (0.03-0.05 mg/kg 50-60 seconds before an etomidate bolus) [17-21]. Slow rate of injection of the drug may also decrease the incidence of myoclonus [22].
Limitation
In the present study, authors did not measure the drug levels in blood and plasma cortisol or adrenocorticotrophin levels. Authors did not perform blinding and did not use Bispectral Index (BIS) to measure depth of anaesthesia and did not conduct a cost-effectiveness analysis.
Conclusion
In conclusion, Etomidate is better inducing agent than propofol with regard to cardiovascular stability. The drawback is high incidence of myoclonus which is manageable.
NS: Non significant