Extra G Positive Band on Long Arm of Chromosome 9 and Long Y-Chromosome in a Patient Presenting with Infertility: A Case Report
Afreen Aftab1, Kundavi Shankar2, Bibhas Kar3
1 Research Assistant, Center for Genetic Studies and Research, The Madras Medical Mission, Chennai, Tamil Nadu, India.
2 Senior Consultant and Head, Institute of Reproductive Medicine and Women’s Health, The Madras Medical Mission, Chennai, Tamil Nadu, India.
3 Consultant and Head, Center for Genetic Studies and Research, The Madras Medical Mission, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bibhas Kar, 4-A, JJ Nagar, Mogappair, Chennai-600037, Tamil Nadu, India.
E-mail: drbibhaskar65@gmail.com
This is a case report of a male patient with rare 9qh+ variant containing extra G positive band along with an increase in heterochromatin in the long arm of Y-chromosome, presenting with primary infertility. There have been various reports on the involvement of 9h+ variation in infertility. In this case, the association maybe coincidental and not causal as the proband’s mother was also presented with similar 9qh+ variation and hence, is not infertile. Besides Yqh+ has been reported to be involved in male factor infertility or subfertility. There have been reports suggesting that epigenetic modifications accompanying cases of inherited heterochromatin polymorphisms may lead to phenotypic effects with clinical significance such as infertility that may not be seen in the parents.
Chromosomal aberration, Constitutive heterochromatin, Male infertility
Case Report
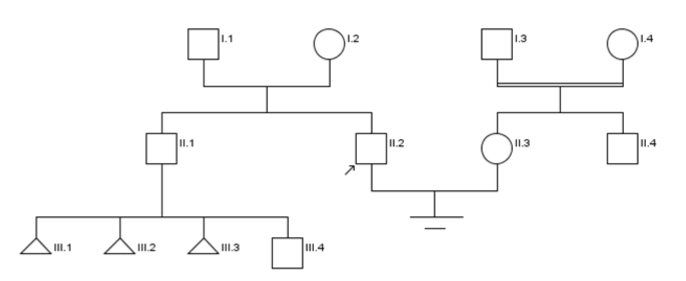
In this report we depict a case where a couple, a 29-year-old man and 26-year-old woman, reported with a history of infertility for two and a half years. They underwent preliminary tests including biochemical, haematological and serological assessments. They were found to be infection free and their hormonal levels were within normal range. The ultrasound reports of the female were found to be normal. The semen analysis of the male patient showed Severe Oligoasthenoteratozoospermia (SOAT). Upon physical examination, he had normal appearing testes. KUB (Kidney, Ureter, Bladder) radiography showed absence of varicocele and the ultrasound reported normal epididymis. The couple was referred for genetic testing due to SOAT. After pedigree analysis [Table/Fig-1], informed consent was collected from the subjects to perform karyotyping for the couple as well as test for Y-chromosome microdeletion for the male patient to indicate the presence or absence of two STS sequences in AZFa, three in AZFb and four in AZFc regions of the Y chromosome. They also provided consent for the use of their test results for research.
Pedigree of proband’s family.
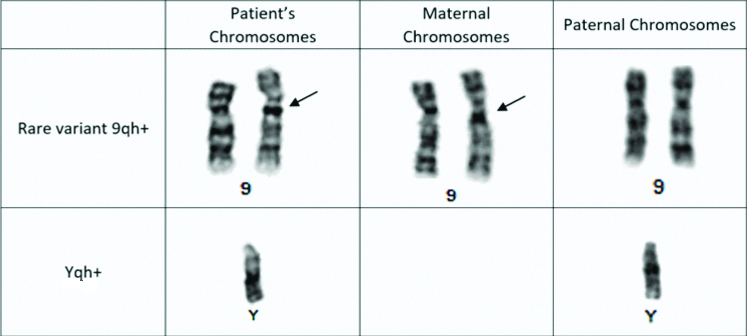
The karyotyping was done using the peripheral blood lymphocytes which were cultured for 72 hours in RPMI-1640 medium supplemented with foetal bovine serum and phytohaemagglutinin. The chromosomes were stained by GTG banding technique. Twenty metaphases were analysed which revealed a rare variant 9qh+ having an extra G band on the q arm of chromosome 9 and increase in heterochromatin region on the long arm of Y-chromosome also known as long Y-chromosome (Yqh+) [Table/Fig-2]. The Y-chromosome microdeletion test done using multiplex Polymerase Chain Reaction (PCR) was reported negative for Y-chromosome microdeletion for the regions tested.
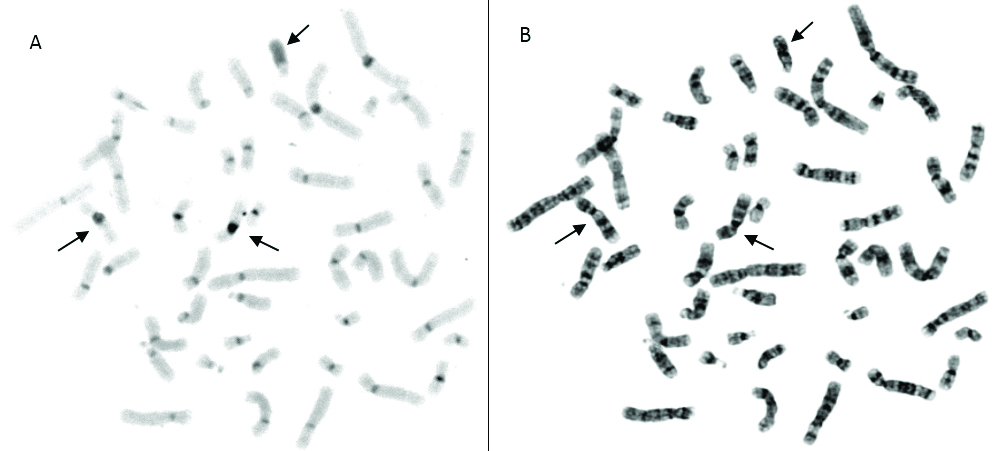
The family history of both patients was unremarkable except for the brother of the male patient whose wife had three repeated pregnancy losses prior to the birth of a healthy baby boy, conceived naturally. The karyotype of the patient’s wife was found to be normal. The couple was advised to undergo further analysis and parental karyotyping. C-banding analysis was done with the patient’s sample to determine the nature of the heterochromatin in the extra G band. C-banding revealed no extra band in chromosome 9. The staining patterns of both the normal and variant chromosome 9s were similar indicating that the extra G positive band is composed of constitutive heterochromatin and present within the C band of the chromosome 9 [Table/Fig-3]. Parental karyotyping was done, and it was found that the mother of the patient was a carrier as she had an extra G band in the q arm of chromosome 9. The father’s karyotype showed Yqh+ [Table/Fig-2].
Partial G banded karyotype showing the proband’s and parental 9 and Y chromosomes*.
*Arrows indicating extra G positive band in chromosome 9 of both proband and maternal sample
C-Banding of proband’s chromosomes*; a) image of C banded metaphase; b) image of G banded matched metaphase.
*Arrows pointing at both 9 and Y chromosomes
It was found that the proband who carried the 9qh+ and Yqh+ variants was infertile but his mother who carried the 9qh+ variant and father who carried Yqh+ variant chromosomes were found to be fertile.
Discussion
The karyotype analysis showed that the proband had inherited the variant chromosome 9 containing extra G positive band from the mother. However, since the mother was able to conceive and bear two children despite the chromosomal aberration the proband’s infertility may be coincidental and not associated with the extra G positive band in chromosome 9. This also indicates that this variant maybe familial in nature. The proband also inherited his father’s variant Y-chromosome. The proband’s brother has not provided his sample for testing. Hypothetically, if the brother only has Yqh+ and a normal chromosome 9 from the mother, then the impact of the chromosomal polymorphism may not be as influential as with the presence of both chromosomal variations.
Male factor infertility is a growing concern due to its rapidly rising rates. It not only affects one’s ability to procreate, but it also has an emotional, psychological, familial and societal impact. There have been several reports regarding the involvement of chromosomal variants in male infertility; one of the genetic factors involved is heterochromatin variation. The chromosome 9 variants are widely debated to play a role with some reports arguing against its significance. It is well known that genetic predisposition and/or environmental factors can play a significant role in infertility [1].
Heterochromatin defects can affect kinetochore assembly, centromere function and chromosome segregation which can lead to spermatozoa with aneuploidies. Chromosome 9 has been known to have several heteromorphic variants. One of the reasons may be the high incidence of breaks producing asymmetric bivalents in meiotic metaphase I stage and structural chromosomal aberrations in later stages of spermatogenesis. Such variants are more commonly found in the general population than compared to DNA sequence changes that may lead to genetic diseases. Morphological differences between the homologous chromosomes 9 could result in faulty crossing over thereby producing aberrant gametes. Although, not all of these variants are known to be clinically significant and hence, they are not deemed as mutations [2-4].
The variations in the Y-chromosome may possibly occur due to the gene transcription inhibition because of the silencing effect on the genes/gene promoters in close proximity. Y-chromosome heteromorphisms may or may not be of clinical significance but reports exist which suggest that epigenetic modifications of the heterochromatic region of the Y-chromosome may play a factor in male factor infertility. Long Y-chromosome has also been associated with foetal loss. Nagvenkar P et al., observed that there was an occurrence of Yqh+ in 3.4% of the Indian male population [5,6].
However, so far, the specific epigenetic mechanisms and the degree to which altered chromosomal state can influence infertility associated with pericentromeric blocks of heterochromatin on both chromosomes 9 and Y are largely unknown. Such studies could help us to understand idiopathic infertility [7]. Such cases of infertility can be managed by utilisation of rapidly advancing techniques such as Intra Cytoplasmic Sperm Injection (ICSI), In Vitro Fertilisation (IVF), sperm donation etc., if necessary [5,8].
Furthermore, studies can be done by performing tests such as a FISH sperm segregation study of chromosome 9 to understand the origin of the aneuploidies and a Sperm Aneuploidy Test (SAT) to study the possibility of Inter-Chromosomal Effect (ICE) which may shed light on this problem.
Conclusion
In conclusion extra GTG-positive and CBG-negative bands in the 9q region, without clinical consequence have been reported in several families although they may be associated with normal, abnormal, autistic and leukaemic phenotypes in some cases. There are several reports on the involvement of 9h+ variation in infertility with some saying that it is coincidental, and some saying that is directly related with no conclusive evidence. Hence further extensive genetic investigation is required along with counselling to understand the function of the heteromorphic region.
[1]. Carrell DT, The Genetics of Male Infertility 2007 1st ed10.1007/978-1-59745-176-5 [Google Scholar] [CrossRef]
[2]. Jorde Lynn B. Carey, John C, Bamshad MJ, Medical Genetics 2009 4th ed10.1016/B978-0-323-05373-0.00011-7 [Google Scholar] [CrossRef]
[3]. Madon PF, Athalye AS, Parikh FR, Polymorphic variants on chromosomes probably play a significant role in infertilityReprod Biomed Online 2005 11(6):726-32.10.1016/S1472-6483(10)61691-4 [Google Scholar] [CrossRef]
[4]. Kosyakova N, Grigorian A, Liehr T, Manvelyan M, Simonyan I, Mkrtchyan H, Heteromorphic variants of chromosome 9Mol Cytogenet 2013 6:1410.1186/1755-8166-6-1423547710 [Google Scholar] [CrossRef] [PubMed]
[5]. Christofolini DM, Mafra FA, Neto RP, Augusto R, Almeida S De, Amaro A, Correlation between chromosomal variants and male infertility in a population of Brazilian infertile menReproductive Sys Sexual Disord 2012 1(1):01-06.10.4172/2161-038X.1000105 [Google Scholar] [CrossRef]
[6]. Nagvenkar P, Desai K, Hinduja I, Zaveri K, Chromosomal studies in infertile men with oligozoospermia & non-obstructive azoospermiaIndian J Med Res 2005 122(1):34-42. [Google Scholar]
[7]. Minocherhomji S, Madon PF, Parikh FR, Epigenetic regulatory mechanisms associated with infertilityObstet Gynecol Int 2010 2010:19870910.1155/2010/19870920814440 [Google Scholar] [CrossRef] [PubMed]
[8]. Pangjaidee N, Suphakom T, Luewan S, Characterization of extra euchromatic band in the 9qh region 2015 54(2) [Google Scholar]