Sepsis is responsible for approximately 30% of in-hospital mortality, with increasing incidence and elevated associated hospitalization costs [1-3]. One third of patients with sepsis are admitted through the Emergency Department (ED) [2-6]. It has been shown that patients admitted to ED and receiving early goal-directed therapy had a 30.5% mortality compared to 46.5% in the group that received standard therapy [7]. However, the window of opportunity to prevent morbidity and mortality occurs during the early phases of sepsis presentation [6].
In 2016, a task force organised by national societies, including the Society of Critical Care Medicine and the European Society of Intensive Care Medicine, sought to update the definition of sepsis and differentiate it from that of uncomplicated infection to be consistent with an improved understanding of the pathobiology [8,9]. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) therefore defined sepsis as a life-threatening organ dysfunction associated to a dysregulated response to infection [8,9]. In this new proposal, both, the use of host inflammatory response syndrome criteria (SIRS) and the term “severe sepsis” have been removed [4,5,8,9]. Moreover, the task force introduced the quick-SOFA (qSOFA) score, a modified and simplified method of the Sequential (Sepsis-related) Organ Failure Assessment score (SOFA), to facilitate the identification of those at risk of dying from sepsis [4,8,10].
Quick-SOFA could be an easy to use and efficient tool for predicting in-hospital mortality and sepsis outside the intensive care unit but its utility disappears in the critical care setting [11]. For patients with infection outside of the Intensive Care Unit (ICU), it is important to recognise sepsis early; however, criteria for organ dysfunction require laboratory data that may prove difficult to obtain [4]. Therefore, the use of a qSOFA score of 2 points or above in encounters with patients with infection in non-ICU settings to consider risk of developing sepsis was recommended [4] Recently, qSOFA showed better discriminative value and hazard ratio than previous criteria for predicting death [12]. To further assess the score, we sought to evaluate mortality rate in ED along with predicting sepsis by Quick-SOFA.
Materials and Methods
The study was of an observational and prospective design, performed between May and November 2016 at a private tertiary care teaching hospital in Buenos Aires, Argentina. The study has been approved by the Hospital Ethics Committee and complies with Argentinean and international ethical norms, with Argentine Act 25326/Habeas Data as well as with norms of the Argentina Drugs Administration (ANMAT).
Included patients were ≥18 years of age, who were presented to the ED and were admitted to a 15-bed observation area of ED, whose screening showed sepsis or infection, or any symptom consistent with an infection, including fever, cough, dysuria, diarrhoea, dyspnoea, sputum production, skin infection. Patients were excluded if they were <18-year-old, had neurological deterioration or cardio-respiratory disease, were on sedative or neuroleptic medication, including home medication treatment with benzodiazepines, suffered severe metabolic disorder, or an acid-base disorder. Patients with these pathologies were excluded as they may act as confounders and make identification of qSOFA variables difficult. The collected data included: age, sex, comorbidities (Charlson index), clinical and analytical data in the ED (altered metal status according to the Glasgow Coma Scale), heart rate (HR, per minute), respiratory rate (RR, per minute), temperature (°C), blood pressure (SBP, mmHg), oxygen saturation (SpO2, %), leucocyte count, and the site of infection (urinary, respiratory, abdominal, skin and soft tissue or other infections). Patients were followed up until in-hospital mortality or hospital discharge.
Data was pulled from the hospital’s electronic medical record system and chart reviews were completed by two trained physician researchers, who followed predetermined guidelines to determine the presence and timing of the components of qSOFA score and SIRS criteria. Two investigators reviewed abstracted data for discrepancies against electronic records and laboratory results. The following definitions from Sepsis-3 were used: organ dysfunction is an acute two point change in the total SOFA score resulting from an infection; sepsis is a life-threatening organ dysfunction associated with a dysregulated response by the host to an infection; septic shock is a subclass of sepsis with primary circulatory and metabolic anomalies serious enough to increase mortality [9]. Septic shock refers to sepsis with continuing hypotension that requires vasopressors to keep MAP 65 mm Hg and with serum lactate level of more than 2 mmol/L (18 mg/dL) despite volume resuscitation [9].
The primary outcome of interest was sepsis as defined above and the secondary outcome was in-hospital mortality. For qSOFA, the following data were used: 1 point for each of respiratory rate above 21 breaths per min, systolic arterial blood pressure ≤100 mm Hg, or altered mental status. A qSOFA score of ≥2 was considered positive. SIRS score included body temperature above 38°C or below 36°C, a respiratory rate of more than 20 breaths per minute, a heart rate of more than 90 beats per minute, and a white blood cell count of immature forms (bands). The score ranged from 0 to 4, one point was awarded for each condition; a SIRS score of ≥2 was considered positive [13].
Continuous variables are expressed as mean (SD) or (95% CI), or median (range), as appropriate; categorical variables are expressed as frequency and percentage. Comparisons were made using the Student’s t-test or Mann-Whitney’s test for continuous variables, Chi-square test and Fisher exact test for categorical variables, as appropriate. To assess how qSOFA and SIRS predicted sepsis and in-hospital mortality, sensitivity and specificity was calculated. The area under the receiver operating characteristic curves (AUC) for qSOFA and SIRS were calculated and compared. A p-value of <0.05 was considered to be statistically significant. All statistical analyses were carried out using Stata v15 (College Station, TX, USA).
Results
Of the total of 2304 patients who visited ED during the study period, 157 (6.8%) patients showed an infection or a suspicion of infection and were included in the analysis. Their mean age was 62.9 years (95% CI 59.9-65.9) and 76 (48.4%) patients were women. Upon admission, 58/157 (36.9%) patients showed a positive-qSOFA (with ≥2 signs) versus 99/157 (63.1%) patients who showed a negative-qSOFA (0 or 1 signs). For qSOFA assessment parameters, 52 (33.1%) patients presented respiratory rate of >21 breaths/min, 51 (32.5%) patients had systolic arterial blood pressure ≤100 mm Hg, and 34 (21.7%) patients had an altered mental status. SIRS score was positive (≥2 signs) in 120/157 (76.4%) patients versus 37/157 (23.6%) patients who showed a negative SIRS (0 or 1 signs). Fifty-four of 157 patients (34.4%) showed both positive SIRS and positive qSOFA. [Table/Fig-1] shows characteristics and outcomes of patients.
Characteristics and outcomes of patients.
| Characteristics and outcomes | Negative qSOFA N=99 | Positive qSOFA N=58 | p-value | Negative SIRS N=37 | Positive SIRS N=120 | p-value | Total |
|---|
| Age, years, Mean±SD | 62.0±20.4 | 64.4±16.9 | 0.44 | 66.8±17.2 | 61.9±19.7 | 0.24 | 62.9±19.2 |
| Women, n (%) | 44 (44.4) | 32 (55.2) | 0.194 | 20 (54.1) | 61 (50.8) | 0.732 | 76 (48.4) |
| Immunosuppression, n (%) | 43 (43.4) | 33 (56.9) | 0.072 | 17 (46) | 59 (49.2) | 0.732 | 76 (48.4) |
| Outcomes | | | | | | | |
| Lactate, <2 mmol/L, n (%) | 75 (75.8) | 32 (53.5) | 0.004 | 33 (89.2) | 73 (80.8) | 0.001 | 106 (67.5) |
| Lactate, 2-3.9 mmol/L, n (%) | 18 (18.2) | 14 (24.1) | 0.371 | 2 (5.4) | 30 (25.0) | 0.009 | 32 (20.4) |
| Lactate, >4 mmol/L, n (%) | 6 (6.1) | 13 (22.4) | 0.004 | 2 (5.4) | 17 (14.2) | 0.247 | 19 (12.1) |
| Any infection, n (%) | 68 (68.7) | 50 (87.7) | 0.006 | 23 (62.2) | 93 (79.5) | 0.033 | 116 (75.3) |
| Sepsis, n (%) | 27 (27.3) | 42 (72.4) | 0.000 | 6 (16.2) | 63 (52.5) | 0.000 | 69 (44.0) |
| Septic shock, n (%) | 8 (8.1) | 24 (41.4) | 0.000 | 2 (5.4) | 30 (25.0) | 0.009 | 32 (20.4) |
| SOFA 24h, mean±SD | 1.7±2.8 | 4.3±4.6 | 0.000 | 1.4±2.3 | 3.1±4.0 | 0.017 | 2.63±3.75 |
| Apache II, mean±SD | 10.4±5.0 | 12.9±6.1 | 0.023 | 9.5±4.6 | 12.0±5.8 | 0.057 | 11.5±5.6 |
| In-hospital mortality, n (%) | 8 (8.1) | 14 (24.1) | 0.005 | 4 (10.8) | 18 (15.0) | 0.600 | 22 (14.0) |
| Any admission, n (%) | 70 (70.7) | 50 (86.2) | 0.027 | 26 (70.3) | 94 (78.3) | 0.312 | 120 (76.4) |
| Admission to ICU, n (%) | 22 (22.7) | 33 (56.9) | 0.000 | 8 (21.6) | 47 (39.8) | 0.043 | 55 (35.5) |
| Admission to ward, n (%) | 49 (50.5) | 23 (39.7) | 0.190 | 19 (51.4) | 53 (44.9) | 0.493 | 72 (41.4) |
| Vasopressors, n (%) | 10 (10.1) | 22 (37.9) | 0.000 | 2 (5.4) | 30 (25.0) | 0.009 | 32 (20.4) |
| Renal replacement, n (%) | 4 (4.0) | 11 (19.0) | 0.004 | 1 (2.7) | 14 (11.7) | 0.196 | 15 (9.6) |
| Mechanical ventilation, n (%) | 7 (7.1) | 17 (29.3) | 0.000 | 2 (5.4) | 22 (18.3) | 0.068 | 24 (15.3) |
Data are presented as median (interquartile range) or number (%) and compared with the Mann Whitney U test or the Fisher’s-exact test, respectively.
COPD: Chronic obstructive pulmonary disease; CKD: Chronic kidney disease; APACHE II: Acute physiology and chronic health evaluation II; ARDS: Acute respiratory distress syndrome; ICU: Intensive care unit
For the treatment, vasopressor agents were administered in 32/157(20.4%) patients, mechanical ventilation was used in 29/157 (18.5%) patients and haemodialysis was required by 15/157 (9.9%) patients. A significantly larger number of patients required each of these three treatments in the positive-qSOFA group, as shown in [Table/Fig-2]. Of the total, 120/157 (76.4%) patients developed infection during their hospital stay, out of which 69/157 (46%) cases were sepsis; 32/157 (20.4%) patients developed septic shock. Twenty-two (14%) patients died during their stay in hospital; all the deaths occurred in the group that developed sepsis. The outcomes according to negative qSOFA (n=99) and positive qSOFA (n=58) groups were as follows: incidences of sepsis in the negative-versus positive-qSOFA groups 27/99 (27.3%) versus 42/58 (72.4%), p=0.000; incidences of in-hospital mortality were 8/99 (8.1%) versus 14/58 (24.1%) in the negative-versus positive qSOFA groups, respectively, p=0.005. In-hospital mortality for the qSOFA 0, 1, 2 and 3 groups were 5%, 10.2%, 14.3% and 39.1%, respectively.
Twenty-four hours after admission to ED, the mean SOFA score was 2.6±3.8, with 1.68±2.76 versus 4.3±4.6 in the negative-qSOFA versus positive-qSOFA groups, respectively, (p=0.000) and the mean APACHE II score was 11.5±5.6 with a significant difference between negative-versus positive-qSOFA groups with 10.4.0±5.0 versus 12.9±6.1, respectively, p=0.0117. Most frequent infection sources were respiratory system corresponding to 86/157 (54.8%), abdomen 21/157 (13.4%), urinary tract 19/157 (12.1%); and the most frequent germs were E. Coli in 11/157 (7.0%), H1N1 in 5/157 (3.2%), S. Agalactiae in 4/157 (2.5%) patients. Fifty-five (35%) patients were admitted to the intensive care unit, there was a significant difference between negative- and positive-qSOFA groups: 22/99 (22.7%) versus 33/58 (51.7%), respectively, p=0.011.
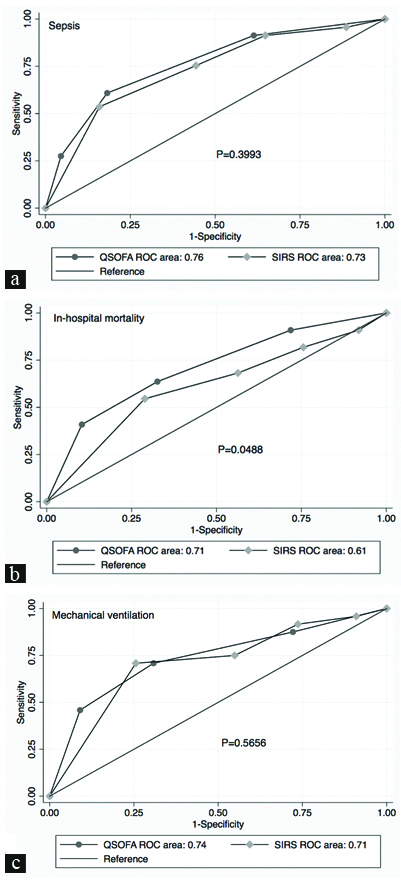
The discrimination of sepsis using qSOFA was comparable with the SIRS criteria (p=0.399) and the discrimination of in-hospital mortality using qSOFa was better than SIRS criteria (p=0.0488). For qSOFA, the AUC for predicting sepsis was 0.765 (95% CI 0.69-0.84); at the cut-off point of 2, sensitivity was 60.9% and specificity was 81.8% while the AUC for predicting in-hospital mortality was 0.71, (95% CI 0.59-0.83), cut-off point of 2 showed a sensitivity of 63.6% and a specificity of 67.4%. The SIRS criteria showed AUC of 0.74 (95% CI, 0.65-0.81) for predicting sepsis, at the cut-off point of 2, sensitivity was 91.3% and specificity was 35.2%; and the AUC for predicting in-hospital mortality was 0.61% (95% CI 0.48-0.74) with cut-off point of 2, sensitivity of 81.8% and specificity of 24.4%. For the prediction of sepsis in patients ≥65 years of age (n=86), qSOFA cut-off point of 2 had an AUC of 0.71, (95% CI 0.61-0.80) and in patients with immunosuppression (n=76), AUC was 0.77 (95% CI 0.68-0.86) not statistically different from AUCs of SIRS for the same subpopulations, AUC 0.66, (95% CI 0.57-0.74), and AUC 0.69, (95% CI 0.60-0.78), p=0.39 and p=0.17, respectively. For the prediction of in-hospital mortality, in patients ≥65 years of age, qSOFA had an AUC of 0.61, (95% CI 0.46-0.76) and in patients with immunosuppression, AUC was 0.62, (95% CI 0.49-0.76), not statistically different from AUCs of SIRS for the same subpopulations, AUC 0.54, (95% CI 0.43-0.66), and AUC 0.54, (95% CI 0.43-0.65), p=0.33 and p=0.21, respectively. The AUCs for qSOFA versus SIRS for predicting mechanical ventilation assistance were: 0.74 (95% CI 0.62-0.86) versus 0.71 (95% CI 0.60-0.83), respectively, p=0.5656; at the cut-off point of 2, qSOFA sensitivity and specificity were 70.83% and 69.2%, respectively whereas SIRS presented sensitivity of 91.67% and specificity of 26.3%. [Table/Fig-2] shows the details of both scores at a cut-off point of two and [Table/Fig-3] represents AUCs.
Comparison of test characteristics and discriminatory performance for qSOFA and SIRS.
| Score | Outcomes | Cut-off | Sens% | Speci% | PPV | NPV | LR+ | LR- | ROC area | 95%CI |
|---|
| qSOFA | Sepsis | 2 | 60.87 | 81.82 | 72.41 | 72.73 | 3.35 | 0.48 | 0.71 | 0.64-0.78 |
| qSOFA | Mortality | 2 | 63.64 | 67.41 | 24.14 | 91.92 | 1.95 | 0.54 | 0.65 | 0.54-0.76 |
| qSOFA | Ventilation | 2 | 70.83 | 69.17 | 29.31 | 92.93 | 2.30 | 0.42 | 0.70 | 0.60-0.80 |
| SIRS | Sepsis | 2 | 91.3 | 35.23 | 52.50 | 83.78 | 1.41 | 0.25 | 0.63 | 0.57-0.69 |
| SIRS | Mortality | 2 | 81.82 | 24.44 | 15.0 | 89.00 | 1.08 | 0.74 | 0.53 | 0.44-0.62 |
| SIRS | Mortality | 2 | 81.82 | 24.44 | 15.0 | 89.00 | 1.08 | 0.74 | 0.53 | 0.44-0.62 |
| SIRS | Ventilation | 2 | 91.67 | 26.32 | 18.33 | 94.59 | 1.24 | 0.32 | 0.59 | 0.52-0.66 |
PPV: Positive predictive value; NPV: Negative predictive value; AUROC: Area under the receiver operating characteristic curve; SIRS: Systemic inflammatory response syndrome criteria; qSOFA: Quick sequential [sepsis-related] organ failure assessment score; LR+: Positive likelihood ratio; LR-: Negative likelihood ratio; CI: Confidence interval
Comparison of the area under the receiver operating characteristic curves (AUC) of qSOFA and SIRS criteria.
aAUC comparison for the prediction of sepsis
bAUC comparison for the prediction of in-hospital death
cAUC comparison for the prediction of mechanical ventilation
Discussion
It was found that qSOFA showed an accuracy comparable to SIRS for predicting sepsis and superior accuracy for predicting in-hospital death. In 2016, a new definition of sepsis was proposed, specifying it is a life-threatening organ dysfunction caused by a dysregulated host response to infection [4,8,14,15]. Potential criteria for organ dysfunction required parameters that may be difficult to obtain and increase workload for clinicians whereas a simple model such as qSOFA, with 3 clinical variables and no laboratory tests, offered a predictive validity outside of the ICU that is statistically greater than SOFA [9]. Studies of qSOFA in Latin America are scarce, although interest on this score everywhere else is growing.
The high specificity of qSOFA to predict sepsis could contribute to improve the screening efficiency of patients with suspected infection who would develop a life-threatening organ dysfunction, allowing them to be assessed further for any clinical conditions, early interventions or transfer to ICU [11]. In a study of community-acquired sepsis encounters, an association between delay from first medical contact to antibiotic administration and in-hospital mortality was observed; moreover, the association of greater delay with increased risk-adjusted in-hospital mortality was robust to confounders [16,17]. It has been found that the risk of progression from severe sepsis to septic shock increased by 8% for each hour that passed between admission and antimicrobial administration [18]. The explanations proposed include a prompt treatment with antibiotics that help in reducing pathogen burden, modifies the host response, possibly reduces the incidence of the consequent organ dysfunction; professionals who quickly measure the serum lactate level may also recognise shock and could deliver lactate-guided resuscitation unlike those who are slower to measure this variable [16].
SOFA, qSOFA, SIRS, and LODS were assessed outside ICU setting and the results showed qSOFA was statistically superior to SOFA and SIRS in predicting in-hospital mortality [4]. qSOFA predicted ICU admission similarl to SOFA and APACHE II but slightly worse than MEDS [19]. In the ED, qSOFA was superior to SIRS in predicting organ failure along with in-hospital mortality rate [20]. In an international prospective study, qSOFA showed a better discriminative value and hazard ratio for predicting death, admission to ICU and ICU stay than SIRS [12]. The qSOFA score was also found to be more accurate than SIRS for predicting in-hospital mortality and ICU-free days, but showed worse predicting capacity for ventilator-free days and any organ dysfunction-free days [21]. Recently, Singer AJ et al., found an association between qSOFA scores and mortality, admission and length of hospital stay; interestingly, qSOFA performed equally well in patients both with and without a suspected infection, which suggested that it serves as a generic tool to predict clinically important outcomes for ED patients regardless of suspected infection [22]. Conversely, a small number of studies showed a poor performance of qSOFA as a screening tool for the early identification of sepsis in ED, and the authors suggested that the severity of illness represented by the qSOFA components may not be present in the early phases of the disease process [23,24]. The point of objection was qSOFA could vary rapidly and patients admitted to ED were not generally met by sepsis experts [24]. When compared with Modified Early Warning Score (MEWS) and the National Early Warning Score (NEWS) for predicting in-hospital mortality and ICU admission, qSOFA was less accurate, but more accurate than SIRS [25].
The main advantages of qSOFA are that it is simple to use and does not depend on laboratory results [22]. Importantly, clinical judgement must always be pre-eminent. No scoring system can be a stand-alone definition of sepsis [26]. In large prospective study, qSOFA showed sensitivity of 0.32 and specificity of 0.98 for the identification of severe sepsis [24]. In the largest cohort to date, qSOFA ≥2 was highly specific for Sepsis-3 organ dysfunction and mortality but sensitivity was poor compared to sensitivity for SIRS≥2 [27]. It has been argued that a cut-off ≥2 qSOFA showed a poor sensitivity despite being highly specific, especially in older patients [27,28]. When evaluating triage in the ED, the sensitivity of qSOFA to predict critical care interventions was very low; the authors argued that the score should be calibrated to an actionable endpoint [29]. In our study, no comparable variable was used; however, qSOFA equal or greater than 2 showed a sensitivity of 70.8% in the prediction of mechanical ventilation.
Limitation
This was a single-centre study, with a small sample size and a limited number of variables. In addition to that, patients discharged were not followed up, as in-hospital mortality was the primary focus. Different measurements of the score within the proposed time frame could not be compared because of limited resources.
Conclusion
The findings suggest that the newly introduced qSOFA provides better discrimination than SIRS for predicting in-hospital mortality and comparable discrimination for predicting sepsis in patients admitted to the ED with suspected infection. This and other studies may help physicians confirm the appropriate use of this simple tool in the ED setting.
Data are presented as median (interquartile range) or number (%) and compared with the Mann Whitney U test or the Fisher’s-exact test, respectively.
COPD: Chronic obstructive pulmonary disease; CKD: Chronic kidney disease; APACHE II: Acute physiology and chronic health evaluation II; ARDS: Acute respiratory distress syndrome; ICU: Intensive care unit
PPV: Positive predictive value; NPV: Negative predictive value; AUROC: Area under the receiver operating characteristic curve; SIRS: Systemic inflammatory response syndrome criteria; qSOFA: Quick sequential [sepsis-related] organ failure assessment score; LR+: Positive likelihood ratio; LR-: Negative likelihood ratio; CI: Confidence interval