Septic Arthritis of Shoulder Joint an Unusual Complication of Acute Cholangitis
Sudhir Maharshi1, Shyam Sunder Sharma2, Vaibhav Jain3, Bharat Sapra4
1 Assistant Professor, Department of Gastroenterology, SMS Medical College and Hospitals, Jaipur, Rajasthan, India.
2 Senior Professor, Department of Gastroenterology, SMS Medical College and Hospitals, Jaipur, Rajasthan, India.
3 Consultant, Department of Orthopaedics, Rukmani Birla Hospital, Jaipur, Rajasthan, India.
4 Senior Professor, Department of Gastroenterology, SMS Medical College and Hospitals, Jaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sudhir Maharshi, Assistant Professor, Department of Gastroenterology, SMS Hospital, Jaipur-302004, Rajasthan, India.
E-mail: sudhir.maharshi@gmail.com
Acute cholangitis manifest as jaundice, abdominal pain and fever. Patients of severe acute cholangitis may develop septic shock, altered sensorium and later may progress to multiorgan failure. Septic arthritis of shoulder joint usually develops due to septicaemia, direct inoculation or because of direct spread of infection from adjacent tissue. There is no reported case of septic arthritis of shoulder joint, secondary to acute cholangitis in literature. Herein, we are reporting a first of its kind case of septic arthritis of left shoulder joint secondary to complication of acute cholangitis, which was managed successfully with antibiotics and arthroscopic debridement.
Choledocholithiasis, Jaundice, Sepsis
Case Report
A 45-year-old woman admitted in Department of gastroenterology with pain in right upper quadrant, fever and jaundice from last 10 days along with decreased urine output and altered sensorium since two days. She was treated with intravenous ceftriaxone 1 gm twice daily for three days in primary health centre, however in view of worsening her general condition, was referred to the hospital. She underwent cholecystectomy for symptomatic gallstones five years back. There was no history of diabetes mellitus, systemic hypertension, coronary artery disease, pulmonary tuberculosis in past. She was a house wife, non smoker and non alcoholic. On physical examination she was febrile, drowsy, talking irrelevantly, pale and had jaundice. Her blood pressure was 80/60 mmHg with pulse rate of 110 per minute. Abdominal examination revealed mild right hypochondrium tenderness without any palpable mass or lump. Laboratory investigations showed White Blood Counts (WBCs) 16300 cells/mm3 with 94% polymorphs, platelets 52000 cells/mm3, ESR 72 mm/hour, haemoglobin 8.9 gm/dL, serum bilirubin 6.8 mg/dL, Aspartate Amino Transferase (AST) 96 IU/L, Alanine Aminotransferase (ALT) 120 IU/L, Alkaline Phosphatase (ALP) 296 IU/L, blood urea 60 mg/dL, and creatinine was 1.92 mg/dL. Abdominal ultrasound showed dilated (15 mm) Common Bile Duct (CBD) and bilateral Intrahepatic Biliary Radicles (IHBR) with a large stone (12 mm) in it. On the basis of history, physical examination and laboratory investigations she was diagnosed to have acute severe cholangitis and started on intravenous antibiotics (Ceftazidime 2 gm thrice daily), inotropic support (noradrenaline) and other supportive treatment. In view of acute severe cholangitis, urgent Endoscopic Retrograde Cholangio Pancreatography (ERCP) was done. Selective CBD cannulation was done, 5 mL bile was aspirated for culture. Cholangiogram showed dilated (15 mm) CBD and IHBR with large (12 mm) filling defect in CBD. Endoscopic papillotomy was done, followed by a 10fr×10 cm double pigtail plastic stent placed in CBD, draining purulent bile [Table/Fig-1]. Stone removal was planned after clinical stabilisation of the patient. Gradually she improved, was off inotropic support and afebrile on day 3. Her serum bilirubin and WBC count were 2.6 mg/dL and 12,100 cell/mm3 respectively on the same day. Bile and blood culture grown Pseudomonas aeruginosa was sensitive to ceftazidime, the antibiotics which she was already on. Presence of Pseudomonas aeruginosa in both bile and blood culture may be because she was hospitalised initially at primary health centre and received intravenous antibiotics, as discussed earlier. She was discharged on day 14 in stable state with a plan of stone removal after four weeks. Three weeks later she came with pain in left shoulder joint along with restriction of movements. Orthopaedic examination showed mild swelling of left shoulder joint along with restriction of all movements. Laboratory investigations revealed WBC 15300 cells/mm3 with polymorphs 90%, platelets 1.4 lacs cells/mm3, ESR 65 mm/hour and normal liver function tests. X-ray of left shoulder joint showed increased joint space and Magnetic Resonance Imaging (MRI) of same joint showed oedema, debris along with heterogeneous signals in the joint [Table/Fig-2]. Synovial fluid from same joint was hazy and had WBC 16000/mL with 95% polymorph, total protein 6.7 gm/dL and glucose 21 mg/dL. Gram staining showed numerous pus cells along with gram negative coccobacilli suggestive of septic arthritis. She was started on intravenous antibiotics (meropenem 1 gm thrice daily) and taken for arthroscopic debridement under general anaesthesia with two portal techniques. Pus was drained and saline wash of the joint was commenced. There was partial rotator cuff tear, left as such because of extensive infection. Synovial fluid culture isolated Pseudomonas aeruginosa which was sensitive to meropenem. Antibiotics continued for the next four weeks along with other supportive treatment. After four weeks she underwent repeat ERCP and the large CBD stone was removed. Gradually her septic arthritis improved and on follow-up after two months her shoulder joint was pain free with minimal restriction of movements.
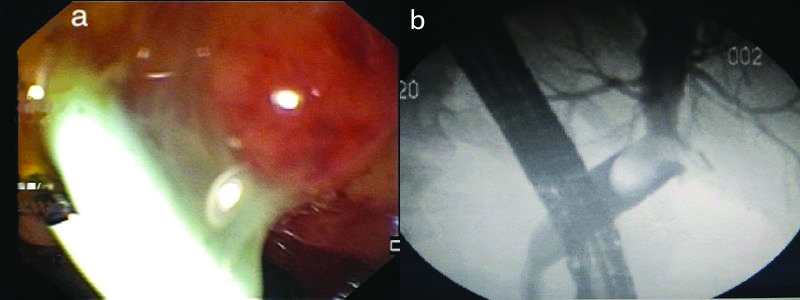
Endoscopic and fluoroscopic images of patient.
a) Side view endoscopic image showing 10 french double pigtail plastic stent in common bile duct draining purulent bile.
b) Fluroscopic image showing dilated (15 mm) common bile duct, large (12 mm) filling defect in it with bilateral dilated intrahepatic biliary radicles.
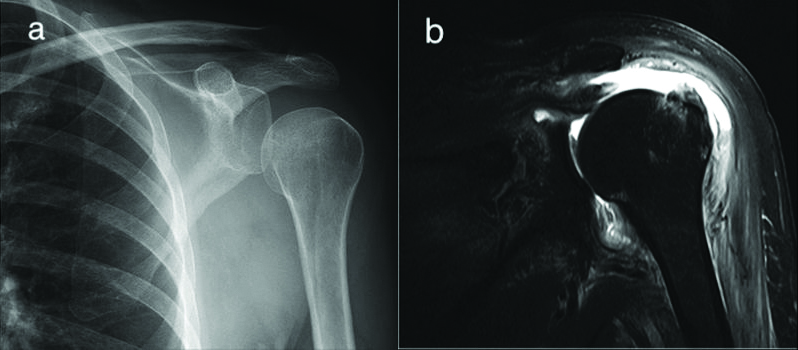
Radiological images of patient.
a) X-ray of left shoulder joint showing increased joint space; b) Magnetic resonance imaging short tau inversion recovery (STIR) coronal image of left shoulder joint showing oedema, debris along with heterogeneous signals in the joint.
Discussion
Acute cholangitis is a biliary tract infection associated with obstruction of biliary system, caused by various aetiologies like choledocholithiasis, bile duct stricture either benign or malignant, previously placed stent malfunction and bilioenteric anastomotic malfunction [1]. It progresses from local biliary infection to Systemic Inflammatory Response Syndrome (SIRS) and in advanced state it leads to sepsis with or without multiorgan failure [1,2]. Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection [3]. Septic shock is defined as a subset of sepsis in which underlying circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than sepsis alone. Organ dysfunction can be identified as an acute change in total Sequential Organ Failure Assessment (SOFA) score ≥2 points consequent to the infection [4]. Charcot described the clinical triad of fever, jaundice and abdominal pain as clinical manifestation of acute cholangitis, later Reynolds BM and Dragan EL, described severe acute cholangitis which included Charcot’s triad plus septic shock and altered mental status termed as Reynould’s pentad [5]. The incidence of Charcot’s triad and Reynould’s pentad varies from 15.4-72% and 3.5-7.7% respectively [6-8]. The patient had acute severe cholangitis with Reynould’s pentad and after three weeks she developed septic arthritis of left shoulder joint.
Acute cholangitis complicated by shoulder joint septic arthritis has not been documented in medical literature. Only one case report shows septic arthritis of hip joint secondary to acute cholangitis [9]. Other causes of septic arthritis of shoulder joint are septicaemia, local spread from adjacent osteomyelitis or soft tissue infection, direct inoculation due to trauma and after an orthopaedic procedure [10-12]. Septicaemia or hematogenous spread is one of the reported causes of septic arthritis, can be seen in patients with acute severe cholangitis [13]. Abnormal joint is the most common risk factor for septic arthritis, usually seen in patients with rheumatoid arthritis, osteoarthritis, crystal arthropathies and other inflammatory arthritis [14]. Staphylococcus aureus is the most common organism causing septic arthritis, however Gram negative organisms are cultured from up to 20% of patients with septic arthritis mostly in children, elderly, diabetics, and immunocompromised [15]. This patient developed septic arthritis of left shoulder joint because of septicaemia secondary to acute cholangitis. In a previous case report septic arthritis of hip joint secondary to cholangitis was also managed successfully with intravenous antibiotics and surgical treatment. The patient developed septic arthritis after the complete treatment of acute cholangitis, the finding is similar to this case report [9]. Clinical symptoms of acute cholangitis like jaundice, pain abdomen, fever, oliguria and altered sensorium has been described in various studies but septic arthritis is a rare manifestation [6-8]. Septic shock, altered mental status and multiorgan failure are more common with acute severe cholangitis [1].
Conclusion
Septic arthritis is an uncommon complication of acute cholangitis, but one should look for joint involvements in acute severe cholangitis. Early diagnosis and management of septic arthritis in such patients can prevent permanent joint damage and disability.
[1]. Wada K, Takada T, Kawarada Y, Nimura Y, Miura Y, Yoshida M, Diagnostic criteria and severity assessment of acute cholangitis: Tokyo GuidelinesJ Hepatobiliary Pancreat Surg 2007 14(1):52-58.10.1007/s00534-006-1156-717252297 [Google Scholar] [CrossRef] [PubMed]
[2]. Lipsett PA, Pitt HA, Acute cholangitisSurg Clin North Am 1990 70:1297-312.10.1016/S0039-6109(16)45285-0 [Google Scholar] [CrossRef]
[3]. Hari MS, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)JAMA 2016 315(8):775-87.10.1001/jama.2016.028926903336 [Google Scholar] [CrossRef] [PubMed]
[4]. Singer M, Deutschman CS, Seymour CW, Hari MS, Annane D, Bauer M, The third international concensus definitions for sepsis and septic shock (Septis- 3)JAMA 2016 315(8):801-10.10.1001/jama.2016.028726903338 [Google Scholar] [CrossRef] [PubMed]
[5]. Reynolds BM, Dragan EL, Acute obsructive cholangitis: A distinct syndromeAnn Surg 1959 150:299-303.10.1097/00000658-195908000-0001313670595 [Google Scholar] [CrossRef] [PubMed]
[6]. Lai EC, Tam PC, Paterson IA, Ng MM, Fan ST, Choi TK, Emergency surgery for severe acute cholangitis: The high risk patientsAnn Surg 1990 211:55-59.10.1097/00000658-199001000-000092294844 [Google Scholar] [CrossRef] [PubMed]
[7]. Chijiiwa K, Kozaki N, Naito T, Kameoka N, Tanaka M, Treatment of choice for choledocholithiasis in patients with acute obstructive suppurative cholangitis and liver cirrhosisAm J Surg 1995 170:356-60.10.1016/S0002-9610(99)80303-1 [Google Scholar] [CrossRef]
[8]. Csendes A, Diaz JC, Burdiles P, Maluenda F, Morales E, Risk factors and classification of acute suppurative cholangitisBr J Surg 1992 79:655-58.10.1002/bjs.18007907201643478 [Google Scholar] [CrossRef] [PubMed]
[9]. Liu HC, Su YS, Fu TF, Hsieh MC, Septic arthritis of the hip secondary to acute cholangitis: A case reportJ Trauma 2005 58:398-400.10.1097/01.TA.0000064451.80581.6515706212 [Google Scholar] [CrossRef] [PubMed]
[10]. Cherney DL, Amstutz HC, Total hip replacement in the previously septic hipJ Bone Joint Surg Am 1983 65:126510.2106/00004623-198365090-00006 [Google Scholar] [CrossRef]
[11]. Gamble JG, Rinsky LA, Bleck EE, Acetabular osteomyelitis in childrenClin Orthop 1984 186:71-80.10.1097/00003086-198406000-00012 [Google Scholar] [CrossRef]
[12]. DeBoeck H, Haentjens P, Verhaven E, Osteomyelitis of the acetabulamActa Orthop Belg 1990 56:621-24. [Google Scholar]
[13]. Resnik CS, Amman AM, Walsh JW, Chronic septic arthritis of the adult hip: computer tomographic featuresSkeletal Radiol 1987 16:513-16.10.1007/BF003512643423819 [Google Scholar] [CrossRef] [PubMed]
[14]. Sharff KA, Richards EP, Townes JM, Clinical management of septic arthritisCurr Rheumatol Rep 2013 15:33210.1007/s11926-013-0332-423591823 [Google Scholar] [CrossRef] [PubMed]
[15]. Arias MG, Balsa A, Mola EM, Septic arthritisBest Practice & Research Clinical Rheumatology 2011 25:407-21.10.1016/j.berh.2011.02.00122100289 [Google Scholar] [CrossRef] [PubMed]