Intraoperative Rupture of Hydatid Cyst Membrane: A Flexible Rhino-laryngoscope Innovation to the Rescue
Nishant Sahay1, Umesh Kumar Bhadani2, Poonam Kumari3
1 Assistant Professor, Department of Anaesthesiology, All India Institute of Medical Sciences, Patna, India.
2 Professor and Head, Department of Anaesthesiology, All India Institute of Medical Sciences, Patna, India.
3 Senior Resident, Department of Anaesthesiology, All India Institute of Medical Sciences, Patna, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nishant Sahay, House No. 112, Type 4 Block 1, AIIMS Residential Complex, Khagaul-801105, Patna, India.
E-mail: nishantsahay@gmail.com
The present case report describes a catastrophe avoided during operative removal of hydatid cyst located in the lower lobe of left lung. The intrabronchial hydatid cyst membranes ruptured intraoperatively and were aspirated in the bronchi. The aspiration caused collapse of left upper lobe of lung. In the absence of flexible fibre optic or rigid bronchoscope for airway management, this potentially dangerous condition was diagnosed and successfully managed innovatively using a rhino-laryngoscope. An improvised arrangement using a paediatric suction catheter with its distal end cut and secured by adhesive paper to a rhino-laryngo fibrescope was made. This arrangement of suction catheter attached to a rhino-pharyngo-laryngoscope was then used to remove more than four pieces of membranes of hydatid cyst under direct vision from the tracheobronchial tree preventing an airway catastrophe. The case report thus highlights importance of quick thinking and effective resource management even in resource limited settings.
Airway management, Bronchoscopy complication, Echinococcus
Case Report
A 45-year-old male (body weight 50 kg) with hydatid cysts in the liver as well as left lung was admitted to the hospital. Surgeons planned to remove both lung and liver hydatid cysts in single sitting and patient was prepared for surgery. General anaesthesia was planned with isolation of lungs using a Double Lumen Tube (DLT). General anaesthesia was induced using Inj. Fentanyl 150 μg, Inj. Propofol 100 mg, and Inj. Vecuronium 5 mg. Trachea was intubated with DLT of 37 Fr size Mallinckrodt DLT tube. Confirmation of placement was done using auscultation method. Removal of left lung hydatid cyst was planned prior to removal of liver hydatid cyst. One lung ventilation was initiated in the right decubitus position and surgeons proceeded to remove the hydatid cyst from the left lung. During removal however they encountered bleeding and a request was made to expand the lung. It was now noted that the left upper lobe of lung was not expanding. At this time there was equipment malfunction of fibreoptic bronchoscope. In absence of a fibreoptic bronchoscope and contemplating a distal shift of the DLT, we repositioned the DLT pulling it proximally very gradually keeping the upper lobe under direct vision. The upper lobe could not be expanded. After application of Positive End Expiratory Pressure (PEEP) and proximal repositioning of the DLT by over 3 cm, suddenly the left upper lobe began to expand. However, by now then the authors started encountering increased airway resistance and there was a fall in the saturation to 86-90% with FiO2 of 1.0. We encountered severe ventilation difficulty even when both lung ventilation was attempted.
Procedure on the thorax was soon completed and the surgeons proceeded to operate on the liver. An ABG report was received by us by this time with a PaO2 58 mmHg and PaCO2 55 mmHg. In view of the unacceptably high airway pressures, low saturataion, low PaO2 and high PaCO2 we decided to replace the DLT with a single lumen tube. The rhino-laryngoscope was used to assess the airway. At 30 cm length, on shortening the endotracheal tube length, carina and beyond can be visualised.
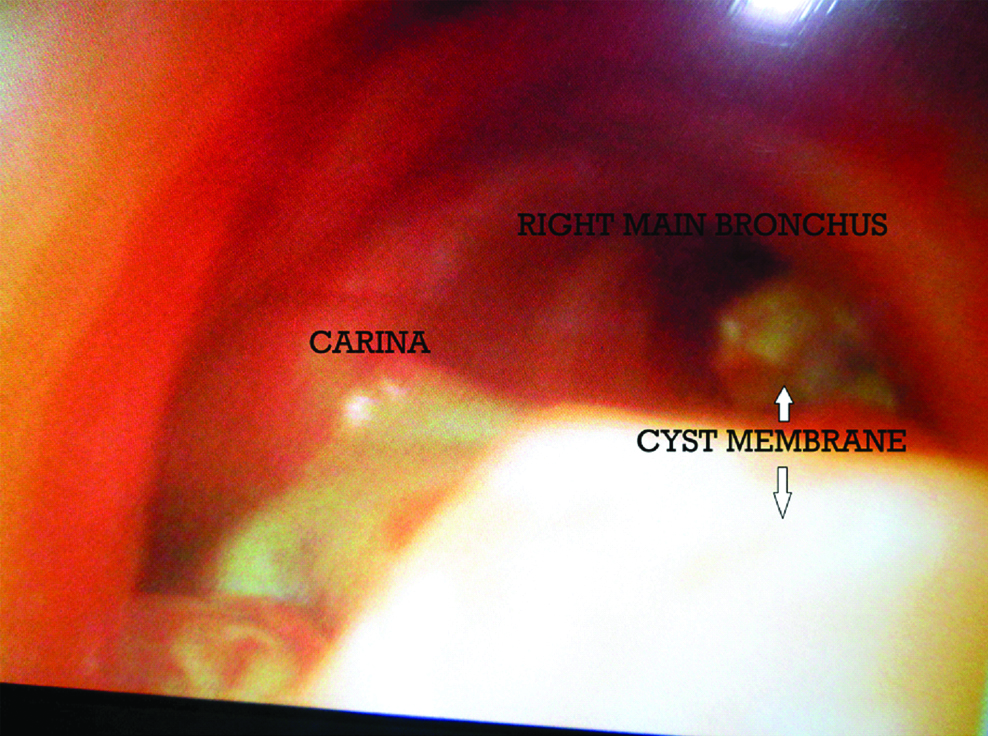
Immediately on introduction of the scope, whitish membranous structure was seen to be present in both left and right main bronchus as shown in [Table/Fig-1]. It was imperative for the authors to remove these membranes. The Karl Storz CMOS Otorhino-laryngo fibrescope has no suction port in the laryngoscope. Independantly used, a suction catheter cannot be manipulated satisfactorily thus, it was decided to secure a small gauge suction catheter with the laryngoscope so that it may be manipulated under vision.
Appearance of the ruptured hydatid cysts lying in the trachea around the carina.
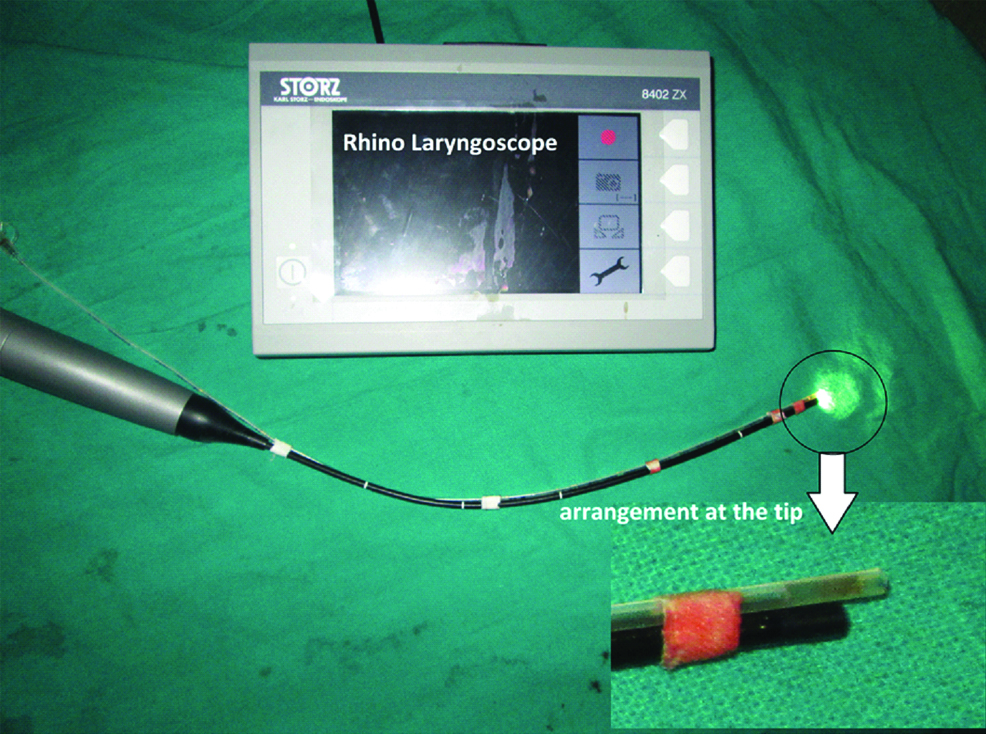
Suction catheter of Fr gauze 10 (500 mm and 3.30 mm diameter) had its terminal end cut such that the single opening was distal, rather than on the side of the catheter. It was secured in such a way that this distal end was slightly more protruded and consequently always under vision of the laryngoscope [Table/Fig-2]. This arrangement was introduced gradually through a catheter mount which enabled us to oxygenate and even gently ventilate at all times.
Suction catheter secured with a rhino-pharyngo-laryngoscope. Note the slight projection of cut end of suction catheter beyond the tip of the scope.
The arrangement was introduced up to the entrance of left main bronchus and kept near the membrane. Other end of the catheter was connected to gentle suction. The hydatid membrane got attached to suction catheter and this membrane attached to suction catheter was pulled gently up under vision into the endotracheal tube and subsequently removed outside.
Similarly membranes from right main bronchus were also removed. The endotracheal tube was disconnected from the anaesthesia machine intermittently. One by one four pieces of membranes were removed. Second membrane piece was a large one and once it was brought into the endo tracheal tube it was sucked out blindly by larger lumen suction catheter. The airway pressures and oxygenation improved significantly. Removal of liver hydatid cyst was accomplished uneventfully as sequenced in [Table/Fig-3]. Patient was reversed with Inj. neostigmine 2.5 mg and glycopyrrolate 0.6 mg, trachea was extubated and patient was shifted to recovery room. In recovery room patient coughed out one small remnant of membrane. Postoperative recovery was smooth and patient was followed for a week for any untoward side-effects.
Removal of the membranes from trachea bronchial tree.

Discussion
Hydatid disease is endemic in many parts of the world. Infestation by hydatid disease in humans most commonly occurs in the liver (55-70%) followed by the lung (18-35%); the two organs can be affected simultaneously in about 5-13% of cases [1-3]. During operative removal of the cyst any rupture during surgery may have variable outcomes. It can cause anaphylaxis during surgery [2,4,5]. Cyst membrane can get dislodged and may get aspirated into bronchi [1].
Patient of present case report had concomitant liver and lung hydatid cysts. In patients undergoing surgical excision of pulmonary hydatid cyst, the healthy lung must be isolated in order to protect it against transbronchial spread of hydatid fluid should inadvertent rupture of the cyst occur during its dissection and exposure. In the present case report, DLT was used to isolate lung during operation. The removal of cyst was done but membrane of hydatid cyst got detached and aspirated in ipsilateral upper left lobe bronchus.
In absence of fibreoptic bronchoscope accurate assessment of position as well as accurate repositioning of DLT was not possible and during the blind repositioning, it is anticipated that the isolation of two lungs was lost. It is also now contemplated that at this time the DLT may still be well positioned and the collapse of the left upper lobe of lung was due to the dislodged membrane itself. The application of positive pressure ventilation caused a dislodgement and possible contralateral spread of membranes to the right lung once the isolation was lost in this case resulting in a fall in oxygen saturation, PaO2 and rise in PaCO2 and airway pressures. Only once the DLT was exchanged to single lumen tube could the rhino-laryngoscope come into use and the condition was diagnosed.
Intraoperative aspiration of hydatid cyst material was seen in seven cases by Saidi F and Rezvan-Nobahar M, which were removed by bronchotomy and suction [1]. In the present case report, the condition was diagnosed intraoperatively however need of brochotomy was avoided due to timely diagnosis and retrieval of membranes using the innovation described earlier.
Anaesthesia is of vital importance in surgical removal of complicated hydatid cysts and particularly ruptured cysts. Spillage of laminated membrane could probably occur at any stage of anaesthesia including induction, maintenance, positioning and positive pressure ventilation, causing airway obstruction and further hypoxemia and asphyxia [6].
Conclusion
Otorhino-laryngo fibrescope is usually a diagnostic gadget, however in an emergency, utilising this tool proved to be life saving in this case.
[1]. Saidi F, Rezvan-Nobahar M, Intraoperative bronchial aspiration of ruptured pulmonary hydatid cystsAnn Thorac Surg 1990 50(4):631-36.10.1016/0003-4975(90)90203-I [Google Scholar] [CrossRef]
[2]. Marashi S, Hosseini VS, Saliminia A, Yaghooti A, Anaphylactic shock during pulmonary hydatid cyst surgeryAnaesth Pain Med 2014 4(3):e1672510.5812/aapm.16725 [Google Scholar] [CrossRef]
[3]. Safioleas M, Misiakos EP, Dosios T, Manti C, Lambrou P, Skalkeas G, Surgical treatment for lung hydatid diseaseWorld J Surg 1999 23(11):1181-85.10.1007/s00268990064310501882 [Google Scholar] [CrossRef] [PubMed]
[4]. Bensghir M, Fjouji S, Bouhabba N, Ahtil R, Traore A, Azendour H, Anaphylactic shock during hydatid cyst surgerySaudi J Anaesth 2012 6:161-64.10.4103/1658-354X.9703122754444 [Google Scholar] [CrossRef] [PubMed]
[5]. Kermenli T, Yalçınöz K, Polat ME, Intrathoracic multiple recurrence and bilateral endobronchial rupture of cyst hydatid disease; the rare cause of anaphylaxisRespir Med Case Rep 2017 21:113-15.10.1016/j.rmcr.2017.04.00228458996 [Google Scholar] [CrossRef] [PubMed]
[6]. Pirmoazen N, Saidi F, Ahmadi ZH, Firouzi F, The surgical management of complicated pulmonary hydatid cystsMed J Islamic Republic of Iran 2004 18(1):01-05. [Google Scholar]