Although more surgeons are now convinced of the superiority of open reduction and internal fixation (ORIF) in maximum number of cases, the management of condylar fracture of mandible is controversial in the field of maxillofacial trauma. The mandible anatomy is such that, it allows the dissipation of forces along the weakest part at the condylar neck, to fracture and thus prevents transfer of forces to the glenoid fossa of the cranium. This is the reason for the high prevalence of condylar fractures [1]. Such injuries are common and accounts for 25-35% of all mandibular fractures [2,3].
There are various treatment options for subcondylar fracture. Whether to go for a Conservative or Surgical treatment mostly depends on the patient opinion. When it comes to surgical treatment, open reduction and internal fixation is done using various plating technique like use of single plate or double miniplate. The fixation of a single four or six hole miniplates vertically on the posterior border of the condylar neck remains the most common technique. However, Hammer B et al., has reported proof of high failure rate with this technique (up to 35%), including plate fracture, structural instability and screw loosening [4]. The main reason for failure of this technique is that it does not comply with the principles of osteosynthesis regarding functional stability in the mandibular condylar area. Choi BH et al., have reported better results with the use of two miniplates in combination i.e. the first being placed parallel to the posterior border of condylar neck, the second being placed obliquely under the mandibular notch [5]. However, it is sometimes difficult to position 4 screws in the condylar fragment due to its small size and extensive surgical exposure and also increases the risk of facial nerve damage. This technique is almost impossible to use in the high subcondylar fractures.
Meyer C et al., described a new design for the condylar plate in 2007 which was trapezoidal in shape. Most of the required prerequisites for rigid fixation in subcondylar fractures was fulfilled by the trapezoidal shaped plate. The normal advantages of the 3-D plates is that it provides stability in three dimensions, provides resistance against torque while maintaining a low profile and malleability, allows for an increased number of screws. Most importantly these trapezoidal plates fits the strain pattern that occur in the condylar region during function [6].
Lauer G et al., used a delta-shaped plate in sub-condylar fractures and found that it adequately stabilized the condylar fragment [7]. Like trapezoidal plate it also allowed for sufficient neutralization of strains in the condylar and subcondylar region thereby providing sufficient stabilization for ORIF combined with its advantage of being a smaller plate.
The aim of this study was to test the stability of fracture fixation obtained with Trapezoidal plates and Delta plates by biomechanical means and to compare them with 2 miniplate fixation technique as described by Choi BH et al., [5]. The advantage of this study is that it is a biomechanical study, not carried out in any live animal or human being and so patient consent is not required [5].
Materials and Methods
This is a prospective biomechanical study which was carried out in ITS Center for Dental Studies and Research, Murad nagar (UP) India in Department of Oral and Maxillofacial Surgery from September 2014 to April 2016. Since it was not carried out in any form of live animal or human being, ethical clearance was not required. A total of 36 fresh porcine hemi- mandibles was used for the study. These fresh mandibles were obtained from butcher. From each mandible the soft tissue was stripped off by boiling the mandible in salt water. All the hemi mandibles were sectioned in the posterior molar region and osteotomized along a line 5 mm above and parallel to a tangent drawn along the posterior border of the coronoid process, using a hand jig saw and then fixed using either one of three techniques. The fractures was fixed with a Trapezoidal titanium plate (2 mm in diameter, orthomax), Delta plate (2 mm in diameter) and Mini plates (2 mm in diameter, Orthomax), using 5 mm and 8 mm screw (in length). 5 mm screws were used in the condylar neck and 8mm screw were used in condylar head region. A 1.5 mm twist drill was used for preparation of all the holes.
The 36 porcine hemi-mandibles were divided into three group (12 Porcine hemi mandible per group) was subjected to linear loading in four different directions using a universal testing machine. The direction of the force was Anterior to posterior, Posterior to anterior, Medial to lateral and Lateral to medial
Group A- Trapezoidal plates;
Group B- Delta plates;
Group C- Mini-plates;
Group A is further divided into 4 sub-groups having 3 hemi-mandible in each:
Group A1- lateral to medial loading;
Group A2- medial to lateral loading;
Group A3- anterior to posterior loading;
Group A4- posterior to anterior loading.
Group B is further divided into 4 sub-groups having 3 hemi-mandible in each:
Group B1- lateral to medial loading;
Group B2- medial to lateral loading;
Group B3- anterior to posterior loading;
Group B4- posterior to anterior loading.
Group C is further divided into 4 sub-groups having 3 hemi-mandible in each:
Group C1- lateral to medial loading;
Group C2- medial to lateral loading;
Group C3- anterior to posterior loading;
Group C4- posterior to anterior loading.
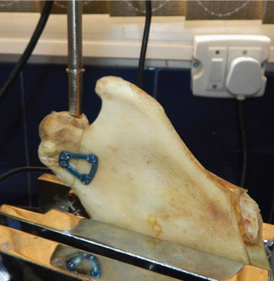
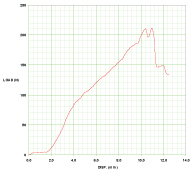
In the Universal Testing Machine of our institute Yield Load (YL) and Yield Displacement (YD) was measured for the plates. Yield load expressed in Newtons, is that load at which permanent deformation of the systems begins. Yield displacement expressed in millimeter is that displacement at which permanent deformation begins. Each sample was subjected to a linear loading at a rate of 10mm/min and the loading was continued to failure. Failure is defined as fracture of the plate or screws, loosening of the screws or displacement at the site of the fracture. [Table/Fig-1,2] shows the development of linear loading and linear displacement. The point at which failure occurs is recorded. That point is the maximum load, the plate can bear in that direction and the amount of displacement is recorded simultaneously.
A sample being tested in UTM.
A graph showing load vs displacement.
Statistical Analysis
The mean values of load and displacement of the three groups were compared by using the Kruskal-Wallis test and Mann-whitney U test with a confidence level of 95% (p < 0.05) using SPSS version 18.
Results
In the biomechanical study none of the plates were fractured. Screw loosening was seen in one case of delta plate and in 2 cases of miniplate. In posterior to anterior and from medial to lateral the trapezoidal plate tolerated the highest load [Table/Fig-3,4]. From anterior to posterior and lateral to medial the miniplate tolerated the maximum load [Table/Fig-5,6].
Posterior to anterior loading Data (Mean±Std. Deviation).
| N | Mean±Sth. Deviation | p-value |
|---|
| YL | A | 3 | 396.75 | ±177.40772 | 0.041* |
| B | 3 | 308.81 | ±56.57713 |
| C | 3 | 188.61 | ±21.94501 |
| YD | A | 3 | 9.1133 | ±2.99133 | 0.957 |
| B | 3 | 8.8167 | ±1.34972 |
| C | 3 | 7.7367 | ±4.81550 |
A: Trapezoidal plate; B: Delta plate; C: Miniplate
Medial to lateral loading Data (Mean±Std. Deviation).
| | N | Mean±Std. Deviation | p-value |
|---|
| YL | A | 3 | 707.10 | ±58.61824 | 0.027* |
| B | 3 | 53.9033 | ±6.32333 |
| C | 3 | 84.9900 | ±12.23696 |
| YD | A | 3 | 11.5393 | ±4.10160 | 0.046* |
| B | 3 | 6.6433 | ±2.33217 |
| C | 3 | 4.2067 | ±1.17462 |
A: Trapezoidal plate; B: Delta plate; C: Miniplate
Anterior to Posterior loading data (Mean±Std. Deviation).
| | N | Mean±Std. Deviation | p-value |
|---|
| YL | A | 3 | 137.26 | ±49.89947 | 0.039* |
| B | 3 | 210.84 | ±49.10627 |
| C | 3 | 282.30 | ±31.19981 |
| YD | A | 3 | 4.8000 | ±3.13809 | 0.491 |
| B | 3 | 6.9283 | ±.71387 |
| C | 3 | 8.1867 | ±3.68876 |
A:Trapezoidal plate; B:Delta plate; C:Miniplate
N-Sample Size
Lateral to medial loading Data (Mean±Std. Deviation).
| | N | Mean±Std. Deviation | p-value |
|---|
| YL | A | 3 | 177.17 | ±30.09082 | 0.027* |
| B | 3 | 108.26 | ±8.72734 |
| C | 3 | 430.48 | ±99.98922 |
| YD | A | 3 | 9.9533 | ±1.04270 | 0.561 |
| B | 3 | 8.9167 | ±10.29130 |
| C | 3 | 13.4133 | ±3.33661 |
Statically significant difference was seen in linear loading from all the direction. However, no statically significant difference was seen in linear displacement except from medial to lateral loading. Clinically it implies that there may be a difference in all the plates to bear the maximum linear load but displacement of the condyle will not occur in all the cases which is a good indication after ORIF.
Discussion
The concept of 3D square and rectangular plate was introduced by Farmand in 90s. Now-a-days advanced osteosynthesis plate has been developed like Trilock trauma condylar plate, Delta plate, Trapezoidal plate and most recently the “A” shaped plate [8], “Y” shaped plate for the sub condylar region. The Trilock trauma condylar plate is a 5-6 hole miniplate and needs to be evaluated both experimentally and clinically. The Delta plate as it name suggest is a delta-shaped miniplate with 4 hole having an upper arm and a base. The base of the delta is fixed on the ramus and the upper arm is fixed on to the condylar segment [7].
In this study the yield load and yield displacement of the three different designs of the plates was tested in four directions. The previous biomechanical studies by various authors (Choi BH et al., Asprino L et al.,) [5,9] used forces in two directions. Haug RH et al., applied forces in the same 4 directions and a rotational force [10]. Lauer G et al., applied forces in 4 directions [7].
In this experimental study it was found that 2-miniplate osteosynthesis with forces in the lateral-medial and anterior-posterior directions was the most stable [Table/Fig-5,6]. This was similar to the result obtained by Lauer G et al., [7]. Aspirno L et al., too found that 2-miniplate resist load better when subjected to anterior-posterior direction [9].
In our experimental study it was also find out that if the delta plate is placed properly, that is, if its lower border arm is placed within a distance of 7-8mm from the fracture line it avoids the rotation of the condylar head around its long axis. Lauer G et al., obtained a mean load of 315.63N, a mean displacement of 6.92mm for the delta plate [7]. The result of mean displacement of delta plate obtained by Lauer G et al., was similar to our study [7]. The application of the Delta plate for the stable osteosynthesis of condylar fractures ensures fully satisfactory treatment results, both from the radiological and the clinical points of view as stated by Sikora M et al., [11].
Trapezoidal shape allows location of the anterior arm over the ‘ideal’ osteosynthesis line. Therefore, the anterior arm acts as a tension bonding plate and the posterior arm which is placed along the axis of the condylar neck, remains free of bonding strains which happens to single conventional straight miniplates in the same position. The Trapezoidal plates fulfills the principles of functionally stable osteosynthesis, and benefits from the 3-D feature: improved stability, minimal soft tissue stripping. Two mono-cortical screws placed in the fractured condyle are sufficient [12]. In this study Trapezoidal plate performed better than the 2-miniplate osteosynthesis for forces in posterior-anterior and medial- lateral directions [Table/Fig-4,5]. The better result of the Trapezoidal plate compared to the delta plate may be because of its trapezoidal shape itself. Clinical application of 3D trapezoidal plate was also done by Chaudhary M et al., who stated that major reduction in posterior facial height, and deranged occlusion can be successfully managed by open reduction of condylar fracture and its fixation using Trapezoidal plates [13].
To compare biomechanical result of trapezoidal plate with other studies, we could not find any literature regarding the biomechanical study of trapezoidal plate where mean load and mean displacement has been mentioned.
Limitation
The main limitation of the study was it lacks co-relation with clinical application since it was only a biomechanical study. Further studies are required on patients having sub-condylar fractures in order to gauge their clinical efficacy.
Conclusion
The present study concluded that two 4-hole mini-plates when placed obliquely to the sigmoid notch and the other placed parallel to the posterior border tolerated the maximum load from lateral to medial and anterior to posterior direction. The Trapezoidal plate placed in the subcondylar region tolerated the maximum load from medial to lateral and posterior to anterior direction. Delta plate avoids rotation of the proximal segment in its long axis if its lower arm is placed within 7-8mm from the fracture line.
Based on the above findings it can be concluded that for sub-condylar fracture it is always a better option for the surgeons to select a 3D plate since its provides adequate stability. However, this study can be substantiated with its clinical applicability for all the 3 different plating modalities.
A: Trapezoidal plate; B: Delta plate; C: Miniplate
A: Trapezoidal plate; B: Delta plate; C: Miniplate
A:Trapezoidal plate; B:Delta plate; C:Miniplate
N-Sample Size