A Rare Combination of Genitourinary Vascular Anomaly
Rohini Arathala1, Vishwajit Ravindra Deshmukh2, S Nagaraj3, Hemanth Kommoru4, K Ariyanachi5
1 Tutor, Department of Anatomy, JIPMER, Karaikal, Puducherry, India.
2 Assistant Professor, Department of Anatomy, JIPMER, Karaikal, Puducherry, India.
3 Assistant Professor, Department of Anatomy, JIPMER, Karaikal, Puducherry, India.
4 Tutor, Department of Anatomy, JIPMER, Karaikal, Puducherry, India.
5 Senior Resident, Department of Anatomy, JIPMER, Karaikal, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vishwajit Ravindra Deshmukh, Ground floor, Department of Anatomy, JIPMER, Karaikal, Puducherry-609605, India.
E-mail: drvishwajitdeshmukh@gmail.com
Vascular anatomy of the genitourinary system is essential to understand the complications related to surgeries, as it may influence the blood flow to the kidney and to the gonads. In the present case report, arterial and venous variations were presented in the kidney. The inferior polar artery to the kidney was seen to arise from the aorta on the left side and the left testicular artery was one of the branches from the inferior polar artery. On the right side, duplication of renal veins was present and right gonadal vein was draining into the accessory renal vein, instead of inferior vena cava. Knowledge regarding such variations is of much use for the vascular surgeries in the retroperitoneal region and during the transplantation surgeries. Sometimes, these accessory arteries may compress renal pelvis, causing hydronephrosis.
Accessory renal artery, Gonadal vein, Renal Artery, Surgery
Case Report
During the routine dissection classes for the first year undergraduates, a rare uncommon variation in the genitourinary vasculature was observed in the male cadaver, aged 59 years in the department of anatomy. The cadaver had no pathological and traumatic lesions or marks of any surgical procedures in the anterior and posterior abdominal wall. Abdominal cavity was opened through the anterior approach as per the Guidelines of Cunningham’s manual for dissection, mesentery was identified and dissected followed by the removal of the small and large intestine to expose the retroperitoneal organs and the related vasculature [1]. The connective tissue surrounding the great vessels was cleared to identify the genitourinary blood vessels.
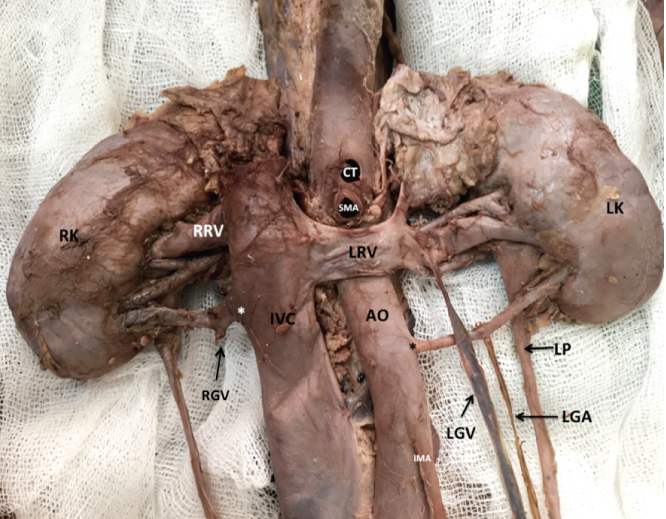
The following variations were observed in this cadaver: [Table/Fig-1a,b]. An accessory renal artery was seen to be arising from abdominal aorta at the level of L2 on the left side. It travelled anterior to the left pelvis and bifurcated before entering into the lower pole of left kidney. The accessory inferior polar artery was approximately 45 mm in length and 18.9 mm from the main renal artery. The left testicular artery arose from the left accessory renal artery whereas the right testicular artery was observed and had a normal pattern of origin from the abdominal aorta. Two aorta were accidentally not preserved during dissection. Two renal veins were draining from the right kidney: one from the hilum of right kidney and the other from inferior pole of the right kidney, which crossed anterior to the right pelvis. The accessory right renal polar vein, draining the inferior pole, was approximately 16 mm from the main renal vein. Both the veins were opening in the inferior vena cava. No such variations were found on the left side.
Photograph showing the variation in the genitourinary vasculature.
RRV: Right Renal Vein; LRV: Left Renal Vein; IVC: Inferior Vena Cava; RK: Right Kidney; LK: Left Kidney; AO: Aorta; CT: Coeliac Trunk; SMA: Superior Mesenteric Artery; IMA: Inferior Mesenteric Artery; LGV: Left Gonadal Vein; RGV: Right Gonadal Vein LGA: Left Gonadal Artery;
**: represents the abnormal origin of vessels
Schematic diagram showing the variation in the genitourinary vasculature.
RRV: Right Renal Vein; LRV: Left Renal Vein, RRA: Right Renal Artery, LRA: Left Renal Artery IVC: Inferior Vena Cava; RK: Right Kidney, LK: Left Kidney, AO: Aorta; LGV: Left Gonadal Vein; RGV: Right Gonadal Vein; LGA: Left Gonadal Artery; ARV: Accessory Renal Vein; LARA: Left Accessory Renal Artery; P: Pelvis, RSG: Right Suprarenal Gland; LSG: Left Suprarenal Gland
**: represents the abnormal origin of vessels
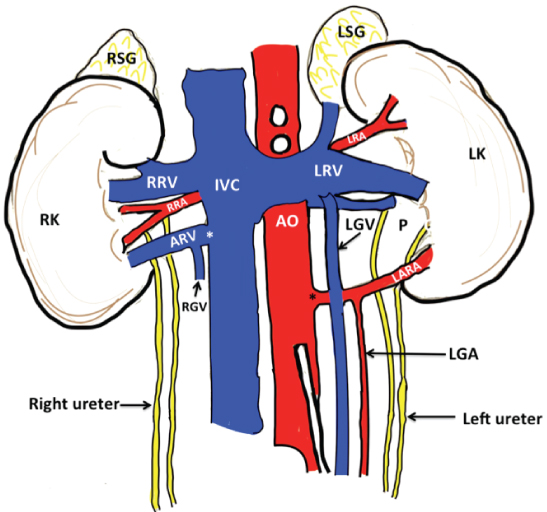
The right gonadal vein was draining into the right inferior polar vein, whereas, on the left side it had a normal pattern of termination into the left main renal vein. Due to dissection errors, only the stump of right gonadal vein was preserved, which is marked in [Table/Fig-1a,b]. On coronal section of left kidney, no sign of gross hydronephrosis was seen.
Discussion
Knowledge regarding genitorurinary development and vasculature is essential to understand the cause of multiple defects and variations related to it.
Variations in the renal arteries are twice more common than the renal veins. Normally, each kidney receives blood supply from the single renal artery. Kidneys receive 20% of the total cardiac output [2]. However, in 30% of the population, the accessory renal artery may be present, which might enter the kidney through hilum or through any pole especially inferior pole of the kidney termed as an accessory or polar arteries [3]. In such conditions, there is a possibility of obstruction for the outflow of the urine at the pelvic-ureteric junction, which may result in hydronephrosis. Aberrant renal arteries were first recorded by Eustachius in one of his famous plates, which remained unprinted in the Papal Library until 1714 [4].
The urogenital system is formed from the intermediate mesoderm. Both urinary and the genital system are intimately interwoven with each other developmentally as well as anatomically. The vascular anomalies of the kidneys can be associated with variations in the origin and course of gonadal vessels. The foetal metanephros is located at the vertebral level of S1-S2. From 6th to 9th week of intrauterine life, kidneys ascend to reach their adult position at T12-L3 [5]. During the ascent of the kidney, they receive blood supply from vessels at the corresponding vertebral level. When kidneys are located in the pelvis, the branches of internal iliac or common iliac arteries supply them. While the kidney ascends to the lumbar region gradually blood supply shifts from the common iliac arteries to the distal portion of the aorta. As the kidneys ascend, the caudal branches of aorta undergo involution and disappear. Then the kidneys receive the most cranial branches of the abdominal aorta, which in future becomes the permanent renal arteries [6]. According to Felix et al, nine lateral mesonephric arteries are divided into the cranial, middle and caudal group [5]. The middle group of lateral mesonephric arteries gives rise to the renal arteries. The caudal arteries usually persist and differentiate into the definite gonadal artery. Kadir S et al., reported that multiple renal arteries were unilateral in 30% of the patients and bilateral in approximately 10% [7]. One of the studies reported the presence of accessory renal artery in 4% out of the 50 cadaveric kidneys studied [8]. Another variation was seen in right kidney, which showed the presence of single accessory renal artery at the upper pole and double accessory renal artery at the lower pole [8]. Deshpande SH et al., observed three renal arteries on right and two on the left side [2]. The lower right is termed as the pre-caval right renal artery. The vessels entering the upper pole may arise either from the abdominal aorta or suprarenal artery, while those entering the lower pole may arise from the aorta, common iliac, internal iliac or superior mesenteric [9].
Some of the reports also mentioned about the venous variation in the renal vasculature such as three renal veins independently draining the right kidney and traversing up to the inferior vena cava [10]. Kidneys with aberrant vasculature are difficult cases for laparoscopic donor nephrectomy. Presence of accessory vessels will increase the duration of surgery and also risk in completing multiple vascular anastomoses.
Hazirolan T et al., reported the most common venous variant as the presence of supernumerary renal veins, which can be seen in approximately 15-30% of the individuals, and occasionally the accessory renal vein can drain into the iliac vein [11].
Various contrast studies were done to identify the sex differences in the gonadal vasculature. According to Bergman RA et al., there is no sex-related difference in the course and origin of gonadal arteries but the results of Cicekcibasi AE et al., showed that the gonadal artery variations were more commonly found in male than female [12,13].
Notkovich H found that in 14% of cases gonadal arteries were taking origin from the main renal artery or accessory renal artery [6]. Shoja MM et al., named this variation as an aberrant renal artery and hypothesised that aberrancies of the gonadal artery were a part of a common embryological error resulting in the persistence of future accessory renal artery [14]. In 5-6% cases, an aberrant gonadal artery originates from the main or accessory renal artery. There are various factors that may take part in the selection and persistence of a particular congenital vascular channel, like different environmental and chemical agents, genetic background, growth factors and haemodynamic forces. Sometimes, the formation of accessory blood vessels may be a sequence of hypoxia. Low oxygen saturation leads to the stabilisation of Hypoxia Inducible factor-1 (HIF-1) alpha, which causes up regulation of Vascular endothelial growth factor (VEGF), resulting in the formation of new blood vessels [15]. However, the embryonic reason for the persistence and formation of an accessory renal artery is unknown.
When aberrant gonadal artery represents the single blood supply to the gland it may become a major risk for some pathological conditions like varicocele or gonadal atrophy. The aberrant gonadal artery may be injured during various surgical procedures, hence increasing the risk during surgery. Hence, before performing any surgery for the genitourinary vasculature, arteriography or Doppler ultrasound examination should be done to avoid any complications related to the aberrant vasculature [16].
Conclusion
In the present case report, certain combinations of vasculature variations were observed. Such vascular variations were rare to find in one cadaver, even in the reports related to the genitourinary vasculature. The knowledge of such variations could be important to the vascular surgeons for grafting procedures and urologist and oncologist while performing surgery in the retroperitoneal region. If the presence of such anomalies were not recognised prior hand, it could prove hazardous during surgery. Knowledge and awareness of these possible variations and anomalies of renal arteries are important during renal transplantation, repair of abdominal aorta aneurysm, urological procedures and angiographic interventions.
[1]. Romanes GJ, Cunningham, smanual of practical anatomy, thorax and abdomen 1986 15th EditionOxford University Press:91:175 [Google Scholar]
[2]. Deshpande SH, Bannur BM, Patil BG, Bilateral multiple renal vessels: A case reportJournal of Clinical and Diagnostic Research: JCDR 2014 8(1):14410.7860/JCDR/2014/6893.380024596748 [Google Scholar] [CrossRef] [PubMed]
[3]. Standring S, Gray’s Anatomy: The Anatomical Basis of the Clinical Practice 2008 39th EditionEdinburgElsevier Churchill Livingstone:1231 [Google Scholar]
[4]. Eustachi B, Lancisi GM, Tabulaeanatomicaequasetenebrisvindicatas... apud R. et G. Wetstenios 1722 [Google Scholar]
[5]. Felix W, Mesonephricarteries. In: Keibel F, and Mall FP, edsMannual of Human Embryology 1912 Vol. 2PhiladelphiaLippincott:820-25. [Google Scholar]
[6]. Notkovich H, Variations of the testicular and ovarian arteries in relation to the renal pedicleSurgery, Gynecology & Obstetrics 1956 103(4):487 [Google Scholar]
[7]. Kadir S, Arteriography of the upper extremitiesDiagnostic angiography 1986 PhiladelphiaWB Saunders:172-206. [Google Scholar]
[8]. Hlaing KP, Das S, Sulaiman IM, Abd-Latiff A, Abd-Ghafar N, Suhaimi FH, Accessory renal vessels at the upper and lower pole of the kidney: a cadaveric study with clinical implicationsBratisl Lek Listy 2010 111(5):308-10. [Google Scholar]
[9]. Bordei P, Sapte E, Iliescu D, Double renal arteries originating from the aortaSurgical and Radiologic Anatomy 2004 26(6):474-79.10.1007/s00276-004-0272-915378279 [Google Scholar] [CrossRef] [PubMed]
[10]. Triple VR, Rara UV, Triple right renal vein: an uncommon variationInt J Morphol 2005 23(3):231-33.10.4067/S0717-95022005000300007 [Google Scholar] [CrossRef]
[11]. Hazirolan T, Öz M, Türkbey B, Karaosmanoglu AD, Oguz BS, Canyigit M, CT angiography of the renal arteries and veins: normal anatomy and variantsDiagnostic and Interventional Radiology 2011 17(1):67 [Google Scholar]
[12]. Bergman RA, Cassell MD, Sahinoglu K, Heidger PM Jr, Human doubled renal and testicular arteriesAnn Anatomy 1992 174:313-15.10.1016/S0940-9602(11)80292-X [Google Scholar] [CrossRef]
[13]. Çiçekcibasi AE, Salbacak A, Seker M, Ziylan T, Büyükmumcu M, Uysal II, The origin of gonadal arteries in human fetuses: anatomical variationsAnnals of Anatomy-Anatomischer Anzeiger 2002 184(3):275-79.10.1016/S0940-9602(02)80126-1 [Google Scholar] [CrossRef]
[14]. Shoja MM, Tubbs RS, Shakeri AB, Oakes WJ, Origins of the gonadal artery: embryologic implicationsClinical Anatomy 2007 20(4):428-32.10.1002/ca.2043817109441 [Google Scholar] [CrossRef] [PubMed]
[15]. Deshmukh V, Singh S, Sirohi N, Baruhee D, Variation in the obturator vasculature during routine anatomy dissection of a cadaverSultan Qaboos University Medical Journal 2016 16(3):e35610.18295/squmj.2016.16.03.01627606118 [Google Scholar] [CrossRef] [PubMed]
[16]. Petru B, Elena S, Dan I, Constantin D, The morphology and the surgical importance of the gonadal arteries originating from the renal arterySurgical and Radiologic Anatomy 2007 29(5):367-71.10.1007/s00276-007-0224-217593308 [Google Scholar] [CrossRef] [PubMed]