Internal Jugular Venous Ectasia in an Adult Female
Bharathguru Nedumaran1, Arunkumar Krishnasamy2
1 Associate Consultant, Department of Cardiothoracic Surgery, Billroth Hospitals, Shenoy Nagar, Chennai, Tamil Nadu, India.
2 Consultant, Department of Cardiothoracic Surgery, Billroth Hospitals, Shenoy Nagar, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bharathguru Nedumaran, Annai Illam, 44 Outer Circular Road, Kilpauk Garden Colony, Kilpauk, Chennai-600010, Tamil Nadu, India.
E-mail: bharathnedumaran@gmail.com
Jugular phlebectasia refers to a saccular or fusiform dilatation of the neck veins. Phlebectasia involving the jugular veins is an entity which is diagnosed more commonly in children presenting with neck swellings, after ruling out other common causes. It is also called a venous aneurysm, venous ectasia or essential venous dilatation. This can affect all neck veins-internal jugular, external jugular, anterior jugular and superficial communicating veins in order of decreasing frequency. Although, various theories have been proposed, there is no general consensus among various authors regarding the cause for its occurrence. It is predominantly congenital in origin. The diagnosis is based on clinical presentation aided by non-invasive imaging modalities. The venous ectasia is being increasingly recognised due to advances in radiographic imaging. Management is mainly conservative and surgery is required only when complications arise. Here, authors present a case of venous ectasia in an adult female who presented with complaints of the presence of a vague swelling in her neck.
Cervical swelling, Internal jugular vein, Phlebectasia, Venous aneurysm
Case Report
A 39-year-old lady presented to Department of Cardiothoracic Surgery with complaints of pain and swelling over the right side of the neck for the past six months. She attributed the pain to an injury sustained six months back. She gave a history of palpitations and occasional breathing difficulty. She had no difficulty in swallowing and no hoarseness of voice.
On general examination, she was healthy with no other significant abnormalities. Thyroid was normal. Examination of the neck did not reveal any obvious swelling. There was no regional nodal enlargement and palpation revealed a vague soft mass in the region of the sternocleidomastoid but the borders of the swelling were not discernible. There was no bruit or any pulsation over the swelling and there was no change in size with movement. The swelling appeared to be compressible and there was no cough impulse.
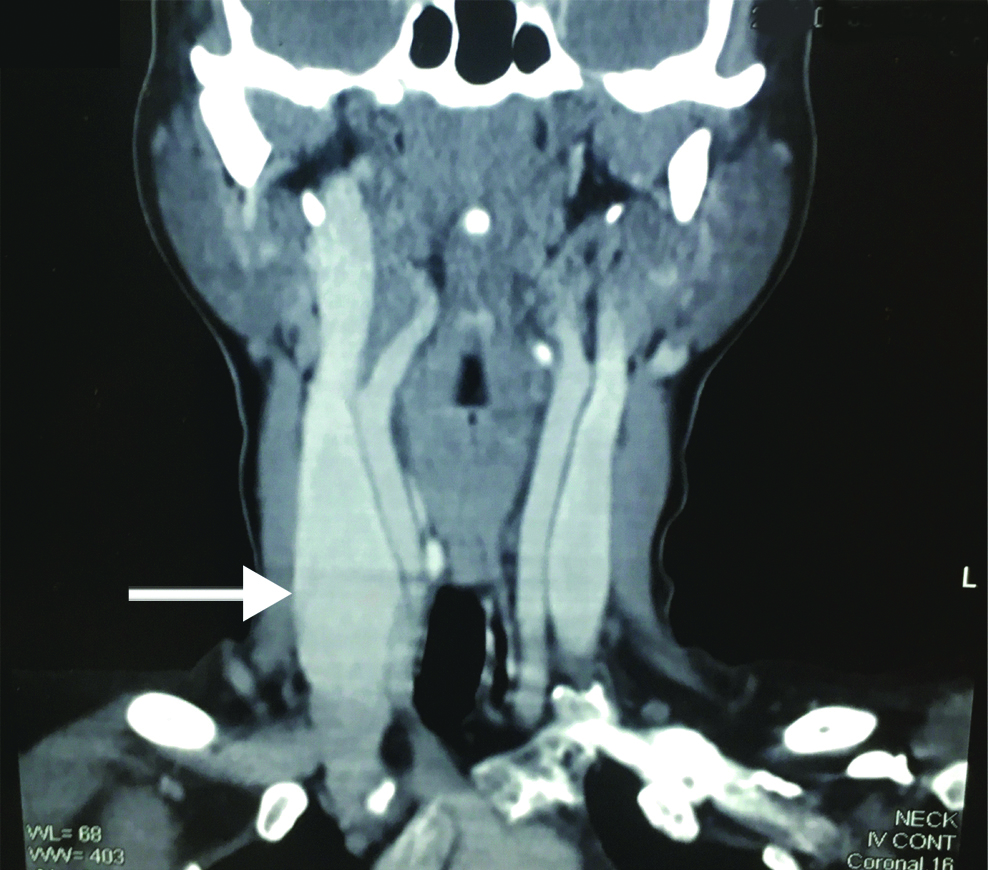
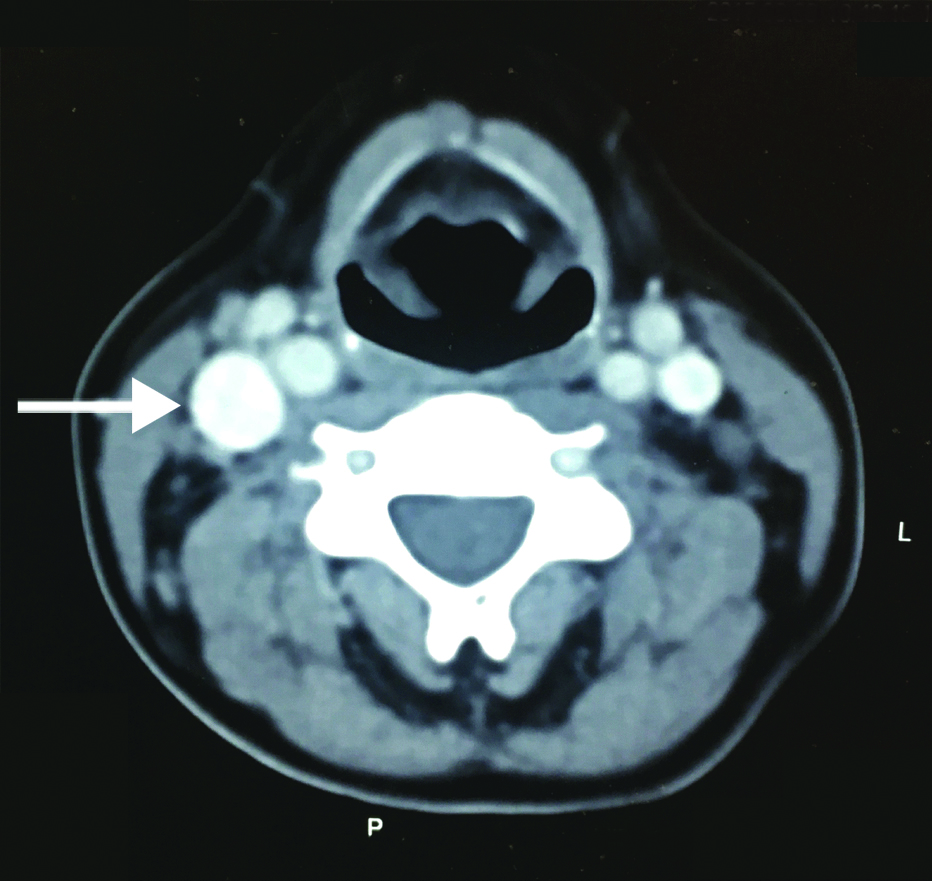
Chest radiograph and radiograph of the cervical spine were normal. An echocardiogram was done which showed normal left ventricular function and normal chamber dimensions. There was no abnormal venous drainage and the superior vena cava was normal in size. Computed tomography of the neck showed fusiform dilatation of the right internal jugular vein from the base of the skull to the level of C1 vertebra measuring 4.5 cm at its maximal width [Table/Fig-1,2].
Coronal section of the neck showing enlarged right internal jugular vein and normal left internal jugular vein.
Sagittal section showing enlarged right internal jugular vein when compared to the left.
As the patient did not have any disabling symptoms she was reassured and was advised regular follow-up.
Discussion
The term jugular ectasia was first coined by Zukschwerdt L [1] and was later characterised by Gerwig W [2]. Ectasia of the internal jugular vein may be fusiform or saccular. It is most commonly diagnosed in children; however rare in adults [3]. Though various theories (compression of the jugular vein between clavicle and apex of the lung, increased muscle tone of scalenus anticus, radiation) have been proposed but there is no proven acquired cause for the occurrence of this anomaly. Congenital ectasia of the jugular veins is a dilatation of the jugular bulb with a right sided predominance. This has been attributed to the course of the right brachiocephalic vein which is in the same direction as the superior vena cava. Hence, the increased pressure in the superior vena cava during inspiration may be directly transmitted to the right internal jugular vein. Also, the increased size of the right brachiocephalic vein when compared to the left and the presence of valves in the left brachiocephalic vein (4-8%) may contribute to the increased occurrence of this anomaly on the right side.
This condition is commonly diagnosed after excluding other differential diagnoses such as laryngocele, laryngeal diverticulae, branchial cysts, cystic hygroma, superior mediastinal cysts and tumours. Ultrasonography with Doppler and computed tomography can give an accurate diagnosis, with computed tomography, being able to give a better picture of the underlying structures [4]. Decreased elasticity of the jugular vein and increase in fibrous tissue has been observed in histopathological studies [5].
The occurrence of complications is very rare which includes thrombosis and hoarseness of voice and in asymptomatic patients, most authors advise monitoring of the size of the ecstatic segment periodically by means of ultrasound and to look for the occurrence of symptoms or complications [6]. Surgical management in these patients is required in the presence of complications such as thrombosis or for cosmetic reasons only. Surgery involves excision of the involved segment or scaffolding of the ectatic segment with 8 mm polytetrafluoroethylene tube graft [7].
Conclusion
Jugular vein ectasia presenting in an adult patient is rare and often leads to a diagnostic dilemma. Patients should be reassured that the condition is benign and should not be subject to an increased number of investigative modalities. Regular follow-up is all that is needed.
[1]. Zukschwerdt L, Seltene Lokalisation einer VenektasieDeutsche Zeitschrift für Chirurgie 1929 216(3-4):283-85.10.1007/BF02797034 [Google Scholar] [CrossRef]
[2]. Gerwig W, Internal jugular phlebectasiaAnnals of Surgery 1952 135(1):130-33.10.1097/00000658-195201000-0002114895158 [Google Scholar] [CrossRef] [PubMed]
[3]. Pandey M, Kumar P, Khanna A, Phlebectasia of the External Jugular Vein [Internet]Ispub.com 2008 [cited 14 July 2018] Available from: http://ispub.com/IJS/19/1/825210.5580/146a [Google Scholar] [CrossRef]
[4]. Bora M, Internal jugular phlebectasia: diagnosis by ultrasonography, doppler and contrast CTJ Clin Diagn Res 2013 7(6):1194-96.10.7860/JCDR/2013/5578.308523905140 [Google Scholar] [CrossRef] [PubMed]
[5]. Yokomori K, Kubo K, Kanamori Y, Takemura T, Yamamoto T, Internal jugular phlebectasia in two siblings: Manometric and histopathologic studies of the pathogenesisJournal of Pediatric Surgery 1990 25(7):762-65.10.1016/S0022-3468(05)80014-4 [Google Scholar] [CrossRef]
[6]. LaMonte S, Walker E, Moran W, Internal jugular phlebectasia: a clinicoroentgenographic diagnosisArchives of Otolaryngology-Head and Neck Surgery 1976 102(11):706-08.10.1001/archotol.1976.00780160102015 [Google Scholar] [CrossRef]
[7]. Balik E, Erdener A, Taneli C, Mevsim A, Sayan A, Yüce G, Jugular phlebectasia in childrenEuropean Journal of Pediatric Surgery 1993 3(01):46-47.10.1055/s-2008-10635078466876 [Google Scholar] [CrossRef] [PubMed]