Osteomas are rare, benign osteogenic neoplasms arising from the bone surface or medullary bone. They are most commonly encountered on the craniofacial skeleton. Complaints including pain and facial asymmetry are managed by surgical excision. The present study presents a case of mandibular osteoma in close relation to the mental nerve and discusses the use of ultrasonography guidance during excision surgery. USG guidance may be used intraoperatively as a cost-effective technique during surgeries of osteomas with close relations to vital structures.
Assisted surgery, Bone, Neoplasm, Osteoid osteoma, Postoperative complications
Case Report
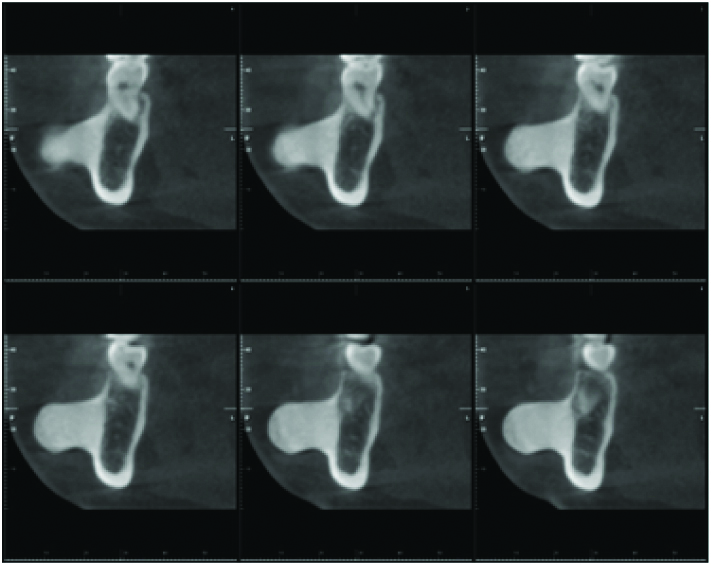
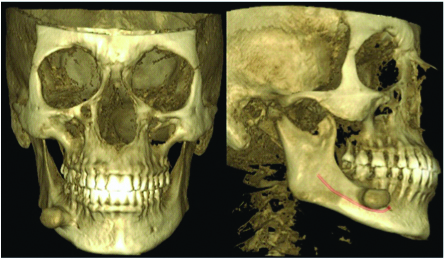
A 43-year-old female patient, referred with extra-oral swelling leading to pain and difficulty in mastication for 5 years. Her medical history was unremarkable. During palpation of the swelling located in the right mandibular premolar region, it appeared to be hard and immobile. Osteoma and osteochondroma was considered for differential diagnosis. Orthopantomograph (PlanmecaProline XC, Finland), revealed a radiopaque lesion and further detailed radiological evaluation was done with Cone-Beam Computerised Tomography (CBCT) (PlanmecaProMax CBCT, Finland) [Table/Fig-1], revealing the lesion to be in close relation with the mental foramen [Table/Fig-2].
CBCT views of the giant osteoma.
A 3D-CBCT view of the lesion revealing close proximity to the mental foramen.
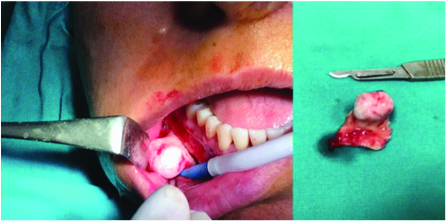
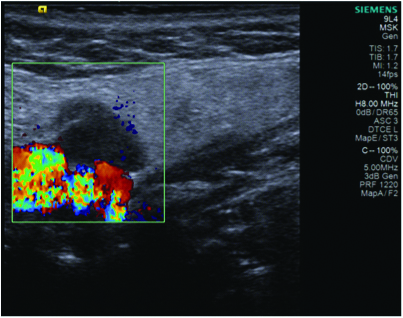
Intraoral approach was preferred for excision surgery and it was anticipated that the mental foramen would be lying under the osteoma, and visual communication would be limited. Therefore, USG guidance was practiced in order to protect the vital structures. USG investigation was carried out using Siemens Acuson S2000TM Ultrasound System, Germany with a linear transducer probe. Transducer was placed extraorally beneath the lesion in order not to disturb surgeon’s view of the surgical site. The pedicle of the osteoma was interrupted using round bur and split from the mandible was completed using osteotomes [Table/Fig-3]. During excision the integrity of mental vascular structures and the proximity of the surgical tools to the mental nerve were observed with USG [Table/Fig-4], Sharp bony spicules were softened before suturing. After excision of the lesion the mental nerve became observable and visual control was obtained, revealing an uninterrupted nerve.
Intraoperative view of the osteoma.
Intraoperative Doppler USG view of the mental structures.
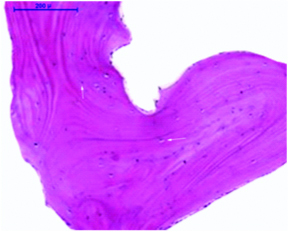
The mental nerve and vascular structures were protected. No intraoperative or postoperative bleeding was observed. Histopathological evaluation revealed dense, compact bone and broad trabeculae of mature bone. Outer surface was sharply demarcated [Table/Fig-5]. Healing was uneventful and no sensory impairment was documented after surgery. During 1.5 years of follow-up no recurrence was observed [Table/Fig-6].
Histopathological view of the lesion. (H&E, 10X).
Postoperative 1.5 years clinical photograph.

The authors read and worked in accordance with the Declaration of Helsinki, the Ankara University, Faculty of Dentistry IRB granted exemption in writing due to the retrospective nature of the study.
Discussion
Osteomas are benign, slow-growing, osteogenic neoplasms, arising from proliferation of either compact or cancellous bone surface (periosteal) or the medullary bone (endosteal) [1,2]. The pathogenesis of osteoma is unclear, although developmental anomalies, osteogenic reactions, infection and endocrine factors have been considered [1,3].
A consensus on the most common location has not yet been reported, although reported cases most commonly involve sessile or pedunculated masses on the lingual aspect, inferior border, sigmoid notch, coronoid process, genial tubercle, and condyle of the mandible [4], making the present case unique with localisation on the buccal aspect of the mandible.
Common opinion on age and gender predilection is also absent. It may occur in any age but it is more frequent in individuals over 40 as well as in this case [5]. Doctors must also be aware that when these pathologies are detected, patients should be scanned for a likely associated Gardner’s Syndrome [2,6].
Usually the appearance of osteomas is typical and does not present a problem for diagnosis. However exostoses, osteoblastoma, and central ossifying fibroma, or complex odontoma have been reported for differential diagnosis [7]. The overlying mucosa and soft tissues are usually normal in color and freely mobile unless trauma has occurred [6,8]. They radiographically appear as well-defined radiopaque masses in rounded shapes [1]. The peripheral type is usually clinically silent, but may produce swelling, cause aesthetic problems or problems in normal function. When osteomas are symptomatic or when aesthetic demands are in question, they are managed by surgical excision [1]. During surgery while using burs or osteotomes, protection of the surrounding vital structures is of course greatly important. Pedunculated lesions usually do not form complexity during surgical excision. In case of mandibular peripheral osteomas, intraoral surgical approach may be preferable to an extraoral surgical approach mainly because of risk of damage to the facial nerve and artery and postoperative scarring resulting in cosmetic problems [7]. Due to these risks, extraoral approach was not preferred in this case.
Knowledge of the normal anatomy of the mental foramen and its anatomical variations are crucial for oral maxillofacial and plastic surgeons, due to planning of various surgical procedures. Important operations related to mental foramen anatomy include: tooth extractions, removal of cysts and tumors, operations involving the lower lip and chin, reconstructive soft tissue procedures, endodontic surgery, orthognathic surgery, fixation of bone fractures and implant placement. Surgical procedures neighboring the mental nerve may be complicated by temporary or permanent sensory dysfunction and paraesthesia as a result of injury to the mental nerve. Therefore, the accurate determination of the position of the mental foramen is very important [6].
When the wide variation of jawbone lesions are considered, imaging techniques play a very important role in detection, diagnosis, treatment and follow-up of maxillofacial lesions [9]. Many imaging methods have entered the field of dentistry through technological developments. One of these imaging methods is Ultrasonography (USG), which is thought to be having an important potential for the maxillofacial region, although not widely used in dentistry [10].
USG is a non-ionising, synchronised, non-invasive and cost-effective imaging technique used in medical diagnostics and intraoperative guidance in several fields of medicine [11]. It transmits high-frequency ultrasonic pulses into the region of interest. Because of different densities of biologic tissues, different portions of the pulses are deflected back to the transducer and the device displays a grey scale image identifying tissue distance and tissue reflectivity. USG may not be able to adequately penetrate bone, but it can delineate bone surface morphology distinctively making it preferable in diagnosing bone diseases [11,12].
USG applications in oral medicine include the visualisation of the alveolar ridge, differentiating between periapical granulomas and cystic lesions, identification of dental cracks and planning of implant lengths. USG also allows a clear visualisation of the mental nerve, greater palatine nerve, lingual nerve and hard tissue surfaces such as bones, which are very important structures for dental surgery [9].
Screenings of osteomas via different radiographic modalities are well described, although the role of USG is not yet fully discussed. This may be because of the fact that imaging modalities like CT, CBCT or conventional radiography are highly reliable in imaging osteomas [13]. However, USG has been reported to show blood flow, which could prove critical for designing flaps and planning surgeries [11]. Chan et al., and Traxler et al., commented that USG provided accurate information about the position of the mental foramen [11,14]. Therefore, USG-guided surgery, might prove useful for surgical procedures involving the mental foramen, and may gain popularity over the years to come.
The use of intraoperative USG provides additional information like blood flow, nerve position and identification of lesion margins. This case report presents USG guided surgery of a solitary peripheral osteoma of the mandible and may be a pioneer for its field since no such case report involving surgical USG guidance for mandibular osteomas could be encountered during literature search. USG may be used for the purpose of planning surgeries and to improve the safety and efficacy of surgery.
[1]. Agrawal R, Agrawal S, Bhargava S, Motlani M, Agrawal R, An uncommon case of solitary peripheral osteoma in the mandibleCase Reports in Dentistry 2015 2015:31973810.1155/2015/31973826788378 [Google Scholar] [CrossRef] [PubMed]
[2]. Ragupathy K, Priyadharsini I, Sanjay P, Yuvaraj V, Balaji TS, Peripheral osteoma of the body of mandible: A case reportJournal of Maxillofacial and Oral Surgery 2015 14(4):1004-08.10.1007/s12663-014-0710-026604477 [Google Scholar] [CrossRef] [PubMed]
[3]. Ata-Ali J, Ata-Ali F, Giant peripheral osteoma of the mandible simulating a parotid gland tumorCortex 2016 1:2 [Google Scholar]
[4]. Sayan NB, Üçok C, Karasu HA, Günhan Ö, Peripheral osteoma of the oral and maxillofacial region: a study of 35 new casesJ Oral Maxillofac Surg 2002 60:1299-301.10.1053/joms.2002.3572712420263 [Google Scholar] [CrossRef] [PubMed]
[5]. Tuncer M, Aktaş A, Bayramov Dİ, Usubütün A, MandibuladaSıkRastlanmay an Periferal OsteomaHacettepe Dişhek Fak Derg 2007 31:47-51. [Google Scholar]
[6]. Sharma M, Peripheral osteoma of the mandible: case report and review of the literatureJournal of Kathmandu Medical College 2017 5(4):128-30.10.3126/jkmc.v5i4.18611 [Google Scholar] [CrossRef]
[7]. Bulut E, Acikgoz A, Ozan B, Gunhan O, Large peripheral osteoma of the mandible: a case reportInternational Journal of Dentistry 2010 2010:83476110.1155/2010/83476121331372 [Google Scholar] [CrossRef] [PubMed]
[8]. Patait M, Nipunge D, Thorat A, Narkhede S, Amberkar S, Diagnosis of osteoma of mandible with 3D cone beam CTInternational Journal of Applied Dental Sciences 2017 3(1):68-70. [Google Scholar]
[9]. Shahidi S, Shakibafard A, Zamiri B, Mokhtare MR, Houshyar M, Mahdian S, The feasibility of ultrasonography in defining the size of jaw osseous lesionsJournal of Dentistry 2015 16(4):335 [Google Scholar]
[10]. Laher AE, Wells M, Ultrasonographically locating the mental foramen and its soft tissue relationsDentomaxillofacial Radiology 2016 45(8):2016023610.1259/dmfr.2016023627506296 [Google Scholar] [CrossRef] [PubMed]
[11]. Chan HL, Wang HL, Fowlkes JB, Giannobile WV, Kripfgans OD, Nonionizing realtime ultrasonography in implant and oral surgery: A feasibility studyClinical Oral Implants Research 2017 28(3):341-47.10.1111/clr.1280526992276 [Google Scholar] [CrossRef] [PubMed]
[12]. Musu D, Rossi-Fedele G, Campisi G, Cotti E, Ultrasonography in the diagnosis of bone lesions of the jaws: a systematic reviewOral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2016 122(1):e19-e29.10.1016/j.oooo.2016.03.02227260284 [Google Scholar] [CrossRef] [PubMed]
[13]. Mehdizade A, Danon M, Ellis S, Wolfe S, Adler RS, Use of ultrasonographic guidance for needle localization of osteoid osteoma of the capitateHSS Journal 2006 2(2):176-80.10.1007/s11420-006-9015-218751833 [Google Scholar] [CrossRef] [PubMed]
[14]. Traxler M, Ulm C, Solar P, Lill W, Sonographic measurement versus mapping for determination of residual ridge widthJ Prosthet Dent 1992 67:358-61.10.1016/0022-3913(92)90246-7 [Google Scholar] [CrossRef]