The chemical-mechanical preparation with antimicrobial irrigating solutions and adequate apical instrumentation are the main factors that lead to the success of endodontic therapy [1,2]. Conventionally, the apical constriction or CDC (Canal-Dentinal-Cement) junction, usually located approximately 1 mm from the root apex, is the site where working length is ideally defined [3,4]. However, the presence of microorganisms in the cemental canal and its participation in the development of periapical lesions has suggested the need for mechanical cleaning up to the apical foramen or even beyond this in order to reduce the microbial load at the maximum extension of the root canal [5-8].
Although some studies have shown that over instrumentation may be more favourable for the repair of chronic periapical lesions [5], others have reported this technique as a traumatic procedure to the periapical tissues, generating the patient discomfort and post-operative pain [9,10]. The occurrence of post-operative pain is a major concern for both patients and professionals and even when the treatment has followed the highest standard, it is a common sensation after endodontic treatment. Studies have reported varying frequencies of pain in 25%-40% of all endodontic patients, including those with vital and non-vital pulp. The possible causes of post-operative pain are related to mechanical, chemical, and microbiological injuries to the periradicular tissues [11-13].
Mechanical allodynia is defined as a reduction in mechanical pain thresholds, manifested as sensitivity to percussion, biting, or pressure, and represents an essential feature of symptomatic periradicular inflammation [14]. Percussion test, often conducted by using a mirror handle, is the traditional method used to detect mechanical allodynia. However, its accuracy has been discussed because it is a subjective and non-quantifiable method, while mechanical allodynia shows a high sensitivity for detecting periradicular pain [15].
During the last decades, one-visit and two-visit endodontic treatments have gained special attention under different aspects, including post-obturation pain [12,13,16], bacterial disinfection [17,18] and tissue repair [1,16,19]. Traditionally, endodontic treatment of infected root canals is performed in multiple visits, using intracanal dressing between them, in order to eliminate microorganisms that survived biomechanical preparation [17]. On the other hand, single-visit root canal treatment has become a common practice with antimicrobial efficacy similar to two-visit treatment [1,16,18,19]. Furthermore, the use of rotary and reciprocating nickel-titanium files, new irrigation devices and more effective disinfection protocols make single-visit treatment more convenient. Reduced treatment time, better cost-effectiveness, patient acceptability, and reduced risk of contamination between sessions are some advantages of the single-visit treatment [16].
Thus, considering that instrumentation of the apical foramen remains a controversial issue, the purpose of this randomised clinical trial was to evaluate the influence of two different working lengths (0.0 mm and 1.0 mm beyond apical foramen) on post-operative pain after endodontic treatment completed in single-visit or two-visits. Additionally, the mechanical allodynia was also compared among treatment protocols.
Materials and Methods
Study Design
This study was a randomised, single-blind, comparative clinical trial with factorial analysis. The patients were allocated to receive one of the treatment protocols investigated according to the number of operative session and Working Length (WL) in the endodontic treatment. The protocol of the study was approved by the local Institute Review Board (CAAE: 50421215.9.0000.00077), and all the patients who volunteered signed an informed consent form.
Patient Selection
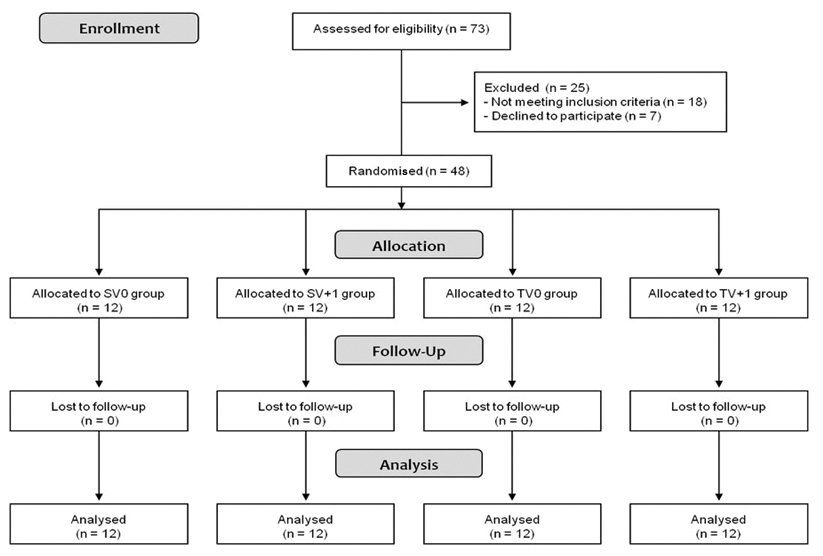
Seventy-three patients were initially recruited for the study, but 25 of them did not meet the inclusion criteria (n=18) or declined to participate in the research (n=7) and were excluded from the study [Table/Fig-1]. Thus, 48 adult patients (i.e., older than 18 years) attending Dental Specialty Center of the city of Bragança Paulista, São Paulo, Brazil, for primary endodontic treatment of maxillary or mandibular single-rooted teeth showing the presence of one root canal with pulp necrosis and asymptomatic apical periodontitis were included in the present study. Diagnosis was established by means of pulp sensitivity tests (negative response was chosen), apical palpation, horizontal and vertical percussion tests, and periapical radiographs (to evaluate the presence or absence of periapical lesions). Sample size was calculated with preliminary data from a pilot study using the software G*Power. Considering the ratio between final and initial forces obtained from 10 individuals treated in a single visit (in working lengths 0 and +1 mm from the apical foramen), with mean values of 1.028 and 1.1910, SD among individuals at 0.135, alpha set at 0.05 and power at 0.8, a total of 12 individuals per group were required to assess differences.
Flow diagram of the clinical trial.
The volunteers were recruited over a 6-month period spanning from January to June 2016. A detailed dental and general history was obtained from each patient. Those who had received any medicament (i.e., non-steriodal anti-inflammatory, analgesics of any kind, opioids, or corticoids) during the last 24 hour that could alter the perception of pain or interfere with the post-treatment pain score analysis, and those with any uncontrolled systemic disease, were excluded. All participants had maxillary or mandibular single-rooted teeth showing the presence of one root canal with straight (0 to 5 degrees) to moderate (10 to 20 degrees) curvature [20].
Randomisation
The 48 patients were randomly assigned to one of the following four groups (n=12) according to treatment protocol: SV0 group – single-visit root canal treatment and instrumentation performed on foraminal working length; SV+1 group – single-visit root canal treatment and instrumentation performed 1 mm beyond the apical foramen; TV0 group – two-visit root canal treatment and instrumentation performed on foraminal working length; TV+1 – two-visit root canal treatment and instrumentation performed 1 mm beyond the apical foramen. The participants were randomly allocated to one of the groups by means of a randomised list generated in a computer program (www.randomisation.com). Sealed opaque envelopes containing the treatment for each patient were numbered following the generated list and were opened by the operator only at the moment of the intervention. The patients were numbered according to the sequence of enrollment. As the study was a single blind trial, they were not informed about which specific treatment protocol would be used in their particular case.
Treatment Protocol
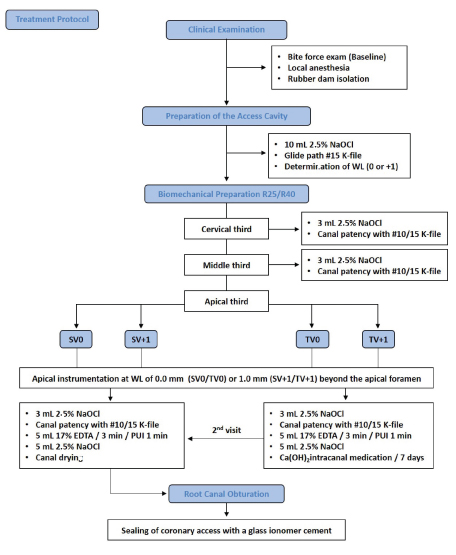
Endodontic treatment throughout the study was performed by a single operator [Table/Fig-2]. After a clinical examination, the patients were submitted to a bite force exam using a gnathodynamometer (digital dynamometer, IDDK model, Kratos, Bauru, SP, Brazil) to obtain the average power of pre-treatment baseline bite [Table/Fig-3]. Then, after local anaesthesia with 1.8 mL 2% lidocaine with epinephrine 1:100.000 (Alphacaine; DFL, Indústria e Comércio Ltda., Rio de Janeiro, RJ, Brazil), the access cavity was prepared under rubber dam isolation.
Flow diagram of the treatment protocol.
Bite force exam using a gnathodynamometer (digital dynamometer, IDDK model, Kratos, Bauru, SP, Brazil).

A glide path was established with #15 K-type hand file (DentsplyMaillefer, Ballaigues, Switzerland) and the WL was determined by introducing it up to the apical foramen as confirmed by a Root ZX II apex locator (J Morita Corp, Kyoto, Japan). For all study groups, apical instrumentation was performed with Reciproc® single-file instrument (VDW, Munich, Germany). The R25 files (25.08) were used in narrow and curved canals, and R40 files (40.06) were used in large canals. In SV0 and TV0 groups, the WL used was 0.0 mm from the apical foramen by introducing the file inside the canal until the “APEX” or “0.0” mark of the apex locator. In the SV+1 and TV+1 groups, the WL was 1 mm beyond the “APEX” or “0.0” mark. The WL was confirmed radiographically.
Reciproc instruments were used according to the manufacturer’s protocol, in a slow in-and-out pecking motion alternating with canal irrigation and file cleaning to prevent debris accumulation. Root canal preparation was performed in the cervical, middle, and apical thirds until attaining the WL. Irrigation with 3 mL 2.5% sodium hypochlorite (NaOCl) was performed using a 30-G NaviTip needle (Ultradent Products Inc, South Jordan, UT) after each file insertion, and the irrigant remained in the root canal throughout the entire procedure. Canal patency was maintained in all groups by passing a #10 or #15 K-type file (Dentsply) 1.0 mm beyond the apical foramen.
After concluding the instrumentation, the root canals were irrigated with 5 mL 17% EDTA solution (Inodon, Porto Alegre, RS, Brazil) that remained for 3 min and was agitated ultrasonically in the final minute with an Irrisonic tip (Helse, São Paulo, SP, Brasil) placed inside the canal up to 2 mm short of the foraminal WL, at a minimum power setting (10%). Afterward, final irrigation was performed with 5 mL 2.5% NaOCl and final aspiration was performed using a capillary tip (Ultradent Products Inc., South Jordan, UT, USA). All root canals received the same volume of irrigants during preparation. The teeth were then dried using Reciproc paper points (VDW).
In SV0 and SV+1 groups, the canals were subsequently filled with Reciproc gutta-percha cones (VDW) and AH-Plus sealer (DentsplyMaillefer, Ballaigues, Switzerland) using single-cone technique. In TV0 and TV+1 group, the root canals were filled with calcium hydroxide paste (UltraCalTM XS, Ultradent Products Inc.) using a 29-G NaviTip needle (Ultradent Products Inc.) and the teeth were sealed provisionally with glass ionomer cement (SS White Goods Dental Ltda, Rio de Janeiro, RJ, Brazil). After the period of 7 days, the intracanal medication was removed using #15 K-type hand file (Dentsply Maillefer) and 3 mL 2.5% NaOCl and the canals were filled in the same way described for the SV0 and SV+1 groups. The treatment phase was concluded by sealing the coronal access cavity with glass ionomer cement (SS White Goods Dental Ltd). The teeth were then X-rayed for evidence of adequate lateral filling of root canal.
Post-operative Pain Evaluation
All participants received a Visual Analog Scale (VAS) to record their assessment of pain at 3 hours, 6 hours, 12 hours, 24 hours, 48 hours, 72 hours and 7 days after the endodontic treatment. The VAS consisted of a horizontal line measuring 0-10 cm in length along which numeric values were grouped into visual categories. The patients were instructed to mark the point that was equivalent to their pain perception, with 0 indicating no pain and 10 indicating extreme pain. According to the values recorded on the VAS, the pain levels were classified in 4 categories: no pain (0), mild pain (1-3), moderate pain (4-7), and severe pain (8-10). The volunteers were informed to contact the professional if they experienced severe pain [9].
Record of Post-operative Mechanical Allodynia
For mechanical allodynia evaluation, bite force measurement was performed using a digital gnathodynamometer (digital dynamometer, IDDK model, Kratos) with a capacity of ~100 kgf (~980 N) at the tooth that has been treated endodontically, for all experimental groups, just before treatment (baseline) and 7 days after its conclusion [14,15]. This device is composed of a stainless steel cylinder (10×10 mm) which contains a load cell that measures force when deformed. Patients were seated erect with Frankfort plane parallel to the floor. The fork was placed unilaterally between the tooth treated endodontically and its antagonist. Subjects were instructed to bite on the fork as forcefully as possible for 3 seconds. Three measurements with a 40 seconds interval were made. The mean value found over these 3 measurements was recorded as the maximum bite force for that individual.
Statistical Analysis
All data were subjected to Gaussian distribution analysis (normality) using the Kolmogorov-Smirnov test. Statistica 8.0 software (Statsoft Inc., Tulsa, OK, USA) was used for the statistical treatment of results and the significance level was set at 5% (p<0.05).
As post-operative pain did not show Gaussian distribution curve, data were submitted to non-parametric tests. The Kruskal-Wallis test was applied to compare the level of post-operative pain among groups in each time assessment, and the Friedman test was used to determine significant differences on time assessments within each group.
Bite force data showed Gaussian distribution curve and significant differences among means of different groups were analysed using two-way repeated measures analysis of variance (ANOVA), followed by Tukey’s test. Allodynia data were initially submitted to one-way ANOVA to determine the homogeneity among initial data of tested groups.
Results
There were no losses during follow-up. Among the 48 patients analysed for the different treatment protocols (12 per group), 30 (62.5%) were female and 18 (37.5%) were male patients. The age of patients ranged from 18-71 year-old (mean age of 40 years). All of them answered the VAS satisfactorily at all the time points assessed (3 hours, 6 hours, 12 hours, 24 hours, 48 hours, 72 hours and 7 days).
Post-operative Pain Evaluation
Regarding post-operative pain, the VAS did not show any significant difference among the treatment protocols in any of the evaluated periods (p>0.05). The greater levels of pain was observed in the period of 12 hours after endodontic treatment for all groups, but there were no statistically significant differences among time assessments (p>0.05) [Table/Fig-4,5].
Mean and standard deviation of the pain scores of the treatment protocols at the different times. Kruskal-Wallis and Friedman tests showed no statistical difference among groups in each time assessment, as also among time assessments within each group (p>0.05).
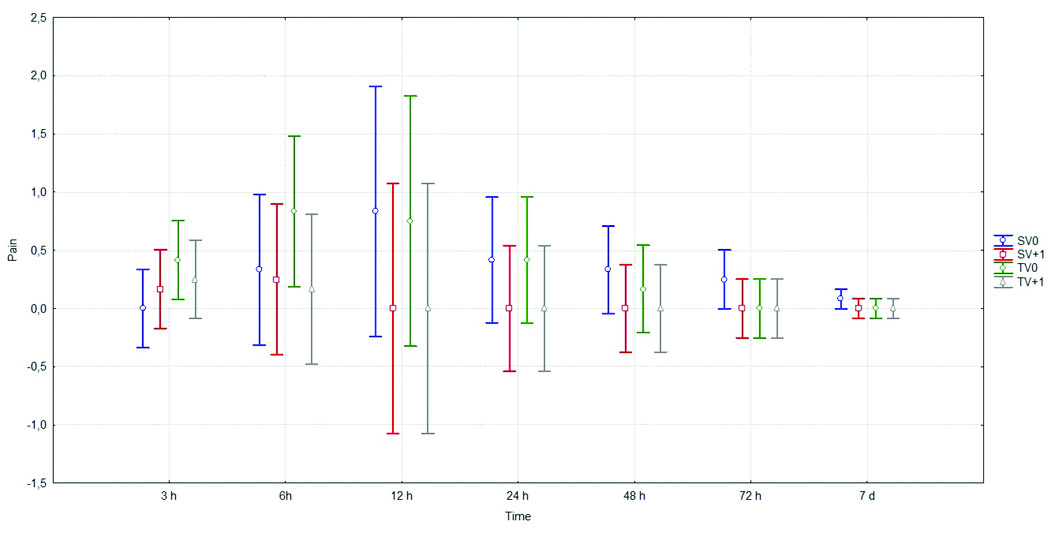
The mean and median (range) of visual analog scale pain values.
| Group | 3 hours | 6 hours | 12 hours | 24 hours | 48 hours | 72 hours | 7 days | p-value |
|---|
| SV0 | 0 aA0 (0-0) | 0.33 aA0 (0-4) | 0.83 aA0 (0-10) | 0.41 aA0 (0-5) | 0.33 aA0 (0-4) | 0.25 aA0 (0-3) | 0.08 aA0 (0-1) | p>0.05 |
| SV+1 | 0.17 aA0 (0-2) | 0.25 aA0 (0-2) | 0 aA0 (0-0) | 0 aA0 (0-0) | 0 aA0 (0-0) | 0 aA0 (0-0) | 0 aA0 (0-0) | p>0.05 |
| TV0 | 0.42 aA0 (0-2) | 0.83 aA0 (0-5) | 0.75 aA0 (0-8) | 0.42 aA0 (0-4) | 0.17 aA0 (0-2) | 0 aA0 (0-0) | 0 aA0 (0-0) | p>0.05 |
| TV+1 | 0.25 aA0 (0-2) | 0.17 aA0 (0-1) | 0 aA0 (0-0) | 0 aA0 (0-0) | 0 aA0 (0-0) | 0 aA0 (0-0) | 0 aA0 (0-0) | p>0.05 |
| p-value | p>0.05 | p>0.05 | p>0.05 | p>0.05 | p>0.05 | p>0.05 | p>0.05 | - |
Equal lowercase letters in the column represent no statistically significant difference among groups (Kruskal-Wallis, p < 0.05); Equal capital letters in the line represent no statistically significant difference among times (Friedman test, p < 0.05).
Record of Post-operative Mechanical Allodynia
One-way ANOVA showed no significant difference among the groups at the baseline, indicating that the initial data were homogeneous. For all experimental groups, bite force values were significantly higher 7 days after endodontic treatment, indicating that there was a significant reduction of mechanical pain in all groups (p<0.05). However, there was no significant difference among the groups regarding gain of strength (p>0.05) [Table/Fig-6,7].
Representative graph illustrating the performance of the bite force (Kgf) for each experimental group at the baseline and 7 days after endodontic treatment. Statistical analysis by ANOVA followed by Tukey’s test. Bars with different letters differ significantly among each other (p<0.05).
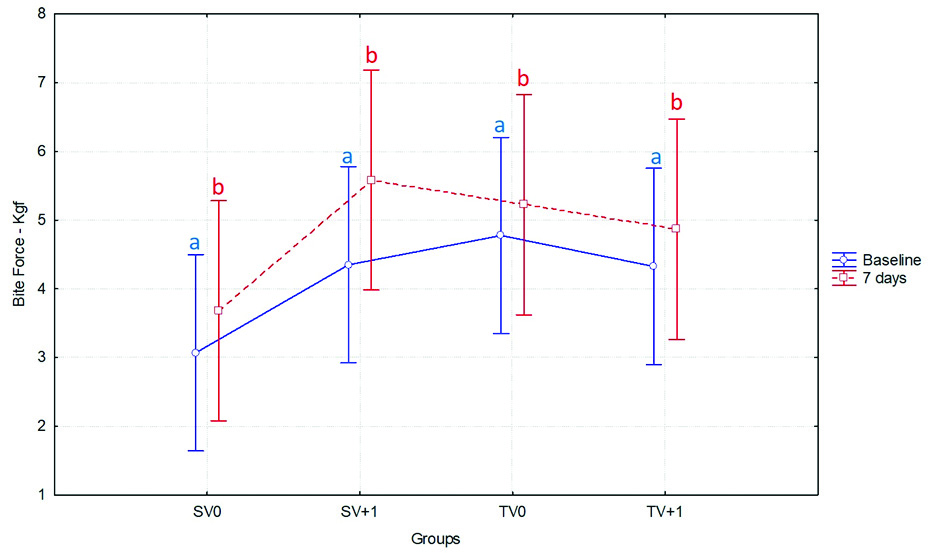
The mean and standard deviations of bite force (Kgf) values.
| Group | Baseline | 7 days | p-value |
|---|
| SV0 | 3.06±2.55 aA | 3.68±2.55aB | p<0.05 |
| SV+1 | 4.35±1.64aA | 5.58±2.10aB | p<0.05 |
| TV0 | 4.77±3.22aA | 5.22±3.88aB | p<0.05 |
| TV+1 | 4.32±2.11aA | 4.86±2.09aB | p<0.05 |
| p-value | p>0.05 | p>0.05 | - |
Equal lowercase letters in the column represent no statistically significant difference among groups; different capital letters in the line represent statistically significant differences among times (ANOVA and Tukey’s-test, p < 0.05).
Discussion
The reduction of microorganisms and biofilm dissolution are obtained through the mechanical instrumentation of the root canals and irrigation with tissue-dissolving antimicrobial solution [11]. In patients diagnosed with necrosis and apical periodontitis, higher foraminal contamination is expected, and a recommended treatment has been apical foramen enlargement to promote better disinfection and therefore, better conditions for tissue repair [5,11], which has been performed at working lengths ranging from 0 mm [6,9-11] to 1 mm [7,8] beyond the apical foramen. For this reason, considering the lack of studies that evaluate the clinical effects of this "overinstrumentation", the present investigation evaluated the occurrence of post-operative pain in teeth with asymptomatic apical periodontitis treated endodontically with Reciproc files, varying the working length (0.0 mm versus 1 mm beyond apical foramen) and the number of operative sessions (single versus two-visit). Only patients without pre-operative pain were selected for this study because pre-operative pain has the potential to significantly confound the results of post-operative pain in clinical trials [11].
Analyses of the results indicated that no statistically significant difference in post-operative pain was observed among the study groups, which suggests that working length up to 1 mm beyond the apical foramen and single or two-visit endodontic treatment has little or no influence on post-operative pain. This speculation is in agreement with other studies that found no significant difference [11] or a low incidence of pain [9] in the enlarged apical foramen group compared with the group without foraminal enlargement in teeth with a single root canal using hand K-files or Reciproc files, respectively. In opposition, Saini HR et al., reported that enlargement of the apical foramen in mandibular first molars with manual instrumentation increased the incidence and intensity of post-operative pain, and attributed this result to the extrusion of infected debris from the canals into the periapical space [10]. Contrasting results can be explained by differences in study designs, such as treatment protocols and teeth evaluated. The incidence of post-operative pain described in a recent research was only 33.33% for maxillary anterior teeth and 58.33% for mandibular molars [21].
Apical extrusion of debris and bacteria is one of the conditions associated with post-operative pain after root canal treatment. Manual instrumentation has demonstrated to cause more apical extrusion and increased incidence of post-operative pain [22,23]. Reciproc files were used in this trial to perform foraminal instrumentation because it outperformed preparation with nickel-titanium rotary files [24] and extruded fewer debris and bacteria apically [25-27], in addition to causing less foraminal transportation [7]. Moreover, other studies showed that reciprocating instruments did not influence the pain intensity and the overall incidence of pain was low [9,11], somewhat similar to current findings. However, some recent studies have reported controversial results regarding evaluations of debris extrusion [28] and post-operative pain [29] after root canal shaping with reciprocating systems. The low incidence of post-operative pain in this clinical trial may suggest that the debris/bacterial extrusions were not clinically significant using Reciproc. The highest levels of post-operative pain among the patients in all experimental groups were observed in the first 24 hours, which is in accordance with results reported by other authors [9,11,16,30] and its possible presence of pain in first 24 hours of inflammatory process, although there was no significant difference among the evaluation periods.
In this study, post-operative pain rate in single and two-visit endodontic treatment was similar to other studies which found no significant difference between single-visit and multiple-visit for post-operative pain [12,19,30]. Probably, it could be because of crown down technique of instrumentation using reciprocating motion allowing better irrigation and minimising the extrusion of debris beyond the apex [24-27], although “overinstrumentation” has been employed, According to Sathorn C et al., in a systematic review, there is no evidence of difference in post-operative pain or flare-up, and even healing rate, between single or multiple-visit root canal treatments [13]. Another recent systematic review [16] found that there is a lower frequency of short-term post-obturation pain after the single-visit than after multiple-visit root canal treatment, with no difference in the healing rate. These findings have reinforced the assumption that mechanical instrumentation and antimicrobial irrigation can significantly reduce the microbial load and single-visit endodontic treatment can lead to a favourable treatment outcome [16].
The diagnosis of apical periodontitis is often carried out with tests of limited accuracy and difficult validation. Acute inflammation of the periradicular tissues is characterised by a reduction in the threshold of mechanical pain, presumably caused by the sensitisation of nociceptors that innervate the periodontal ligament region. This reduction in the threshold of mechanical pain is called mechanical allodynia and is manifested as the sensitivity to percussion, biting, or pressure, and represents an essential feature of symptomatic periradicular inflammation [14]. Percussion test, often conducted by using a mirror handle, is the traditional method used to detect mechanical allodynia in patients with odontalgia. However, its accuracy has been questioned because it is a subjective, non-quantifiable method, and their results are inherently variable because of their force vectors, while mechanical allodynia shows a high sensitivity for detecting periradicular pain [15].
The measurement method of mechanical allodynia based on some articles that elucidate the use and their advantages such as increasing accuracy of bite force by giving a precise number which is totally different from percussion test, it is easy and safe to use [14,15]. Khan AA et al., tested the occlusal strength meter to calculate the mechanical allodynia and the efficiency of local anaesthesia in patients with irreversible pulpitis and acute periradicular periodontitis [14]. This study is part of a series of experiments testing the occlusal strength meter, evaluating the utility of the apparatus as a potentially suitable instrument for endodontic diagnosis and for conducting endodontic clinical trials. As a result, mechanical allodynia was reduced in 62% of the cases after the anaesthetic technique. The author concluded that the strength meter presents a quantifiable method for measuring the thresholds of mechanical pain in patients with toothache because of acute periapical conditions. According to the authors, using a standardised method to measure mechanical allodynia will provide a measure of the effectiveness of therapeutic interventions.
Taking this into account, the present study compared the levels of bite force among subjects undergoing the treatment protocols investigated as a resource to quantify pain and to improve the evaluation of post-operative pain after endodontic treatment. All the treatment protocols investigated increased the mechanical pain thresholds, with no significant difference among groups, but a significant increase in maximal bite force was observed 7 days after the endodontic treatment in relation to the baseline in all groups. This finding is in agreement with post-operative pain results obtained with the VAS and gives greater reliability to them because it is a more accurate test of the periapical inflammatory condition.
Limitation
This study achieved the minimal required number of participants but, due to the subjective and multifactorial nature of pain of endodontic origin, clinical studies with a greater number of patients are necessary to confirm the current results [10]. The limited time period of the study and the strict eligibility criteria adopted are among the factors that made it impossible to recruit a larger number of patients. Thus, more well-designed randomised clinical trials are needed to further investigate the differences of post-operative pain among the treatment protocols. In addition, follow-up after completion of treatment should be taken into consideration to evaluate the success of endodontic therapy.
Conclusion
In conclusion, the variation of the foraminal working length between 0.0 mm and 1 mm beyond the apical foramen using Reciproc files in asymptomatic necrotic teeth resulted in almost the same rate of low post-operative pain and mechanical allodynia after endodontic treatment completed in single-visit or two-visit.