About one in every three children have at least one episode of wheezing prior to their third birthday and cumulative prevalence of wheeze is around 50% at six years of age [1-3]. Recurrent wheeze is defined as three or more episodes of parentally reported wheeze in the past 12 months of life [3]. Its occurrence is quite common and is reported in 6.2% of the Indian children [4]. Although there are many risk factors responsible for the development of recurrent wheezing, recently, vitamin D has gained significant interest. Studies reported that low vitamin D levels even in cord blood may be responsible for many childhood diseases [5,6]. Consequently, more studies reported the association of low serum vitamin D levels and severe asthma in children [7-9]. Although there are many risk factors including infections and allergy, for the development of recurrent wheezing [10,11]; recently, vitamin D emerged as significant risk factor owing to its immunomodulatory properties [8,9,12].
Being a tropical country, vitamin D deficiency was thought of uncommon in India, however, contrary to this belief recent studies have shown its prevalence to be as high as 50-90% [13-15]. Previous studies from India used older definitions (<30 ng/mL) for defining vitamin D deficiency and insufficiency hence overestimated the association between vitamin D insufficiency/deficiency and wheeze [16]. Recent Indian as well as international guidelines redefined the vitamin D deficiency as well as insufficiency as advocate using the same for ensuring uniformity [13,17]. It was observed that lot of children visiting to emergency with recurrent wheeze did not have any underlying etiology except low vitamin D levels, on the other hand many children with even florid rickets doesn’t have wheeze. So, this study was planned to find out the association between serum vitamin D (25(OH) D) levels and recurrent wheezing in children less than three years of age in our population using standard definitions.
Materials and Methods
This was a hospital-based analytical case-control study performed in the Department of Pediatrics in collaboration with Department of Biochemistry of a tertiary care referral hospital from October 2013 to March 2015. Children less than three years of age, diagnosed with recurrent wheeze, presenting to emergency/outpatient department were enrolled after getting written informed consent. Those with underlying chronic/prolonged medical or surgical illness, clinical rickets received vitamin D supplementation in last six months or congenital malformations were excluded. Healthy age and weight matched children visiting outdoors for immunization or routine check-up were taken as controls.
The sample size was calculated using matched case-control study design. Assuming alpha equal to 0.05 and power of 80%, proportion of discordant pairs of type A (PA) among discordant pairs as 25%, and the proportion of discordant pairs (PD) among all pairs as 10%, the sample size required was 61 pairs.
Detailed history of wheezing episodes along with therapy, dietary history, sunlight exposure, respiratory system examination and anthropometry using WHO growth charts were recorded [18]. The study was approved by the Institute ethics committee.
Blood samples (2 mL) were taken in two plain vials. Subsequently, serum was separated by in-house centrifuge machine and was stored at -4°C. Serum analysis for 25(OH)D, calcium, inorganic phosphate, and alkaline phosphatase was done on the same day. Serum 25 (OH) D was measured by an ELISA kit from DLD Diagnostika GMBH (Alderhost, Hamburg, Germany). Serum 25(OH)D level of >20 ng/mL was considered sufficient, level between 12-20 ng/mL as insufficient, and <12 ng/mL was considered as deficient [17,19]. Recurrent early wheeze was defined as >2 reports of wheezing in the first 3 years of life [3].
Statistical Analisis
Data were collected on structured proforma and managed using Microsoft Excel spreadsheets. Subsequently, SPSS software version 20.0 was used for statistical analysis. Descriptive statistic was used for the characteristics of the study subjects. Comparison of continuous variables across two groups was done using Student’s t-test or Mann-Whitney U test. Statistical significance of categorical variables was determined by Chi-square test or Fischer-Exact test. Spearman rank correlation was calculated to find the strength of the relationship between various quantitative variables (vitamin D and ALP). A p-value of less than 0.05 was considered statistically significant.
Results
A total of 61 cases with recurrent wheeze along with 61 healthy controls were enrolled. The basic demographic characteristics i.e., age, sex, weight, and height [Table/Fig-1] was comparable in both the groups. Moreover, both the groups had very less but comparable sunlight exposure. The feeding pattern was significantly different between two groups. Most of the cases (63.9%) were exclusively and prolonged breastfed in contrast to controls in which most (72.10%) of the babies were started on complementary feeds at six months. There were no seasonal variations in the frequency of wheezing.
Baseline characteristics of the study population.
| Parameter | Cases (n-61) | Controls (n-61) | p-value |
|---|
| Age (months) Mean (SD) | 19.4 (9.1) | 20.9 (9.4) | 0.1 |
| Male n (%) | 31 (50.8) | 30 (49.2) | 0.4 |
| Weight (kg) Mean (SD) | 10.49 (1.7) | 12.75 (3.3) | 0.09 |
| Length (cms) Mean (SD) | 81.52 (8.5) | 82.10 (8.7) | 0.3 |
| Exclusively breastfed until 6 month of age n (%) | 39 (63.9) | 25 (40.9) | 0.005 |
| Complementary feeding: Started at 6 months n (%) | 21 (34.4) | 44 (72.1) | <0.001 |
| Sunlight Exposure <30 min/week n (%) | 44 (72.1) | 41 (67.2) | 0.2 |
The mean serum levels of 25-hydroxyvitamin D, calcium, and inorganic phosphate were significantly higher in controls compared to cases. Conversely, median serum ALP was significantly more in cases than the controls [Table/Fig-2]. Out of 122 children, 69 (56.6%) had vitamin D insufficiency and 15 (12.3%) had vitamin D deficiency. Around three-fourth of the cases (73.8%) and one third (39.3%) of the controls had insufficient vitamin D levels. However, significantly more cases were having vitamin D insufficiency and/or deficiency compared to controls.
Comparison of biochemical parameters among cases and controls.
| Parameter | Cases (n-61) | Controls (n-61) | p-value |
|---|
| Vitamin D level (ng/mL) Mean (SD) | 16.87 (4.9) | 27.23 (3.1) | <0.001 |
| Calcium(mg/dL) Mean (SD) | 8.67 (1.78) | 9.48 (1.43) | 0.003 |
| Inorganic phosphate (mg/dL) Mean (SD) | 4.82 (1.32) | 5.67 (1.41) | <0.001 |
| Alkaline phosphatase (IU/L) Median (1st, 3rd quartile) | 677 (478-819) | 317 (165-581) | <0.001 |
| Vitamin D insufficiency (<20 ng/mL) n (%) | 45 (73.8) | 24 (39.34) | <0.001 |
| Vitamin D deficiency (<12 ng/mL) n (%) | 14 (22.9) | 1 (1.6) | <0.001 |
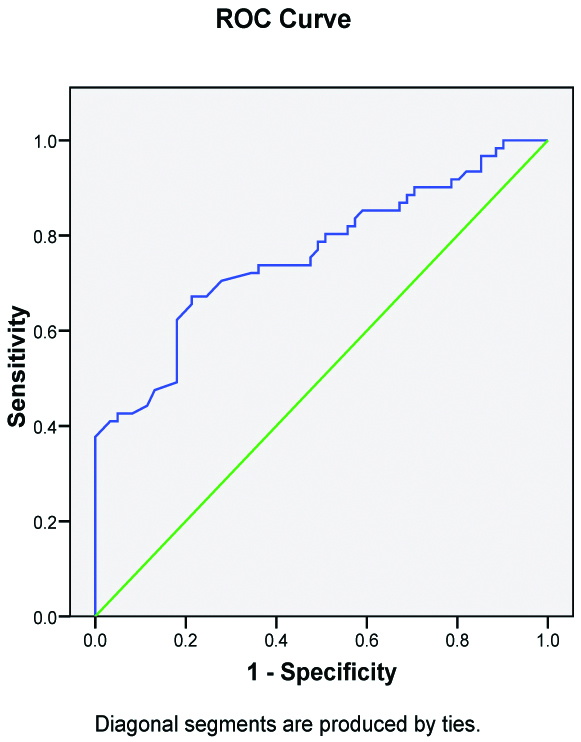
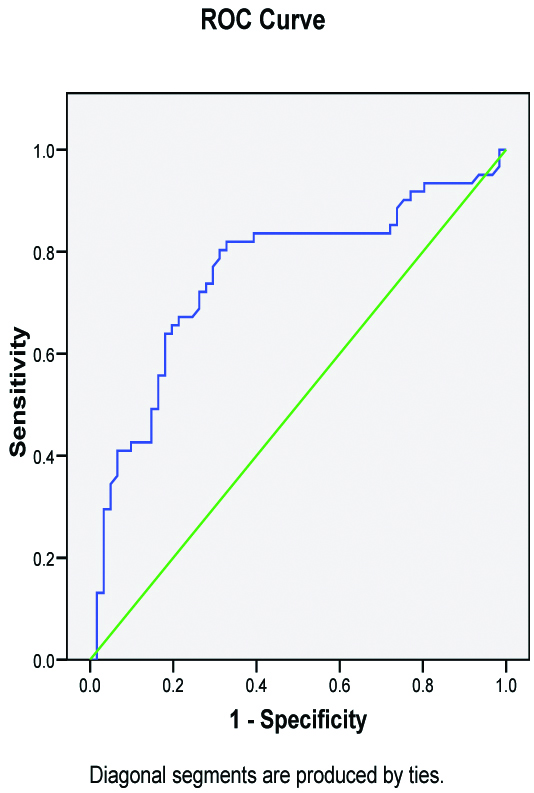
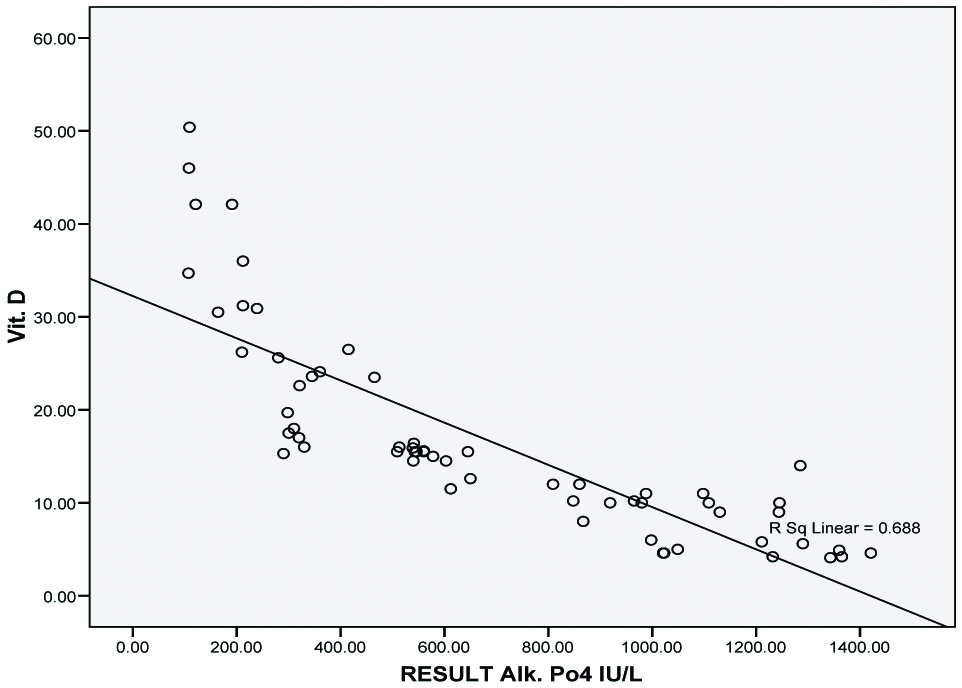
We also used ROC curve [Table/Fig-3] analysis and logistic regression to find out the cut-off value of serum 25(OH) D for predicting recurrent wheezing. The cut-off with maximum Youden’s index was 17.5 ng/mL, suggesting that any children less than three years with 25(OH) D level less than this value are more likely to have the recurrent wheeze. Furthermore, logistic regression shows that if 25(OH) D levels decrease by 1 ng/mL, the chances of wheezing increases by 7.3%. Similarly, for ALP the cut-off derived from ROC curve [Table/Fig-4] was 350 IU/L, suggesting that children with serum ALP more than 350 IU/L are more likely to have the recurrent wheeze. We also observed inverse relationship [Table/Fig-5] between serum vitamin D and serum ALP levels (k-0.688).
ROC analysis for vitamin D cut-off for wheezing.
ROC analysis for alkaline phosphatase cut-off for wheezing.
Inverse correlation between serum vitamin D and serum ALP levels.
All subjects with vitamin D insufficiency were separately analysed [Table/Fig-6]. Among them too, serum vitamin D and ALP levels were significantly different in cases and control. Most of the babies were exclusively breastfed until six months, however complementary feeding was not initiated at six months of age in most.
Analysis of subjects with vitamin D insufficiency.
| Parameter | Cases (n-45) | Control (n-24) | p-value |
|---|
| Sunlight exposure of <30 min/week n (%) | 37 (82.2) | 20 (83.3) | 0.9 |
| Exclusively breast fed until six months n (%) | 36 (80.0) | 17 (70.8) | 0.8 |
| Complementary feeding initiated at six months of age n (%) | 11 (24.4) | 10 (41.7) | 0.1 |
| Serum Vitamin D level (ng/mL) Mean (SD) | 11.4 (4.6) | 15.8 (2.4) | <0.001 |
| Serum Alkaline phosphatase level (IU/L) Mean (SD) | 838.16 (341.2) | 616.42 (283.1) | 0.005 |
| Serum Alkaline phosphatase>350 IU/L n (%) | 40 (88.9) | 18 (75.0) | 0.07 |
Discussion
The present study showed a strong association between vitamin D levels and recurrent wheeze in the children below three years of age. Serum vitamin D level below 17.5 ng/mL predisposes for the recurrent wheezing episodes and decrease in its level by 1 ng/mL in serum, increases the chances of wheezing by 7.3%. The prevalence of vitamin D insufficiency in the study population was very high (52.3%). Wheezing is quite prevalent in pre-school children and consequently, many children develop asthma [3]. Insufficiency/deficiency of vitamin D is widespread in all parts of the world [14]. 25(OH)D is the major stable and circulating form of vitamin D with a half-life of 2-3 weeks and its level is the best available indicators of vitamin D status [13]. Many cut-offs have been chosen to define insufficiency/deficiency of vitamin D but most of the guidelines meet consensus at a level of <20 ng/mL, to label as insufficient, this cut-off was chosen in concordance to international standards [14].
Vitamin D has an important role in the lung development and regulation of innate and adaptive immunity [20,21]. A significant association exists between the number of vitamin D receptors genes and the respiratory syncytial virus bronchiolitis [22]. Conversely, serum 25(OH)D levels are inversely related to respiratory viral infections in children [23]. So, there is enough evidence to conclude that vitamin D plays an important role in respiratory diseases like asthma and wheeze in children.
In this study mean levels of serum 25 (OH) D were significantly lower among cases (16.87±4.9) as compared to controls (27.23±3.1). Similar to other studies, in this study too, most of the children with recurrent wheeze (73.8%) had vitamin D insufficiency [16,24-26]. Ozdemir et al studied 186 infants with recurrent wheezing and found that children with recurrent wheeze had significantly lower vitamin D levels and the levels were much less in children who had the propensity to develop asthma based upon Asthma Predictive Index [26]. Hence, paving a way that recurrent wheeze with low vitamin D levels are at higher risk of developing asthma.
In present study, the prevalence of vitamin D insufficiency was very high (52.3%) but is in concordance with other Indian studies [13,14,24]. This finding again reinforces that vitamin D deficiency is a significant public health problem and there is urgent need of routine supplementation of vitamin D in all age groups along with food fortification.
This study adds that serum ALP > 350 IU/L (AUC-0.756), can be used as a surrogate of vitamin D insufficiency and is an important predictor (sensitivity 79%, specificity 69%) of recurrent wheeze. So, it can be used as a substitute in resource-limited settings.
Another eye-opening finding was that the majority of the wheezing children (63.9%) were exclusively breastfed till six months of age and complementary feeding was not started while the majority of the controls were mixed fed and complementary feeding was started at six months of age. This may be explained by the fact that human milk is a poor source of vitamin D, and in absence of supplementation, those who are exclusively breastfed are likely to develop vitamin D deficiency [13].
In this study breastfeeding rates were significantly higher in wheezers compared to controls, which is contrary to the belief that breastfeeding protects against allergic disorders. This finding is in concordance with a recent systematic review which showed that breastfeeding doesn’t protect against allergic disorders [27].
Sunlight exposure is an important factor for vitamin D synthesis. In our study, 82.2% of vitamin D insufficiency cases had limited sunlight exposure (<30 minutes per week), which may have contributed to such a high prevalence. The limited exposure seems to be due to change in lifestyle [28,29]. Studies have shown that a minimum 30-minute weekly sunlight exposure in bright sunlight, over 40% body area for at least four months is required to achieve sufficient vitamin D levels by six months of age [28].
Similar to vitamin D, children with recurrent wheeze also had significantly low calcium as well phosphate levels. These low levels may be partly due to vitamin D deficiency and poor dietary intake. In India along with vitamin D, calcium deficiency is also common and Indian Academy of Pediatrics recommend routine supplementation with calcium [13]. The current findings also support this recommendation.
Limitation
Limitation of this study was a small sample size. Also, detailed information about vitamin D intake was not collected and serum IgE levels were not measured.
Conclusion
Low serum 25(OH)D levels are strongly associated with recurrent wheezing in preschool children. In absence of vitamin D levels, high serum alkaline phosphatase levels (>350 IU/L) can be used as a predictor of recurrent wheeze. However, breastfeeding doesn’t seem to protect against recurrent wheezing.