Systemic Lupus Erythematosus Presenting with Finger Drop
Marjan Rahimi Farahani1, Samira Alesaeidi2
1 Resident, Department of Internal Medicine, Tehran University of Medical Sciences, Tehran, Iran.
2 Assistant Professor, Department of Rheumatology Research Center, Tehran University of Medical Sciences, Tehran, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Samira Alesaeidi, Assistant Professor, Department of Rheumatology Research Center, Tehran University of Medical Sciences, Tehran, Iran.
E-mail: kiani.sandra@yahoo.com
Systemic Lupus Erythematosus (SLE) is an autoimmune disease with multiple organ involvement that can affect joints, skin, heart, lungs, kidneys and nervous system. SLE is a multisystem disorder resulting from abnormal immunological function. SLE affects women more than men. It affects both the central and the peripheral nervous system. Severe acute peripheral neuropathy in SLE is quite rare and it is always accompanied by evidence of active disease in other organs, including the central nervous system. The recognition of neurologic symptoms in SLE remains a clinical problem for physicians. Neurological manifestations are frequently present in SLE patients, although the peripheral nervous system involvement is rarer than the central one. Peripheral neuropathy is a known but uncommon presentation of SLE and the aim of this study is to report various forms of lupus-related neuropathies that may present as finger drop and discusses one of the rare neurological manifestations of lupus which remains a diagnostic challenge.
Autoimmune diseases, Nervous system, Pathology
Case Report
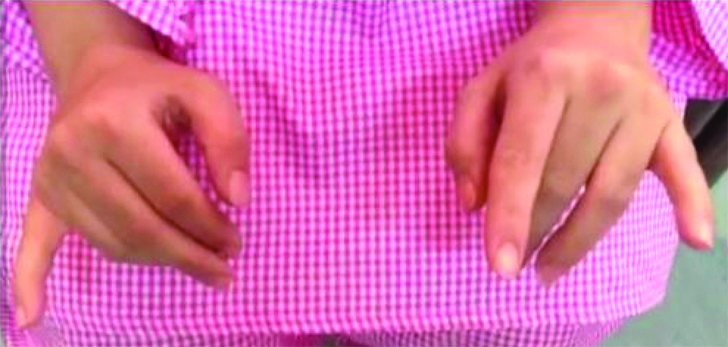
A 33-year-old female was referred to the hospital with a chief compliant of symmetric finger drop of second, third and fourth fingers without any wrist drop for nine months before. She was able to use her fists but she had limitation on abduction of all fingers and also full extension of metacarpophalangeal and interphalangeal joints. The evaluation of sensation and reflexes were normal. The patient complained of shoulder, wrist, interphalangeal, knee, and elbow and ankle arthralgia. Her affected joints had inflammatory pain and morning stiffness for about one hour. In her past history, she reported photosensitivity, alopecia, migraine headache and an abortion in eighth week of pregnancy. Therefore, in addition to the values of KFTs and urine examination, complement and Coombs’ tests were performed, which revealed lymphopenia, positive Anti β2 oneIgG and Anticardiolipin Ab (anti-body) IgG (more than three times), in two occasions, but negative lupus antibodies. Nevertheless, other examinations were normal. At first, she went to see the orthopaedist and with diagnosis of carpal tunnel syndrome, local steroid injection was done but since the patient’s symptoms did not improve after injection, she was referred to the rheumatologist for advanced evaluations [Table/Fig-1].
Finger drop during hand extension.
The patient was admitted and besides the hand exam, initial assessment revealed, malar rash, diffuse thinning and broken hairs, tenderness in wrists, elbows and shoulders. Therefore, in addition to routine blood examinations, antiphospholipid antibody panel, lupus antibodies (ANA subtypes, dsDNA Ab, Anti-Sm), complement and Coombs’ test were performed, which revealed lymphopenia, positive Anti β2 glcoprotein 1 IgG and Anticardiolipin Ab IgG (more than three times), in two occasions, but negative lupus antibodies. The patient did not have any symptoms of renal involvement at any time during the follow-up period. Urinalysis and serum creatinine were normal in all tests.
Then electromyography and bilateral radial nerves conduction were taken, EMG showed severe bilateral axonal neuropathy and the following results were obtained [Table/Fig-2].
The results of bilateral axonal neuropathy.
| Side | Muscle | Nerve | Spontaneous Activity | Volition | PSW | Fasc. | Poly. | Amp. | Interf. | Comments |
|---|
| Ins. | Fib. |
|---|
| Rt | Flex.C.rad | Median | Nl | 0 | 0 | 0 | 0 | Nl | Full | |
| Rt | FDI | Median | Nl | 0 | 0 | 0 | 0 | Nl | Full | |
| Rt | EI | Radial | Increase | +3 | +4 | 0 | Increase | Increase | Dec | Few MUAP |
| Rt | EDC | Radial | Increase | +3 | +4 | 0 | Increase | Increase | Dec | Dec MUAP |
| Lt | Flex.C.rad | Median | Nl | 0 | 0 | 0 | 0 | Nl | Full | |
| Lt | FDI | Median | Nl | 0 | 0 | 0 | 0 | Nl | Full | |
| Lt | EI | Radial | Increase | +3 | +4 | 0 | Increase | Increase | Dec | Dec MUAP |
| Lt | EDC | Radial | Increase | +3 | +4 | 0 | Increase | Increase | Dec | Dec MUAP |
| Lt and Rt | anconeous | Radial | Nl | 0 | 0 | 0 | 0 | Nl | Full | |
| Lt and Rt | Triceps | Radial | Nl | 0 | 0 | 0 | 0 | Nl | Full | |
Flex.c.rad: Flexor carpi radialis; FDI: First dorsal interosseous; EI: Extensor indicis; EDC: Extensor digitorum; INS: Insertion; FIB: Fibrillation; PSW: Positive sharp waves; Fasc: Fasciculations; Poly: Polyphasic; AMP: Amplitude; ITERF: Interference pattern; MUAP: Motor unit action potential; Dec: Decrease
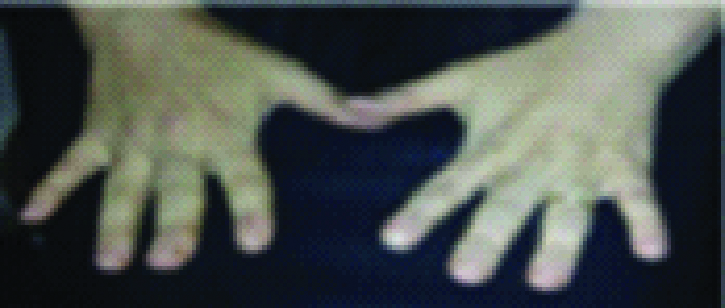
According to SLICC criteria the diagnosis of SLE was based on clinical findings and laboratory evidence. As a result, treatment with prednisone was started at a dose of 60 mg/day with intravenous cyclophosphamide pulses. After fifth months of treatment, FANA revealed positive result. Finally, the patient achieved a complete resolution of her peripheral neurologic symptoms after six cycles of cyclophosphamide [Table/Fig-3].
Fully recovery of peripheral neuropathy and finger drop after six months of immunosuppressive therapy.
Discussion
Systemic lupus erythematosus is a multisystem disorder resulting from abnormal immunological function [1]. Mononeuritis multiplex can sometimes be the initial presentation of SLE [2]. SLE affects both the central (CNS) and the Peripheral Nervous System (PNS). Severe acute peripheral neuropathy in SLE is quite rare and it is almost always accompanied by evidence of active disease in other organs, including the central nervous system [3]. Neurological manifestations are frequently present in SLE patients, although the initial presentation of lupus as Mononeuritis multiplex is rarer than the central one. Peripheral neuropathy is a relatively uncommon finding in SLE and occurs more frequently in patients with central nervous system involvement and high SLE-disease activity index. The nervous system involvement is associated with a worse prognosis. Finger drop is a rare neurological disorder in the field of lupus and it can affect the quality of life of individuals. The causes of finger drop are limited; however, the most important causes include neurologic and orthopaedic disorders and we should also be aware of the importance of diagnoses. Common neurologic causes are motor neuron disease (amyotrophic lateral sclerosis form), posterior interosseous nerve palsy, myasthenia gravis, syringomyelia, distal myopathies and cortical hand. Orthopaedic disease can also lead to finger drop, including posterior interosseous nerve palsy, ruptured extensor tendon, extensor tendon subluxation and trigger finger [4]. The main cause of finger drops in our patients associated with dorsal interosseous nerve involvement. The most common type of PN is symmetric polyneuropathy with sensory involvement. Mostly lower limb nerves are involved. The prevalence of PN in SLE is relatively high and occurs more frequently in patients with central nervous system involvement and high SLE-disease activity index [5]. Based on SLE Disease Activity Index 2000 (SLEDAI-2K), our patient scored 24 points in severity and after treatment, the symptoms of the patient improved and the score decreased to zero.
In a study conducted by Oomatia A et al., over a 25-year study period, the overall prevalence of peripheral neuropathies was 5.9%, with 66.7% having peripheral neuropathies attributable to SLE [6].
According to the recommendations of the management of neuropsychiatric manifestations in SLE, our patient was treated with high doses of corticosteroid and cyclophosphamide and neurological symptoms have completely improved. Intravenous Cyclophosphamide is recommended in severe neuropsychiatric SLE which is administered as a monthly pulse [7]. A controlled clinical trial in SLE patients with severe Peripheral Neuropathy (PN) manifestations showed that Intravenous (IV) cyclophosphamide treatment was more effective than IV methylprednisolone [8]. In addition, a previous retrospective study indicated that cyclophosphamide could prevent the relapse of vasculitic PN case [9]. Rituximab, intravenous immunoglobulins, or plasmapheresis may be used if response is not achieved. Mononeuritis multiplex (as seems to be this case) is a well-established though admittedly rare manifestation of SLE. The response to immunosuppressant drugs like cyclophosphamide to all inflammatory manifestations of lupus are also well established [10] which can be associated with favorable clinical outcomes and can be useful in controlling neurological symptoms. The most common manifestation of PNS involvement in SLE is symmetric polyneuropathy [11]. This case presenting as Mononeuritis multiplex (MM) of bilateral posterior interosseous nerves is, to the best of our knowledge the first case report of SLE presenting as MM involving bilateral PIN. Mostly lower limb nerves are commonly involved.
Conclusion
Systemic lupus erythematosus is similar to many autoimmune rheumatic diseases and may present atypically, lack a pathognomonic feature and run a dynamic course. Peripheral neuropathy is a known but uncommon presentation of SLE. This article reported various forms of lupus-related neuropathies that may present as finger drop and discussed one of the rare neurological manifestations of lupus which remains a diagnostic challenge. Our case report showed the first finger drop case as a rare clinical presentation of SLE patients presenting as MM and beneficial effect of immunosuppressive therapies. This condition is in the differential diagnosis for many neurologic conditions. Thus, neurologists and other clinicians need to be aware of the various presentations and neurologic complications of SLE. This case presenting as MM of bilateral posterior interosseous nerves is, to the best of our knowledge the first case report of SLE presenting as MM involving bilateral PIN. Mostly lower limb nerves are commonly involved.
Consent, for the publication for this case report and any additional related information was taken from next of kin of patient involved in the study.
Flex.c.rad: Flexor carpi radialis; FDI: First dorsal interosseous; EI: Extensor indicis; EDC: Extensor digitorum; INS: Insertion; FIB: Fibrillation; PSW: Positive sharp waves; Fasc: Fasciculations; Poly: Polyphasic; AMP: Amplitude; ITERF: Interference pattern; MUAP: Motor unit action potential; Dec: Decrease
[1]. Pons-Estel GJ, Alarcón GS, Scofield L, Reinlib L, Cooper GS, Understanding the epidemiology and progression of systemic lupus erythematosusSemin Arthritis Rheum 2010 39:257-68.10.1016/j.semarthrit.2008.10.00719136143 [Google Scholar] [CrossRef] [PubMed]
[2]. Hughes RA, Cameron JS, Hall SM, Heaton J, Payan J, Teoh R, Multiple mononeuropathy as the initial presentation of systemic lupus erythematosus-nerve biopsy and response to plasma exchangeJ Neurol 1982 228:239-47.10.1007/BF003134146188811 [Google Scholar] [CrossRef] [PubMed]
[3]. Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosusArthritis Rheum 2012 64:2677-86.10.1002/art.3447322553077 [Google Scholar] [CrossRef] [PubMed]
[4]. Varatharaj A, Pinto A, Manning M, Differential diagnosis of finger dropNeurologist 2015 19(5):128-31.10.1097/NRL.000000000000002125970834 [Google Scholar] [CrossRef] [PubMed]
[5]. Florica B, Aghdassi E, Su J, Gladman DD, Urowitz MB, Fortin PR, Peripheral neuropathy in patients with systemic lupus erythematosusSemin Arthiritis 2011 41(2):203-11.10.1016/j.semarthrit.2011.04.00121641018 [Google Scholar] [CrossRef] [PubMed]
[6]. Oomatia A, Fang H, Petri M, Birnbaum J, Peripheral neuropathies in systemic lupus erythematosus: clinical features, disease associations, and immunologic characteristics evaluated over a twenty-five-year study periodArthritis Rheumatol 2014 66(4):1000-09.10.1002/art.3830224757151 [Google Scholar] [CrossRef] [PubMed]
[7]. Petri M, Brodsky R, High-dose cyclophosphamide and stem cell transplantation for refractory systemic lupus erythematosusJAMA 2006 295:559-60.10.1001/jama.295.5.55916449623 [Google Scholar] [CrossRef] [PubMed]
[8]. Barile-Fabris L, Ariza-Andraca R, Olguín-Ortega L, Jara LJ, Fraga-Mouret A, Miranda-Limón JM, Controlled clinical trial of IV cyclophosphamide versus IV methylprednisolone in severe neurological manifestations in systemic lupus erythematosusAnn Rheumatic Dis 2005 64(4):620-25.10.1136/ard.2004.02552815769918 [Google Scholar] [CrossRef] [PubMed]
[9]. Mathew L, Talbot K, Love S, Puvanarajah S, Donaghy M, Treatment of vasculitic peripheral neuropathy: a retrospective analysis of outcomeQJ Med 2007 100:41-51.10.1093/qjmed/hcl12517189246 [Google Scholar] [CrossRef] [PubMed]
[10]. Martinez-Taboada VM, Alonso RB, Armona J, Fernandez-Sueiro JL, Gonzalez CV, Rodriguez-Valverde V, Mononeuritis multiplex in systemic lupus erythematosus: response to pulse intravenous cyclophosphamideLupus 1996 5(1):74-76.10.1177/0961203396005001148646231 [Google Scholar] [CrossRef] [PubMed]
[11]. Londhey VA, The most common manifestation of PNS involvement in SLE is symmetric polyneuropathyJ Assoc Physician India 2015 63(12):11-12. [Google Scholar]