Case 1
A five-year-old male presented with a two-year history of gradual progressive painless swelling of eyes, jaws and neck which started in the right upper eyelid and gradually extended to involve the lower eyelids [Table/Fig-1]. There were associated bilateral itchy eyes discharging yellowish fluid with significant weight loss. However no dysphagia, dyspnea, snoring, halitosis, abdominal or urinary symptoms nor obvious masses in other parts of the body were seen.
Summary of clinical presentations.
| S/N | | Case 1 | Case 2 | Case 3 |
|---|
| 1 | Age | 5 yrs | 14 Yrs | 7 yrs |
| 2 | Sex | Male | Male | Male |
| 3 | Place of presentation | CHOP | CHOP | CHOP |
| 4 | Classical Symptoms | Gradual progressive painless swelling of eyes, jaws and neckNo fever | Bilateral painless neck swelling and low-grade fever | Recurrent painless right neck swelling, No fever |
| 5 | Duration of Symptoms before presentation | 2 yrs | 3 months | 2 yrs |
| 6 | Lymph nodes | Submental, submandibular and cervicallymph nodes | Preauricular, submandibular, cervical, axillary and inguinal lymph nodes | Submental, cervical, axillary and inguinal lymph nodes. |
| 7 | Duration of therapy | 2 yrs | 1 1/2 yrs | 1 yr |
| 8 | Type of lesion/location | Ocular, lymph nodes | Tonsils, Lymph nodes, cutaneous | Lymph nodes |
| 9 | Spleen, liver and kidney involvement | Mild hepatomegaly | nil | nil |
| 10 | Weight loss | Weight loss (22% of expected) | No Weight loss | Weight loss |
| 11 | Provisional diagnosis | AML (Acute Myeloid Leukaemia) | Hodgkin’s lymphoma | NonHodgkin’s lymphoma |
| 12 | Differential diagnosis | Neuroblastoma, sarcoidosis. | Tuberculous lymphadenitis, Infectious mononucleosis | Tuberculous lymphadenitis, Rhabdomyosarcoma |
| 13 | Therapy | Tabs prednisolone 12.5mg twice daily | Tabs Prednisolone 30mg twice daily, Caps Augmentin 625mg twice daily x 1/52, and tab vitamin C 100mg thrice daily | Tabs prednisolone 5mg bd and tabsVitamin C 100mg thrice daily |
| 14 | Initial response | 5 months after commencement of therapy there was significant reduction in the size of the masses. | 3 months later - cervical nodes had markedly reduced in size, and the inguinal nodes were non-palpable6 months - the lymph nodes were no longer palpable | 7 months after commencement of therapy the neck swellings had markedly reduced in size |
| 15 | Complications | Cushingoid facies, Tinea capitis | - | Generalized skin rashes |
| 16 | Treatment of complications | Prednisolone replaced with methylprednisolone + ketoconazole cream | Prednisolone dose gradually reduced to 5mg alternate daily, Dapsone, Erythromycin (tablets and cream), Flucloxacillin, Mupiderm, cream Retin-A, Mary Kay acne gel | Prednisolone therapy was stopped briefly |
| 17 | Other involvements | Eyes - bilateral firm nontender eyelid swellings | Tonsils - Bilateral hyperemic tonsils.Skin - Bilateral maculo-papular lesions on axillary and the supra pubic regions | nil |
| 18 | Outcome | Relapse after the initial response, and the patient was lost to follow-up 2 years later. | Full recovery-after 18 months of therapy | Partial recovery but Lost to follow up 1 year after commencement of therapy. |
CHOP: Children Out Patient;
Clinical examination revealed, a chronically ill-looking pale child, with respiratory rate-30 breaths/minute, pulse rate-96 beats/minute, weight-14kg (78% of expected), with bilateral firm nontender eyelid swellings with chemosis, prominent veins, excessive tearing and yellowish discharge. There were discrete nodular jaw swellings; submental, submandibular and cervical lymphadenopathy but no other palpable lymph nodes and no intraoral extension or dental anarchy. Patient’s occipitofrontal circumference was 49.5cm, mid upper arm circumference was 14cm and height was 106cm (99% of expected). Abdomen was full on examination with only mild hepatomegaly but no other palpable abdominal organs, masses nor ascites. An impression of lymphoproliferative disorder probably AML (Acute Myeloid Leukaemia) was made to rule out neuroblastoma and sarcoidosis [Table/Fig-1].
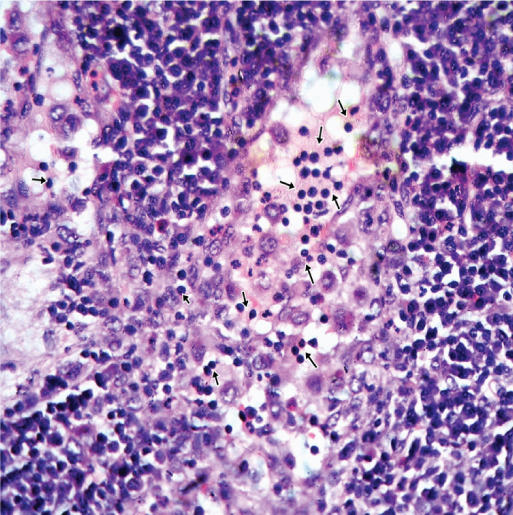
Urgent haemoglobin estimation was done (Hb -8.2g/dL) and the patient was transfused. Other laboratory investigations were Erythrocyte Sedimentation Rate (ESR) - 119mm 1st hour, platelet count - 109000/mm3, Mean Corpuscular Volume (MCV)-72.5fl, Mean Corpuscular Haemoglobin Estimation (MCHC)-27.6; total White Cell Count (WBC)- 3200/mm3 (neutrophils 53%, lymphocytes 37%), serum uric acid- 0.31 [Table/Fig-2]. The serum electrolytes, urea and creatinine (SEUCr) were within normal limits. The skull X-ray showed massive soft tissue swelling with no bony involvement but the abdominopelvic ultrasonography was unremarkable. Fine needle aspiration cytology of the masses showed proteinaceous material with a predominance of mature and maturing lymphocytes compatible with a diagnosis of lymphoproliferative disease [Table/Fig-2]. On gross examination, the excision biopsy of left cervical lymph node showed a nodular tissue measuring 1.5x1x0.3 cm with solid, grayish white cut surfaces. The microscopic examination showed lymph node tissue with pronounced dilatation of the sinuses, predominantly occupied by histiocytes with large vesicular nucleus and abundant clear cytoplasm with many containing intact lymphocytes (emperipolesis) [Table/Fig-3]. A histopathological diagnosis of Rosai-Dorfman’s disease (sinus histiocytosis with massive lymphadenopathy) was made and the patient was commenced on tablet prednisolone 12.5mg twice daily. There was a significant reduction in the size of the masses at five month assessment after commencement of therapy but patient developed cushingoid facies following which prednisolone was withdrawn and replaced with methylprednisolone. Patient also developed Tinea capitis which was managed with ketoconazole cream. After the initial response, the masses began to increase in size again and the patient was lost to follow-up two years later.
Summary of laboratory findings.
| S/N | Test | Case 1 | Case 2 | Case 3 |
|---|
| 1 | Hb | 8.2g/dl | 9.8 g/dl | 9.8 g/dl |
| 2 | PCV | 25% | 30% | 31%; |
| 3 | Platelet count | 109000/mm3 | 235x109/L, | 150x109/L, |
| 4 | ESR | 119mm 1st hour | 99mm 1st hour | 65mm 1st hour |
| 5 | Total WBC | 3200/mm3(N - 53%, L -37%) | 8.5x109/L (N-65%, L-31%, E-2%, M-2%) | 2.5x109/L (N-63%, L-36%, M-01%) |
| 6 | Peripheral blood film | Within normal limits | Mild hypochromasia, few toxic granules of neutrophils, platelets-appear adequate and normal | Within normal limits |
| 7 | SEUCr | Within normal limits | Within normal limits | Within normal limits |
| 8 | Mantoux | Negative | Negative | Negative |
| 9 | HIV I & 2 antibodies | Negative | Negative | Negative |
| 10 | Skull X-ray | massive soft tissue swelling with no bony involvement | Within normal limits | Within normal limits |
| 11 | Chest X-ray | Not done | Within normal limits | Within normal limits |
| 12 | Abdominopelvic ultrasonography | Within normal limits | Not done | Within normal limits |
| 13 | Fine needle aspiration cytology | Predominance of mature and maturing lymphocytes compatible with a diagnosis of - Lymphoproliferative disease. | Not done | Not done |
| 14 | Excision biopsy of cervical lymph node | Sinus histiocytosis with massive lymphadenopathy | Sinus histiocytosis with massive lymphadenopathy | Sinus histiocytosis with massive lymphadenopathy |
Hb: hemoHaemoglobin Concentration; PCV: Packed Cell Volume, ESR: Erythrocyte Sedimentation Rate, Total WBC: Total White Blood Cell Count; N: Neutrophils; L: Lymphocytes; E: Eosinophils; M: Monocytes; Seucr: Serum Electrolyte Urea; Creatinine Concentration
Photomicrograph of case 1 lymph node showing many histiocytes with several intact lymphocytes within their cytoplasm (emperipolesis] (short arrows) (H&E, 400X).
Case 2
A 14-year-old male presented with a three month history of bilateral neck swelling and fever. The swelling was nontender and started initially in front of the ears but gradually spread to involve the jaw and groin areas bilaterally. The fever was low grade, intermittent, with associated chills but there were no associated rigors, catarrh, cough, night sweats, weight loss nor significant medical or family history. Patient was initially treated with Augmentin before referral to our hospital for expert management.
Clinical examination revealed a male teenager, afebrile (37.2°C), not pale, anicteric, not cyanosed, not dehydrated and had significant lymphadenopathy involving the preauricular, submandibular, cervical, axillary and inguinal groups of lymph nodes. The nodes were rubbery, some mobile, others matted together and attached to underlying structures, but not attached to overlying skin; with no differential warmth elucidated. Patient also had bilateral hyperemia of the tonsillar area and bilateral maculo-papular lesions on both axillary and the supra pubic regions [Table/Fig-1]. The respiratory rate was 28 breaths/minute, pulse rate -100 beats/minute and Blood Pressure (BP) -90/60mmHg.
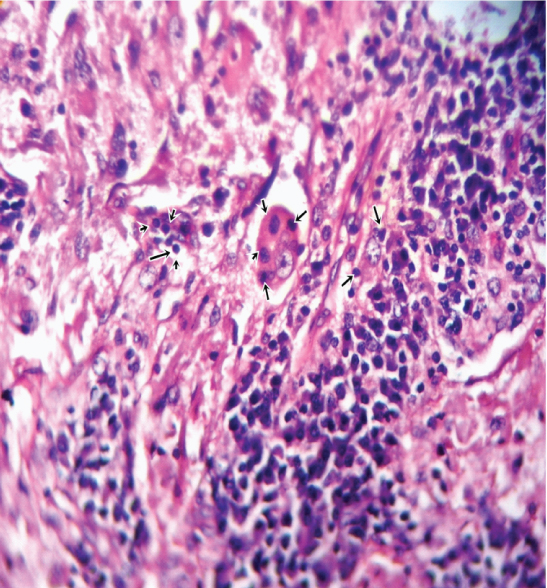
An impression of Hodgkin’s lymphoma to rule out Tuberculous Lymphadenitis (TBLN) and Infectious mononucleosis was made and an excision of cervical lymph node biopsy was done [Table/Fig-1]. The laboratory investigations were: Hb-9.8 g/dL; PCV 30%; total WBC- 8.5x109/L (N - 65%, L - 31%, E - 2%, M -2%); ESR-99 mm 1st hour; platelets- 235x109/L, peripheral blood film–mild hypochromasia and few toxic granules of neutrophils, platelets appear adequate and normal, negative HIV I & 2 antibodies. The SEUCr was within normal limits but the Skull X-ray showed massive soft tissue swelling with no bony involvement [Table/Fig-2]. The gross examination of the excision lymph biopsy showed two nodular lessions measuring 2x1x1 cm and 1x0.5x0.3 cm with solid, greyish white cut surfaces. The microscopic examination showed pronounced dilatation of the sinuses predominantly occupied by histiocytes with large vesicular nucleus and abundant clear cytoplasm, many of which contained numerous intact lymphocytes (emperipolesis) with the intersinusal tissue exhibiting a variable number of plasma cells [Table/Fig-4]. A histopathological diagnosis of Rosai-Dorfman disease was made and the patient was subsequently treated with tabs Prednisolone 30mg bd, caps Augmentin 625mg bd x 1/52 and tabs Vit C 100mg tds. On a follow-up visit three months later, the cervical nodes had markedly reduced in size, and the inguinal nodes were non-palpable and by six months the lymph nodes were no longer palpable but the patient still had the hyperpigmented maculo-papular rashes on the skin and was then referred to the dermatology clinic where the prednisolone dose was adjusted downward gradually to 5mg alternate day over a period of three weeks. Patient also received tablets Dapsone, Erythromycin (tablets and cream), flucloxacillin, Mupiderm, cream Retin A, Mary Kay acne gel. On further follow-up visit 18 months later, patient’s general condition was satisfactory, the nodal and skin lesions had completely resolved.
Photomicrograph of case 2 lymph node showing many histiocytes with several intact lymphocytes within their cytoplasm (emperipolesis) (short arrows) (H&E, 400X).
Case 3
A seven-year-old male presented with a two year history of recurrent right neck swelling which progressively increased in size over time. The swelling was painless, not associated with fever, cough, drenching night sweats, difficulty in swallowing and anorexia but with weight loss. There was no history of blood transfusion, surgery, hospital admissions or family history of similar illness.
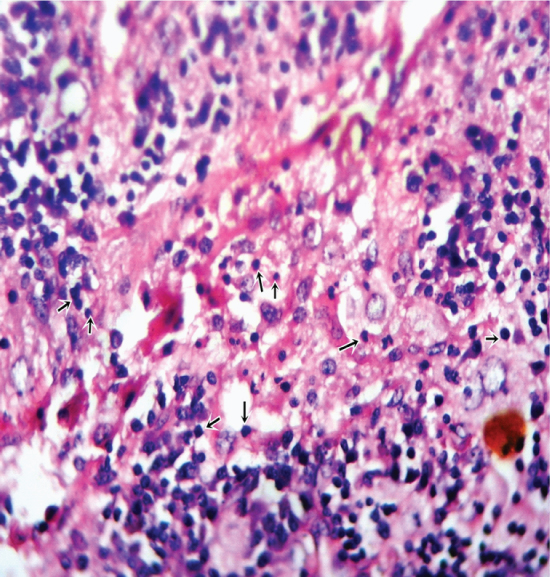
Clinical examination revealed a male child, afebrile, not pale, anicteric, not cyanosed, not dehydrated, but had significant lymphadenopathy involving the submental (7cm x 6cm), cervical (12cm x 6cm), axillary and inguinal lymph nodes. The largest nodes were located at the postero-inferior aspect of the right auricular area, extending to the posterior and anterior neck triangles. These matted nodular masses were firm, non-tender, not attached to overlying or underlying structures and with no associated skin lesions. The respiratory rate was 20 breaths/minute, pulse rate-80 beats/minute, and the liver and spleen were non-palpable. An impression of Non Hodgkin’s lymphoma was made to rule out Tuberculous lymphadenitis and Rhabdomyosarcoma and patient had an excisional cervical lymph node biopsy. The initial laboratory investigations were: Hb-9.8 g/dL; PCV-31%; Total WBC - 2.5x109/L units (N - 63%, L - 36%, M - 01%); Platelets - 150x109/L units, ESR - 65mm 1st hour; negative HIV I & 2 antibodies, mantoux – negative, fasting blood sugar level- 89mg/dl. SEUCr, CXR and abdominal ultrasonography were unremarkable [Table/Fig-2]. The gross examination of the excision cervical lymph biopsy showed a circumscribed tissue measuring 3x1.5x1 cm with solid, yellowish cut surface. The microscopic examination showed pronounced enlargement of the sinuses populated by histiocytes with large vesicular nucleus and abundant clear cytoplasm, some of which demonstrate emperipolesis [Table/Fig-5]. A histopathological diagnosis of Rosai-Dorfman disease was made and the patient was subsequently placed on tab prednisolone 5mg bd and tab vitamin C 100mg tds daily and discharged. Patient subsequently developed rashes all over his body and prednisolone was temporarily stopped five months after initial commencement of treatment, but on a further follow-up visit two months later, the neck swellings had markedly reduced in size and the rashes had disappeared. He was lost to follow-up one year after presentation.
Photomicrograph of case 3 lymph node showing many histiocytes with several intact lymphocytes within their cytoplasm (emperipolesis) (short arrows) (H&E, 400X).
Discussion
RDD or SHML is a rare histiocytic disorder of unknown aetiology that was first described by Rosai and Dorfman over four decades ago [1,2]. Though it is an idiopathic disease, the presence of occasional cytoplasmic inclusions, nuclear changes and identification of human herpes virus 6 and Epstein-Barr virus in visceral and cutaneous lesions have led some researchers to explore and suggest possible viral aetiology [3,4]. RDD is a benign, self-limiting disease of phagocytic histiocytes presenting mainly as massive painless bilateral cervical lymphadenopathy with a male predominance in the first and second decades of life [5-8]. It has a variable clinical presentation occurring with nodal and extra-nodal manifestations with periods of exacerbations and remissions, and a highly variable treatment response [7]. Though lymphadenopathy is the main clinical presentation, extranodal involvements have been reported in 43% of cases [9] with the skin being the most common extranodal manifestation, presenting as single papules, multiple nodules and plaques [9-11]. The involvement of unusual regions such as the breast, kidney, thyroid, testis, and central nervous system has also been reported [12-16].
Diagnosis of RDD is based on the histological identification of proliferating histiocytes with abundant pale cytoplasm, pericapsular fibrosis, and dilated sinuses in the lymph nodes. The presence of the phenomenon of emperipolesis, in which different types of blood cells, such as lymphocytes or neutrophils, exist in the cytoplasm of histiocytes with a background of mature lymphocytes and plasma cells is the hallmark of RDD [4,6,17]. However this finding is not specific to RDD and has also been described in haematological disorders such as idiopathic myelofibrosis and in tumor cells [18,19]. Immunohistochemical techniques demonstrating positivity for S-100 protein and CD68, and negativity for CD 1a [4], have also been used in diagnosing RDD especially in extranodal sites [9,20,21]. However, a prudent search of literature show reports of only few cases of RDD in Nigeria with no attempt at clinicopathological correlation.
All the three index cases managed and presented in this report were males, aged within the range 5-14 years and presented with painless bilateral cervical lymphadenopathy. These findings have been reported in previous studies [5-8]. In addition to the presentation of massive painless bilateral cervical lymphadenopathy in our RDD cases, there were other lymph node enlargements which included submental, submandibular, axillary, preauricular and inguinal lymph nodes.
Though extranodal involvements have been reported in 43% of RDD cases [9] with the skin being the most common extranodal site affected [9-11] occurring in about 10% of cases [22,23], two of our patients (2/3) had extranodular manifestations of ocular and cutaneous RDD, while one (1/3) did not have any extranodular involvement. Though involvement of breast, kidney, thyroid, testis, and central nervous system by RDD have been documented in previous studies [12-16], current cases did not present with any kidney, spleen or liver involvements.
RDD is commonly associated with systemic symptoms, such as: fever; weight loss; night sweats; leukocytosis with neutrophilia; polyclonal gammopathy and increased Erythrocyte Sedimentation Rate (ESR) [24,25], only one of our patients had a low-grade fever, while two had weight loss, and all three had mild anemia, and increased ESR. Also, though all three patients had a normal white blood cell count, they all had a relative neutrophilia which has been previously demonstrated [24,25].
Present cases also had a varied duration of illness before presentation ranging from 3 months to 2 years. These findings are also in agreement with the reported varied presentations of RDD [7]. The initial provisional diagnoses of our cases varied from lymphoreticular malignancies; Acute Myeloid Leukaemia (AML), Hodgkin’s lymphoma to NonHodgkin’s lymphoma. Other differential diagnoses considered were: viral syndromes (Infectious mononucleosis), other childhood malignancies (Neuroblastoma and Rhabdomyosarcoma), and chronic granulomatous disorders (Tuberculous lymphadenitis and Sarcoidosis). These differentials of RDD have also been described by other researchers [9,26,27] and thus, a high index of suspicion for RDD is required when diagnosing lymphoreticular lesions.
Though all three of our patients were mildly anemic at presentation, there were no other remarkable haematological or biochemical alterations and they were all negative to both Mantoux test, and HIV I & 2 antibodies. There were no radiological or ultrasonographical abnormalities. The diagnoses of RDD in our cases were made histologically on excision cervical lymph node biopsies. This in agreement with other studies [9-16]. Though there are recent reports of diagnosis by immunohistochemical techniques [20,21,28], due to the absence of immunohistochemical facility in our center, we could not immunologically demonstrate the presence of RDD cells as is being done in other developed [20,21] and some developing countries [9,28].
The treatment of RDD is dependent on the clinical presentation with different therapeutic modalities which include corticosteroids, thalidomide, interferon, surgery, cryotherapy, radiotherapy and chemotherapy [4,26,29,30]. Prednisolone was the main therapy given to our patients who came from low socioeconomic communities and could not afford the newer and more expensive modalities of treatment. Our patients’ response to treatment was however in agreement with reports from other centers where newer and more expensive drugs with induced rapid remission and better aesthetic results have been used [20,30]. With the commencement of treatment, an initial response of reduced size of lesions were observed within five months, three months, seven months in all three cases, giving an average initial response period of five months. This is also similar to the initial response time reported by other authors [20,26], but was marred by the appearance of complications which included mainly skin rashes, cushingoid facies and fungal infections (Tinea capitis). These complications were treated by either replacement of prednisolone with methylprednisolone for Cushing’s facies, or by reducing or briefly stopping prednisolone. Varied outcomes were observed in our cases over a therapy period of 2 years, 1 1/2 years and 1 year respectively, with relapse observed in case 1, full recovery in case 2 and partial recovery in case 3, who was lost to follow-up 1 year after commencement of therapy.
Conclusion
RDD remains a rare but significant cause of massive lymphadenopathy within the pediatric age group, presenting with unique clinicopathological features. Prompt and accurate histological diagnosis and prednisolone therapy would reduce the significant morbidity associated with this condition, even in low socioeconomic settings of developing countries.
CHOP: Children Out Patient;
Hb: hemoHaemoglobin Concentration; PCV: Packed Cell Volume, ESR: Erythrocyte Sedimentation Rate, Total WBC: Total White Blood Cell Count; N: Neutrophils; L: Lymphocytes; E: Eosinophils; M: Monocytes; Seucr: Serum Electrolyte Urea; Creatinine Concentration
[1]. Rosai J, Dorfman RF, Sinus histiocytosis with massive lymphadenopathy: a newly recognized benign clinicopathological entityArch Pathol 1969 87:63-70. [Google Scholar]
[2]. Sardana D, Goyal A, Gauba K, Sinus histiocytosis with massive lymphadenopathy: a “massive” misnomerDiagn Cytopathol 2015 43:315-19.10.1002/dc.2319825088489 [Google Scholar] [CrossRef] [PubMed]
[3]. Al-Daraji W, Anandan A, Klassen-Fischer M, Auerbach A, Marwaha JS, Fanburg-Smith JC, Soft tissue Rosai-Dorfman disease: 29 new lesions in 18 patients, with detection of polyomavirus antigen in 3 abdominal casesAnn Diagn Pathol 2010 14:309-16.10.1016/j.anndiagpath.2010.05.00620850691 [Google Scholar] [CrossRef] [PubMed]
[4]. Becker M, Gaiser T, Middel P, Rompel R, Clinicopathologic challenge. Destombes-Rosai-Dorfman disease (DRDD) (sinushistiocytosis with massive lymphadenopathy)Int J Dermatol 2008 47:125-27.10.1111/j.1365-4632.2008.03376.x18211480 [Google Scholar] [CrossRef] [PubMed]
[5]. Bist SS, Varshney S, Bisht M, Pathak VP, Kusum A, Gupta N, Rosai Dorfman syndrome - A rare clinical entityIndian J Otolaryngol Head Neck Surg 2007 59:184-86.10.1007/s12070-007-0056-823120428 [Google Scholar] [CrossRef] [PubMed]
[6]. Maia RC, de Meis E, Romano S, Dobbin JA, Klumb CE, Rosai-Dorfman disease: a report of eight cases in a tertiary care center and a review of the literatureBraz J Med Biol Res 2015 48(1):06-12.10.1590/1414-431x2014411025493377 [Google Scholar] [CrossRef] [PubMed]
[7]. Warpe BM, More SV, Rosai- Dorfman disease: A rare clinico-pathological presentationAMJ 2014 2:68-72.10.4066/AMJ.2014.193124611075 [Google Scholar] [CrossRef] [PubMed]
[8]. Kushwaha R, Ahluwalia C, Sipayya V, Diagnosis of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman Disease) by fine needle aspiration cytologyJ Cytol 2009 262:3-5.10.4103/0970-9371.5522921938160 [Google Scholar] [CrossRef] [PubMed]
[9]. Leal PAB, Adriano AL, Breckenfeld MP, Costa IS, de Sousa ARD, Gonçalves H, de S, Rosai-Dorfman disease presenting with extensive cutaneous manifestation - Case reportAnais Brasileiros de Dermatologia 2013 88(2):56-259.10.1590/S0365-0596201300020001423739703 [Google Scholar] [CrossRef] [PubMed]
[10]. Wang KH, Chen WY, Liu HN, Huang CC, Lee WR, Hu CH, Cutaneous Rosai-Dorfman disease: clinicopathological profiles, spectrum and evolution of 21 lesions in six patientsBr J Dermatol 2006 154:277-86.10.1111/j.1365-2133.2005.06917.x16433797 [Google Scholar] [CrossRef] [PubMed]
[11]. Pitamber HV, Grayson W, Five case of cutaneous Rosai-Dorfman diseaseClin Exp Dermatol 2003 28:17-21.10.1046/j.1365-2230.2003.01195.x12558621 [Google Scholar] [CrossRef] [PubMed]
[12]. Green I, Dorfman RF, Rosai J, Breast involvement by extranodal Rosai-Dorfman disease: report of seven casesAm J Surg Pathol 1997 21:664-68.10.1097/00000478-199706000-000069199644 [Google Scholar] [CrossRef] [PubMed]
[13]. Abdollahi A, Ardalan FA, Ayati M, Extranodal Rosai-Dorfman disease of the kidneyAnn Saudi Med 2009 29:55-57.10.4103/0256-4947.5182319139612 [Google Scholar] [CrossRef] [PubMed]
[14]. Chhabra S, Agarwal R, Garg S, Singh H, Singh S, Extra-nodal Rosai-Dorfman disease: a case report with thyroid involvementDiagn Cytopathol 2012 40:447-49.10.1002/dc.2173721630484 [Google Scholar] [CrossRef] [PubMed]
[15]. Del Gobbo A, Moltrasio F, Young RH, Rosai J, Involvement of the testis and related structures by Rosai-Dorfman disease: report of 2 new cases and review of the literatureAm J Surg Pathol 2013 37:1871-75.10.1097/PAS.0b013e31829e250924061526 [Google Scholar] [CrossRef] [PubMed]
[16]. Beros V, Houra K, Rotim K, Zivkovic DJ, Cupic H, Kosec A, Isolated cerebellar intraparenchymal Rosai-Dorfman disease - case report and review of literatureBr J Neurosurg 2011 25:292-96.10.3109/02688697.2010.54689921344967 [Google Scholar] [CrossRef] [PubMed]
[17]. Pradhananga RB, Dangol K, Shrestha A, Baskota DK, Sinus histiocytosis with massive lymphadenopathy (rosai-dorfman disease): a case report and literature reviewInternational Archives of Otorhinolaryngology 2014 18(44):06-408.10.1055/s-0034-138716325992132 [Google Scholar] [CrossRef] [PubMed]
[18]. Schmitt A, Jouault H, Guichard J, Wendling F, Drouin A, Cramer EM, Pathologic interaction between megakaryocytes and polymorphonuclear leukocytes in myelofibrosisBlood 2000 96:1342-47. [Google Scholar]
[19]. Singhal N, Handa U, Bansal C, Mohan H, Neutrophil phagocytosis by tumor cells - a cytological studyDiagn Cytopathol 2011 39:553-55.10.1002/dc.2142120949458 [Google Scholar] [CrossRef] [PubMed]
[20]. Sandoval-Sus JD, Sandoval-Leon AC, Chapman JR, Velazquez-Vega J, Borja MJ, Rosenberg S, Rosai-Dorfman disease of the central nervous system: report of 6 cases and review of the literatureMedicine 2014 93(13):65-175.10.1097/MD.000000000000003024797172 [Google Scholar] [CrossRef] [PubMed]
[21]. Vuong V, Moulonguet I, Cordoliani F, Crickx B, Bezier M, Vignon-Pennamen Cutaneous revelation of Rosai-Dorfman disease: 7 casesAnn Dermatol Venereol 2013 140:83-90.10.1016/j.annder.2012.06.03623395488 [Google Scholar] [CrossRef] [PubMed]
[22]. Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, Fitzpatricks’s Dermatology in general medicine 2014 8th edNew YorkMcGraw-Hill [Google Scholar]
[23]. Kutlubay Z, Bairamov O, Sevim A, Demirkesen C, Mat MC, Rosai-Dorfman disease a case report with nodal and cutaneous involvement and review of the literatureAm J Dermatopathol 2014 36:353-57.10.1097/DAD.0b013e31829e556423863552 [Google Scholar] [CrossRef] [PubMed]
[24]. Rizwan MM, Chhabra G, Mishra A, Kapadia S, Rai R, Gill H, A case of isolated cutaneous Rosai-Dorfman-SyndromeGulf J Oncolog 2013 1:87-89. [Google Scholar]
[25]. Chang LY, Kou T, Chan HL, Extranodal Rosai-Dorfman disease with cutaneous, ophthalmic and laryngeal involvement: report of a case treated with isotretinoinInt J Dermatol 2002 41:888-91.10.1046/j.1365-4362.2002.01675.x12492979 [Google Scholar] [CrossRef] [PubMed]
[26]. Gameiro A, Gouveia M, Cardoso JC, Tellechea O, Histological variability and the importance of clinicopathological correlation in cutaneous Rosai-Dorfman diseaseAnais Brasileiros de Dermatologia 2016 91(65):34-637.10.1590/abd1806-4841.2016447727828638 [Google Scholar] [CrossRef] [PubMed]
[27]. Maheshwari R, Shekde S, Extranodal Rosai-Dorfman Disease presenting as an isolated epibulbar massIndian Journal of Ophthalmology 2008 56(6):02-504.10.4103/0301-4738.4337218974523 [Google Scholar] [CrossRef] [PubMed]
[28]. Agarwal A, Pathak S, Gujral S, Sinus histiocytosis with massive lymphadenopathy--a review of seven casesIndian J Pathol Microbiol 2006 49(4):509-15. [Google Scholar]
[29]. Chan CC, Chu CY, Dapsone as a potential treatment for cultaneous Rosai-Dorfman disease with neutrophilic predominanceArch Dermatol 2006 142:428-30.10.1001/archderm.142.4.42816618860 [Google Scholar] [CrossRef] [PubMed]
[30]. Dalia S, Sagatys E, Sokol L, Kubal T, Rosai-Dorfman disease tumor biology, clinical features, pathology, and treatmentCancer Control 2014 21:322-27.10.1177/10732748140210040825310213 [Google Scholar] [CrossRef] [PubMed]