Comparison of Microleakage and Shear Bond Strength (SBS) of Dyad Flow and Tetric Flow in Primary Molars: An In-vitro Study
Ramya Chowdary Mandava1, Deepa Gurunathan2, Mahesh Ramakrishnan3, EMG Subramanian4
1 Student Department of Pediatric and Preventive Dentistry, Saveetha Dental College, Saveetha University, Velappanchavadi, Chennai, Tamil Nadu, India.
2 Reader, Department of Pediatric and Preventive Dentistry, Saveetha Dental College, Saveetha University, Velappanchavadi, Chennai, Tamil Nadu, India.
3 Sr Lecturer, Department of Pediatric and Preventive Dentistry, Saveetha Dental College, Saveetha University, Velappanchavadi, Chennai, Tamil Nadu, India.
4 Head of Department, Department of Pediatric and Preventive Dentistry, Saveetha Dental College, Saveetha University, Velappanchavadi, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ramya Chowdary Mandava, #401, Sri Lakshmi Nilayam, D D Colony, Lane no 3, Bagh Amberpet, Opp Hotel Management College, Hyderabad -500013, Telangana, India.
E-mail: drramya_pedo@yahoo.com
Introduction
Early diagnosis combined with conservative adhesive treatment of occlusal caries may preserve the integrity of the remaining tooth and increase its longevity.
Aim
To compare microleakage and Shear Bond Strength (SBS) of Dyad flow and Tetric flow in primary molars.
Materials and Methods
Microleakage test: Eighteen samples were utilised separately for SBS and Microleakage. Standard Class I tooth cavity were prepared on occlusal surface of all teeth. The samples of Group 1 group were restored with Dyad flow restorative material; Samples of Group 2 were restored with Tetric flow and subjected to thermocycling in customized thermocycling device. Further, the samples were soaked in freshly prepared 2% Rhodamine B dye solution for 24 hours. The samples were then sectioned in bucco-lingual direction with hard tissue microtome under constant water flow and were observed under confocal microscope at 4× magnification and evaluated for die penetration. Eight out of nine samples were graded III, where as the other sample was graded as II based on ISO microleakage scoring system.
Shear Bond Strength Test: A 2 mm high cylindrical polyethylene tube with an internal diameter of approximately 2 mm was placed on the dentin surface of each specimen. No etching or bonding was done for samples of Group 1 (Dyad flow), Optibond bonding agent was applied to the prepared buccal surface of the specimens in group 2 (Tetric Flow) and cured for 20 seconds. Flowable resin composite was injected into the tube and polymerized for 40 seconds using an LED curing unit. All specimens were subjected to thermocycling from 5°C and 55°C for 500 cycles. SBS testing was done following thermocycling. Specimens were secured in the holder of a universal testing machine and sheared with a knife-edge blade at a crosshead speed of 1.0 mm/minute. Independent t-test was performed for statistical significance.
Results
Microleakage Test: There was no significant difference in microleakage between Dyad Flow and Tetric flow (p<0.05). Inter-examiner reliability was done between the accessors and the probability was 0.65 and 0.73.
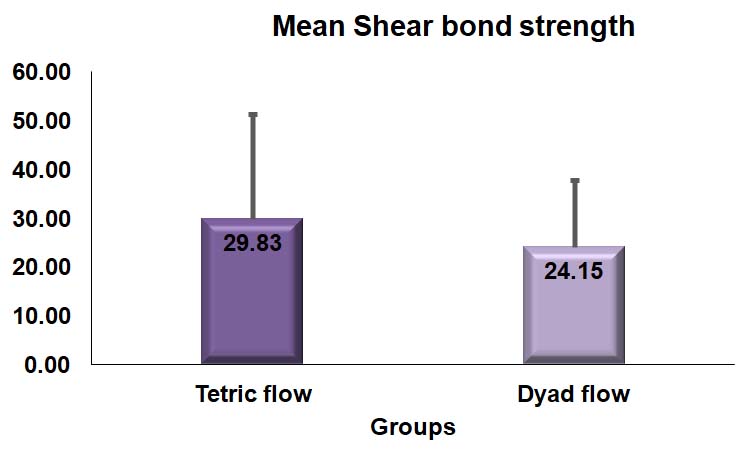
Shear bond strength test: No statistical significance was observed between the groups (p=0.51). The highest mean SBS value was recorded for group 2 in Tetric flow (29.83±21.4 MPa), whereas the lowest value was recorded for group 1 in Dyad flow (24.15±3.5 MPa).
Conclusion
Dyad flow and Tetric flow had similar microleakage. Whereas, Mean SBS of Dyad flow was lower than Tetric flow. With the results of this study, Dyad flow can be used for class I cavities of primary molars.
Conventional flowable composite, Primary Molars, Self adhesive flowable composite, Shear bond strength, Microleakage
Introduction
Proper diagnosis of occlusal caries, when treated with conservative adhesive treatment preserves the integrity of the existing tooth thus increasing its longevity. Two major advances in aesthetic restorative dentistry are composites and acid-etch technique. When used as a posterior restorative material they had several limitations in strength, dimensional stability and wear resistance which lead to the restoration failure, subsequently causing secondary caries and loss of anatomic form [1,2].
Even though there is an improvement over the years in the wear resistance and strength of posterior restorative materials, the problem of polymerisation shrinkage still remained, with the use of composites [3,4]. Contraction of resin during curing results in polyerisation shrinkage, inducing internal and interfacial stresses at the tooth restoration interface, leading to marginal leakage [4,5]. Because of the belief that Flowable composites are minimally invasive, and requires less sound tooth removal than amalgam restorations, they are used widely for Class I restorations [6,7]. The commonly used dental restoratives in paediatric dentistry today are glass ionomer cements, compomers, and resin composites [8-10]. These materials are suitable for conservative cavity preparations of tooth cavities. Since child compliance is often a limiting factor, a desirable property of a dental restorative should have good handling characteristics in the sense of a smooth application technique, which is more valid for resin-modified glass ionomer cement which, together with compomer, is the most commonly used restorative material in primary teeth [1,11]. An ideal posterior filling material should possess properties like aesthetics, high resistance to clinical wear, permanent marginal integrity, minimum cavity preparation, radiopacity, easy manipulation and nontoxicity. Posterior composite resins can fulfil most of these properties. One of the most significant problems associated with use of posterior composite as restorative material is the predisposition for marginal leakage, due to polymerization shrinkage and thermal expansion [2,7,8,10].
As bonding to dentin is more difficult than to enamel, dentin bonding agents are used to improve the marginal seal of resin composite restoration at the composites and tooth interface [12]. They have proven to be effective at reducing but not eliminating the microleakage [13]. Flowable composites have recently been used as a initial thin liner under composites resulting as a stress breaker [1,12]. Microleakage leads to marginal permeability to bacterial, chemical or molecular invasion at the interface between the tooth and the restoration. Marginal leakage of such restoration may lead to hypersensitivity, staining and discolouration, secondary caries and eventually pulpal irritation. Checking the depth of dye penetration under stereo microscope is the most common method used for estimating the microleakage of the materials [9].
Multiple studies which compared the bond strengths of adhesive systems to permanent and primary dentin, showed contradictory results [13,14]. Results of some studies showed lower bond strength in primary dentin [14], others resulted with either similar or even superior performance of the adhesive systems in primary dentin [14]. In this era with evolution of Self-adhesive flowable composites, restoration of permant teeth have become easier and time saving. To utilise the advantages of the same, this study aimed at evaluating the shear bond strength using universal testing machine and microleakage under confocal microscope of single step self-adhesive flowable composite with a gold standard three-step etch-rinse-cure flowable composite.
Materials and Methods
The study was carried out after Scientific Review Board protocol approval from University Scientific Review Board committee (SRB/SDMDS13PED3). It was conducted as a collaborative effort involving Department of Pedodontics and CIPET (Central institute of plastic engineering technology, Chennai) from period of February 2015 to May 2015.
Extraction was performed in children who attended the out-patient clinic, Department of Paediatric and Preventive Dentistry, Saveetha Dental college, Chennai.
Independent t-test was done to calculate the sample size keeping the power 90% attaining 8 samples for each group. To attain more accuracy and reduce damage of sample during the process, each group contained 9 samples in the current study, keeping 18 separate samples for microleakage and 18 separate samples for shear bond strength.
Tooth Selection Criteria:
Caries free sound maxillary and mandibular 1st primary molars obtained following serial extraction done during orthodontic treatment
Caries free sound teeth extracted due to pre-shedding mobility:
Maxillary 1st primary molars
Maxillary 2nd primary molars
Mandibular 1st primary molars
Mandibular 2nd primary molars
Following extraction, teeth were cleaned with scalers and stored in formalin for one week, following which they were transferred to saline solution at room temperature for three months prior to the experiment to maintain hydration of tooth structure [15-18].
Materials and Methods
Two commercially available flowable composites: Dyad Flow (Kerr Dental, Orange, CA, USA Lot No: 5123563; and Tetric flow; Ivoclar Vivadent India Lot No: U10940), 37% phosphoric acid gel (Scotchbond Multipurpose, 3M/ESPE, USA Lot No: EG 00415) and one adhesive (Opti Bond All-In-One; Kerr Dental, Orange, CA, USA Lot No: 0197) were used in this study. All materials were applied according to the manufacturer’s instructions.
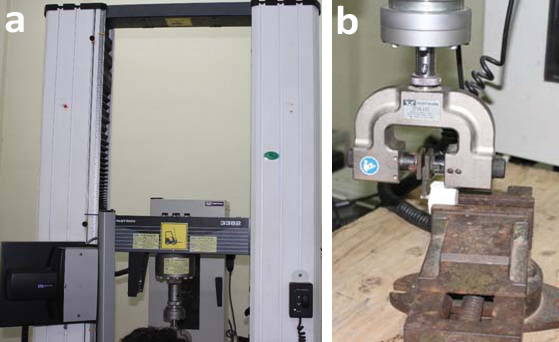
Shear Bond Strength Test: Specimens were embedded in plaster of Paris in cylindrical rubber molds, with the buccal bonding site facing the bottom of the mold. To obtain uniform smear layers, dentin surfaces were ground with 600-grit silicon carbide paper. To maintain hydration, dentin specimens were placed in a box containing water and stored in an incubator at 37°C for 24 hours before application of bonding agent. Primary tooth specimens were randomly divided into 2 groups with 9 specimens each, as follows: Group 1: Dyad Flow (single step technique); Group 2: Tetric flow (three step technique). A 2-mm-high cylindrical polyethylene tube with an internal diameter of approximately 2 mm was placed on the dentin surface of each specimen. Optibond bonding agent was applied to prepared buccal surface of specimens in group 2 and cured for 20 seconds. Flowable resin composite was injected into the tube and polymerized for 40 seconds using an LED curing unit (Elipar Free Light II; 3M/ ESPE, St. Paul, MN, USA; light intensity: 1,000 mW/cm2) [Table/Fig-1].
Samples of shear bond strength test.

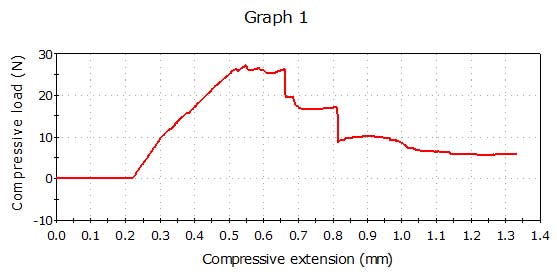
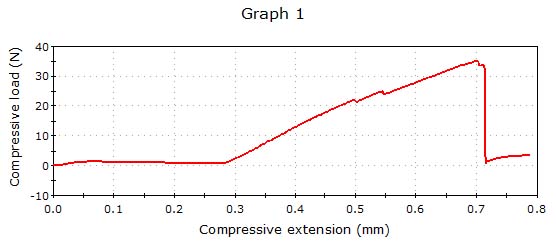
Specimens were then stored in 100% relative humidity at 37°C for 24 hours. Tubes were removed with a sharp blade. Specimens were then thermocycled (ENVIROTRONICS C 1500) between 5°C and 55°C for 500 cycles using a dwell time of 10 seconds and a transfer time of 30 seconds between each bath [Table/Fig-2] [19-21]. SBS testing following thermocycling, specimens were secured in the holder of a universal testing machine (Lloyd LRX; Lloyd Instruments, Fareham, Hants, UK) and sheared with a knife-edge blade at a crosshead speed of 1.0 mm/min [Table/Fig-3a,b]. Shear Bond Strength was calculated in Megapascals (MPa) by dividing the peak load at failure of restoration with the specimen surface area [Table/Fig-4a,b]. The Normality test and the Kolmogorov-Smirnov results show that the variable follows Normal distribution. Therefore, to analyse the data parametric tests were used. To compare mean values between groups independent t-test was applied, version 12.0.1 (SPSS Inc, Chicago, IL, USA).
Samples in thermocycling process.

a) Universal testing machine; b) Shear stress application on sample.
Compressive load applied on Group 1 (Dyad flow) sample till failure.
Compressive load applied on group 2 (Tetric Group) sample till failure.
Microleakage Test: Standard Class I cavity was prepared on occlusal surfaces of all the teeth. The dimensions of occlusal box preparation with pulpal depth of 3 mm, bucco-lingual width of 3 mm, and mesio-distal width of 4 mm and mounted on round acrylic blocks.
After the cavity preparation etching was done by application of 37% phosphoric acid gel (Scotchbond Multipurpose, 3M/ESPE, USA) for 15 seconds. It was rinsed with water for 10 seconds. After removal of excess water with moist cotton pellet, bonding agent (OptiBond All-In-One, Kerr Dental, Orange, CA, USA) was applied as per manufacturer’s directions and light cured for 10 seconds with light curing unit (Unicorn Denmart, India). Placement of composite was done in incremental manner along the walls to avoid air bubbles and for complete curing. Tefflon coated instruments (GDC plastic filling instrument #1) were used to standardise the technique for incremental build-up. It was placed in contact with the wall to standardize the space for incremental build-up. The increment was then adapted and light cured for 40 seconds. Horizontal increments were placed to fill the remaining preparation and light cured for 40 seconds. Further, finishing and polishing of occlusal surfaces were done with sof-lex discs and strips (3M/ESPE, USA) in sequential manner as per manufacturer’s instructions.
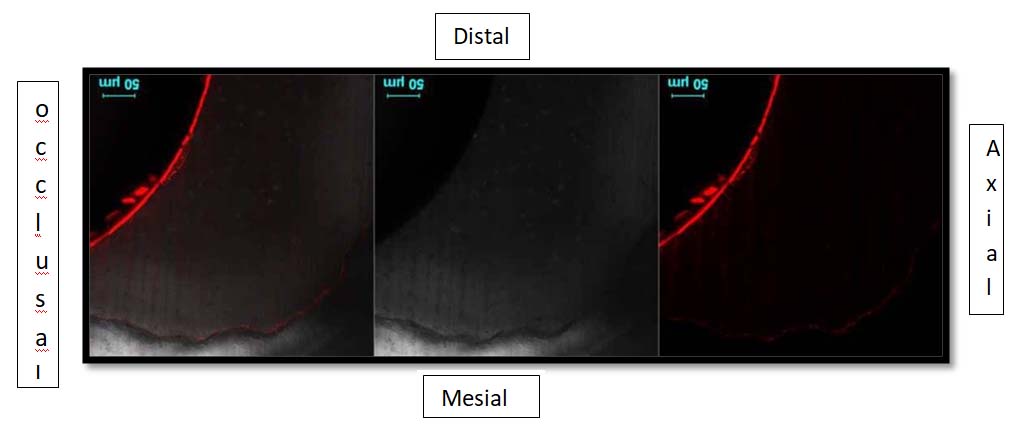
Dye penetration test: The samples were subjected to thermocycling in customized thermocycling device (ENVIROTRONICS C 1500) which worked at 500 cycles at 5°C, 37°C, and 55°C, with a dwell time of 30 seconds and transfer time of 15 seconds [Table/Fig-2] [19-21]. The apices were then sealed with modelling wax and two coats of nail varnish were applied over the entire sample surface except for the restoration and 1 mm area beyond the margins. Further, the samples were soaked in freshly prepared 2% Rhodamine B dye solution for 24 hours after which they were thoroughly rinsed under tap water. The samples were then sectioned in bucco-lingual direction from center of the restorations with hard tissue microtome under constant water flow. The sectioned teeth were observed under confocal microscope (KEISS LSM S10 META) at 4X magnification and evaluated using the ISO microleakage scoring system (ISO/TS 11405:2003) [Table/Fig-5a,b,c and d] [22-25]. The ISO scoring criteria for occlusal microleakage scores was as follows:
Sample of dyad flow group under confocal microscope with grade III microleakage.
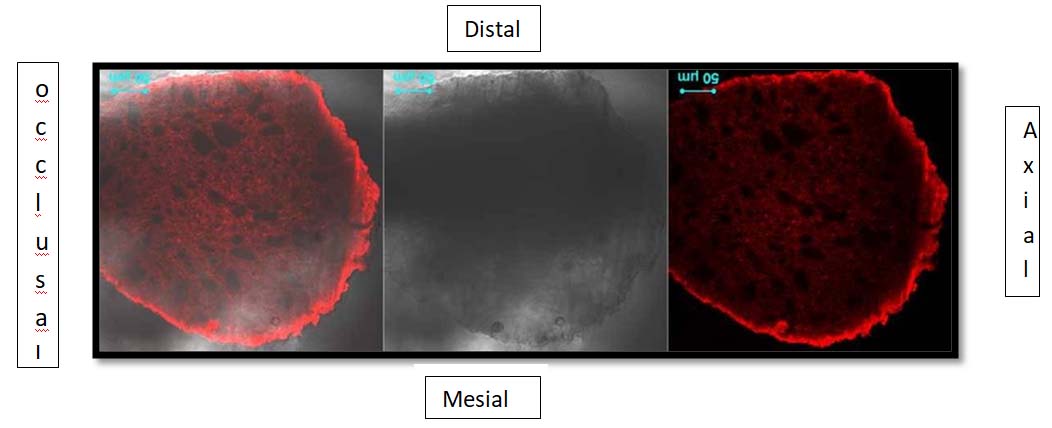
Sample of dyad flow group under confocal microscope with grade II microleakage.
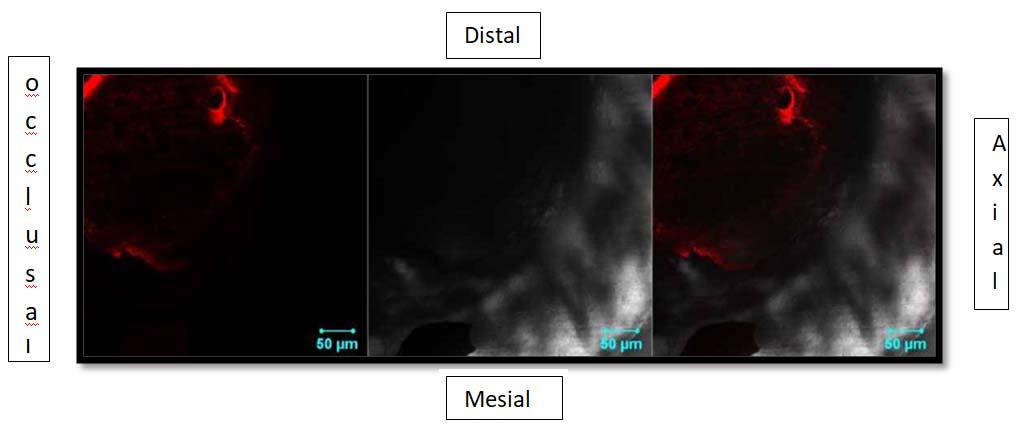
Sample of tetric flow group under confocal microscope with grade II Microleakage.
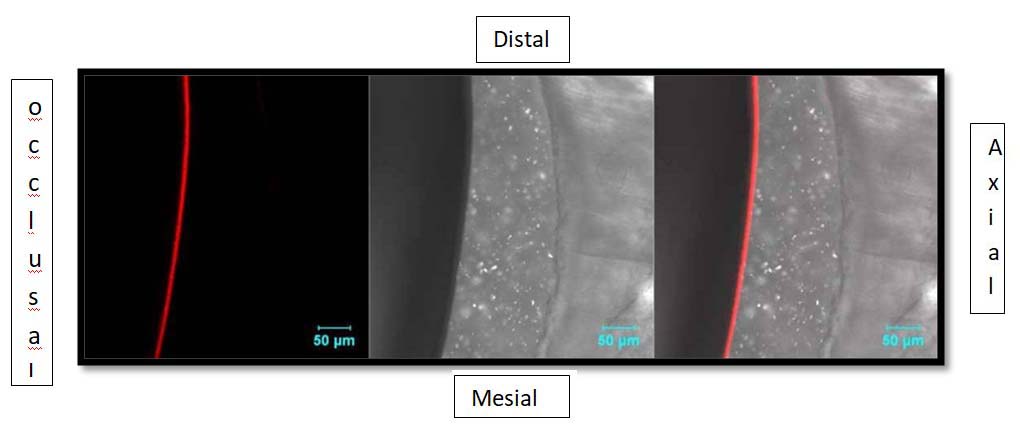
Sample of tetric flow group under confocal microscope with grade III microleakage.
0 = No dye penetration
1 = Dye penetration into enamel
2 = Dye penetration into the dentin, not including the pulpal wall/gingival floor
3 = Dye penetration into the dentin including the pulpal wall
The degree of dye penetration was independently scored [15]. In case of disagreement or doubt of evaluations, the least score was considered.
Kappa statistics performed to assess inter-examiner reliability.
Results
Shear Bond Strength: The mean Shear Bond Strength (SBS) values for the experimental and control groups were tabulated in [Table/Fig-6] and shown in [Table/Fig-7]. The mean SBS of specimens restored with Dyad Flow (single step technique) and Tetric flow (Three step techniques) was 24.15 and 29.83 respectively. There was no statistically significant difference in the SBS between the two groups (p>0.05).
Descriptive sample size distribution with mean SBS.
| Group | N | Mean Shear bond strength | Std. Dev | t-Value | p-value |
|---|
| Dyad flow | 9 | 24.15 | 13.59 | 0.671 | 0.512 |
| Tetric flow | 9 | 29.83 | 21.45 |
Mean SBS of Dyad flow and tetric flow.
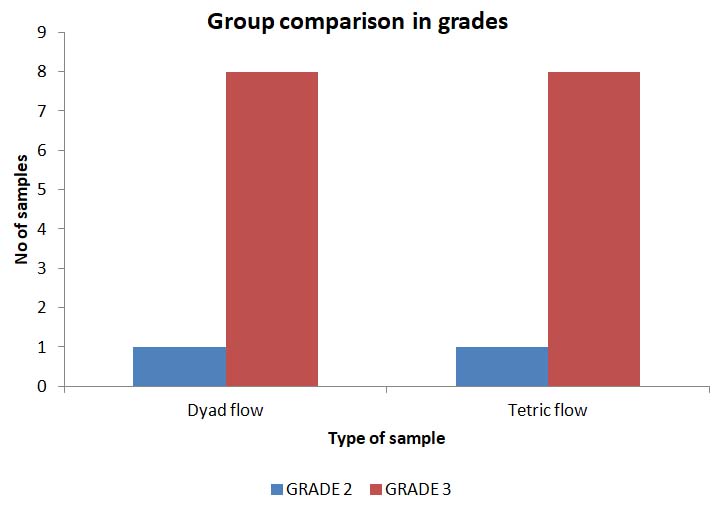
Micro Leakage: Statistical results of the Mann-Whitney test for microleakage score of the groups are shown in [Table/Fig-8,9]. Among nine samples of each group, one sample was graded II and the remaining were graded III. There was no significant difference in microleakage between Dyad flow (single step technique) and Tetric flow (three step technique) (p>0.05). Inter-examiner reliability was done between the assessors and the probability was 0.65 and 0.73. Substantial agreement was achieved through Kappa statistics.
Microleakage score of Dyad flow and tetric flow.
| Dyad flow | Tetric flow |
|---|
| GRADE 2 | 1 | 1 |
| GRADE 3 | 8 | 8 |
Microleakage score of each group.
Discussion
The major drawback in an adhesive restoration is the lack of suitable adhesion to the tooth structure and microleakage between the tooth and the filling material. This study was designed to compare the shear bond strength and microleakage of a self-adhesive flowable composite with traditional three step flowable composite in class I cavities of primary molars when used as a filling material done in in-vitro conditions.
This study was directed towards comparing the gold standard technique (three step technique) with the self-etch adhesives technique, which showed lower shear bond strength of Dyad flow than Tetric flow but with similar microleakage between the two groups. Thus, the null hypothesis has to be accepted.
The Shear Bond Strength of a self-etch adhesive flowable composite to enamel and dentin of permanent teeth concluded that self-etch adhesive had lower bond strength than the conventional technique [26]. Additional etching of the tooth substance with phosphoric acid didn’t improve the bond strength of the self-etch adhesive. Studies comparing single step to three step composite leads to lower bond strength for single step technique with varied bond strengths in permanent molars [20,27,28]. Self-etch adhesives have lower bond strength than conventional composite in permanent teeth [29,30]. A study conducted using self-etch adhering composite to three step composite concluded stronger bonding of self-etch adhesives with tight marginal seal when compared to three step technique on permanent dentin. Few voids in specimens restored with flowable composites appeared as tiny microscopic bubbles [31].
Thick hybrid layer in primary teeth which subsequently lacks complete penetration of adhesive resins into already demineralized dentin results in reduction of bond strength in primary dentin. To reproduce the higher bond strengths like permanent teeth, the dentin etching time should be shorter (50% less) or use of weaker concentrations should be considered for primary teeth. The decreased dentin permeability of primary teeth is caused by smaller tubule concentration and diameter. However, when the number of DBA coats is increased (without in between curing of layers), it leads to improving resin infiltration, subsequently producing greater shear bond strength to primary dentin [27,28,32-34].
Conclusion
Within the limitations of the study, it may be concluded that Dyad flow has lower bond strength with similar microleakage when compared with Tetric flow in class I cavities of primary molars. Dyad flow can be used as sealant, repairing enamel defects, liner of restorations and incisal abrasions. Further, clinical studies and developments in material technology are required to evaluate the clinical success of this new material which can change the time consuming restorative treatment in paediatric dentistry.
[1]. Attar N, Turgut MD, Gungor HC, The effect of flowable resin composites as gingival increments on the microleakage of posterior resin compositesOper Dent 2004 29(2):162-67. [Google Scholar]
[2]. Anusavice KJ, Phillips’ science of dental material 2003 1111th edSt.LouisElsevier:399-441.10.1016/S0262-1762(03)90281-1 [Google Scholar] [CrossRef]
[3]. Beznos C, Microleakage at the cervical margin of composite class II cavities with different restorative techniquesOper Dent 2001 26(1):60-69. [Google Scholar]
[4]. Burrow MF, Nopnakeepong U, Phrukkanon S, A comparison of microtensile bond strengths of several dentin bonding systems to primary and permanent dentinDent Mater 2002 18(3):239-45.10.1016/S0109-5641(01)00041-0 [Google Scholar] [CrossRef]
[5]. Kidd EA, Microleakage in relation to amalgam and composite restorations: A laboratory studyBr Dent J 1976 141(10):305-10.10.1038/sj.bdj.4803840826263 [Google Scholar] [CrossRef] [PubMed]
[6]. Welbury RR, Shaw AJ, Murray JJ, Gordon PH, McCabe JF, Clinical evaluation of paired compomer and glass ionomer restorations in primary molars: final results after 42 monthsBr Dent J 2000 189:93-97.10.1038/sj.bdj.480069310975160 [Google Scholar] [CrossRef] [PubMed]
[7]. Buerkle V, Kuehnisch J, Guelmann M, Hickel R, Restoration materials for primary molars results from a European surveyJ Dent 2005 33:275-81.10.1016/j.jdent.2004.08.00915781135 [Google Scholar] [CrossRef] [PubMed]
[8]. Andersson-Wenckert IE, van Dijken JWV, Stenberg R, Effect of cavity form on the durability of glass ionomer cement restorations in primary teeth: a three-year clinical evaluationASDC J Dent Child 1995 62(3):197-200. [Google Scholar]
[9]. Yazici AR, Celik C, Ozgünaltay G, Microleakage of different resin composite typesQuintessence Int 2004 35(10):790-94. [Google Scholar]
[10]. White JM, Eakle WS, Rationale and treatment approach in minimally invasive dentistryJ Am Dent Assoc 2000 131(6):13-19.10.14219/jada.archive.2000.039410860340 [Google Scholar] [CrossRef] [PubMed]
[11]. Kilpatrick NM, Murray JJ, McCabe JF, The use of a reinforced glass-ionomer cermet for the restoration of primary molars: a clinical trialBr Dent J 1995 179:175-79.10.1038/sj.bdj.48088677546970 [Google Scholar] [CrossRef] [PubMed]
[12]. Malmström HS, Schlueter M, Roach T, Moss ME, Effect of thickness of flowable resins on marginal leakage in class II composite restorationsOper Dent 2002 27(4):373-80. [Google Scholar]
[13]. Retief DH, Denys FR, Adhesion to enamel and dentinAm J Dent 1989 2(Spec No):133-44. [Google Scholar]
[14]. Hosoya Y, Nishiguchi M, Kashiwabara Y, Horiuchi A, Goto G, Comparison of two dentin adhesives to primary vs. permanent bovine dentinJ Clin Pediatr Dent 1997 22(1):69-76. [Google Scholar]
[15]. Kumar M, Sequeira P S, Peter S, Bhat G K, Sterilisation of extracted human teeth for educational useIndian J Med Microbiol 2005 23(4):256-58. [Google Scholar]
[16]. Sawani S, Arora V, Jaiswal S, Nikhil V, Shefali Comparative evaluation of microleakage in Class II restorations using open vs. closed centripetal build-up techniques with different lining materialsJ Conserv Dent 2014 17(4):344-48.10.4103/0972-0707.13645025125847 [Google Scholar] [CrossRef] [PubMed]
[17]. Lee J, Nettey-Marbell A, Cook A, Pimenta L, Leonard R, Ritter A, Using extracted teeth for researchJ Am Dent Assoc 2007 138(12):1599-603.10.14219/jada.archive.2007.011018056105 [Google Scholar] [CrossRef] [PubMed]
[18]. George S, Pichardo M, Bergeron B, Jeansonne B, The effect of formalin storage on the apical microleakage of obturated canalsJ Endod 2006 32(9):869-71.10.1016/j.joen.2006.04.00916934630 [Google Scholar] [CrossRef] [PubMed]
[19]. Rajbaran Sandeepa Dannheimer M, Wet F De, The effect of thermocycling on the determination of microleakage in permite amalgam restorations: scientificSADJ 2009 64(9):394-96. [Google Scholar]
[20]. Gale M, Darvell B, Thermal cycling procedures for laboratory testing of dental restorationsJ Dent 1999 27(2):89-99.10.1016/S0300-5712(98)00037-2 [Google Scholar] [CrossRef]
[21]. Alexandre R, Sundfeld R, Giannini M, Lovadino J, The Influence of Temperature of Three Adhesive Systems on Bonding to Ground EnamelOper Dent 2008 33(3):272-81.10.2341/07-7918505217 [Google Scholar] [CrossRef] [PubMed]
[22]. Bitter K, Paris S, Martus P, Schartner R, Kielbassa A, A confocal laser scanning microscope investigation of different dental adhesives bonded to root canal dentineInt Endod J 2004 37(12):840-48.10.1111/j.1365-2591.2004.00888.x15548275 [Google Scholar] [CrossRef] [PubMed]
[23]. Lopes M, Consani S, Gonini-Júnior A, Moura S, McCabe J, Comparison of microleakage in human and bovine substrates using confocal microscopyBull Tokyo Dent Coll 2009 50(3):111-16.10.2209/tdcpublication.50.11119887753 [Google Scholar] [CrossRef] [PubMed]
[24]. Kitayama S, Nasser N, Pilecki P, Wilson R, Nikaido T, Tagami J, Effect of resin coating and occlusal loading on microleakage of class II computer-aided design/computer-aided manufacturing fabricated ceramic restorations: A confocal microscopic studyActa Odontol Scand 2011 69(3):182-92.10.3109/00016357.2010.54950421231818 [Google Scholar] [CrossRef] [PubMed]
[25]. Grobler SR, Oberholzer TG, Rossouw RJ, Grobler-Rabie A, Van WykKotze TJ, Shear bond strength, microleakage, and confocal studies of 4 amalgam alloy bonding agentsQuintessence Int 2000 31(7):501-08. [Google Scholar]
[26]. Bonilla ED, Stevenson RG, Caputo AA, White SN, Microleakage resistance of minimally invasive Class I flowable composite restorationsOper Dent 2012 37(3):290-98.10.2341/11-106-L22313270 [Google Scholar] [CrossRef] [PubMed]
[27]. Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, Buonocore memorial lecture. Adhesion to enamel and dentin: Current status and future challengesOper Dent 2003 28:215-35. [Google Scholar]
[28]. Vichi A, Margvelashvili M, Goracci C, Papacchini F, Ferrari M, Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorationsClin Oral Invest 2012 17(6):1497-506.10.1007/s00784-012-0846-623086332 [Google Scholar] [CrossRef] [PubMed]
[29]. Prabhakar AR, Madan M, Raju OS, The marginal seal of a flowable composite, an injectable resin modified glass ionomer and a compomer in primary molars--an in vitro studyJ Indian Soc Pedod Prev Dent 2003 21(2):45-48. [Google Scholar]
[30]. Morabito A, Defabianis P, The marginal seal of various restorative materials in primary molarsJ Clin Pediatr Dent 1997 22(1):51-54. [Google Scholar]
[31]. Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M, Ferrule effect: a literature reviewJ Endod 2012 38(1):11-19.10.1016/j.joen.2011.09.02422152612 [Google Scholar] [CrossRef] [PubMed]
[32]. Poitevin A, De Munck J, Van Ende A, Suyama Y, Mine A, Peumans M, Bonding effectiveness of self-adhesive composites to dentin and enamelDent Mater 2013 29(2):221-30.10.1016/j.dental.2012.10.00123107191 [Google Scholar] [CrossRef] [PubMed]
[33]. Scaminaci Russo D, Iuliano V, Franchi L, Ferrari M, Giachetti L, Adhesion to primary dentin: microshear bond strength and scanning electron microscopic observationAm J Dent 2013 26(6):341-46. [Google Scholar]
[34]. Arregui M, Giner L, Ferrari M, Vallés M, Mercadé M, Six-month color change and water sorption of 9 new-generation flowable composites in 6 staining solutionsBraz Oral Res 2016 30(1):e12310.1590/1807-3107bor-2016.vol30.012327901205 [Google Scholar] [CrossRef] [PubMed]