The Role of Prophylactic Diverting Loop Ileostomy in Preventing Leaks in High Risk Intraperitoneal Colonic Anastomosis: A Literature Review
Yusuf Afaque1, Mohammad Riyaz2, Mohammad Aslam3, Amjad Ali Rizvi4
1 Assistant Professor, Department of Surgery, J.N.M.C.H., Aligarh, Uttar Pradesh, India.
2 Junior Resident, Department of Surgery, J.N.M.C.H., Aligarh, Uttar Pradesh, India.
3 Professor, Department of Surgery, J.N.M.C.H., Aligarh, Uttar Pradesh, India.
4 Professor, Department of Surgery, J.N.M.C.H., Aligarh, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohammad Riyaz, Room No. 912, Gulzar Residency, Medical Road, Aligarh-202001, Uttar Pradesh, India.
E-mail: republicriyaz@gmail.com
Introduction
The anastomotic leak occurs in approximately 3-15% of patients who undergo colon and rectal surgery and can lead to significant morbidity and mortality. Prophylactic Diverting Loop Ileostomy (DLI) is done at times to prevent the anastomotic leak in high risk intraperitoneal colonic anastomosis. The role of DLI to prevent intraperitoneal colonic anastomosis leak is not well defined and we present the first review of literature to address this subject.
Aim
To do a literature review and study the role of prophylactic DLI for intraperitoneal colonic anastomosis.
Materials and Methods
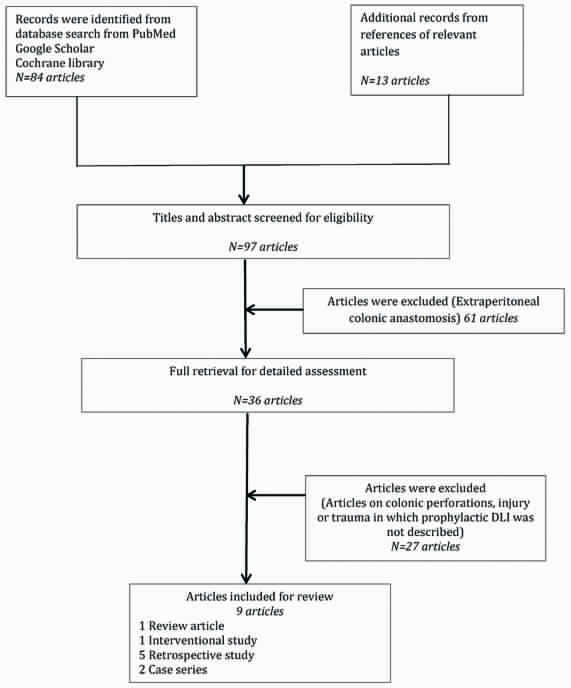
We searched the PubMed, Google Scholar and Cochrane Library database and also searched the reference of the relevant articles. After the extensive search, we got nine articles on this subject for review.
Results
For destructive colon injury with hypotension requiring more than four units of packed red blood cells or with significant co-morbidities, the high risk anastomosis becomes safer with a prophylactic DLI. For patients with pathological perforations, DLI can be added to safeguard colonic anastomosis if there are two or more risk factors for anastomotic leak. Patients not falling in above groups may not require prophylactic DLI for intraperitoneal colonic anastomosis.
Conclusion
Prophylactic DLI should be done to safeguard intraperitoneal colonic anastomosis only when there are multiple risk factors for the anastomotic leak.
Anastomotic leak, Colonic injury, Colonic perforations, Colonic surgery
Introduction
Anastomotic leak occurs in approximately 3-15% of patients who undergo colon and rectal surgery and can lead to significant morbidity and mortality [1,2]. Anastomotic complications are more common after colon and rectal surgery compared to gastric and small-bowel surgeries [3,4] and it is also the most common cause of death after colon and rectal surgery [5]. DLI is often done to prevent anastomotic complications in extraperitoneal rectal anastomosis when the integrity of anastomosis is in doubt. DLI is done to prevent the anastomotic leak of intraperitoneal colonic anastomosis also when there are risk factors for anastomotic leak, mostly in colonic trauma and colonic perforations in emergency surgeries and less often in elective surgeries. The role of DLI to prevent intraperitoneal colonic anastomosis leak is not well defined and there is scant literature on this. When should be DLI added to intraperitoneal colonic anastomosis? Does DLI prevent anastomotic leak or its septic complications or an emergency re-exploration? We studied the role of prophylactic DLI for intraperitoneal colonic anastomosis and present the first review of literature on this subject.
Materials and Methods
We searched the PubMed, Google Scholar and Cochrane Library with the words-ileostomy AND Colonic anastomosis, ileostomy AND emergency surgery, ileostomy AND anastomosis, colonic perforations, colonic injury and colonic trauma. We also searched the references of the relevant articles.
Inclusion criteria: Article on prophylactic DLI for intraperitoneal colonic anastomosis in adults (>15 years) in emergency surgery and elective surgery.
Exclusion criteria: Articles on prophylactic DLI for extraperitoneal colonic anastomosis or paediatric patients (<15 years).
Results
There is a large body of literature on the role of DLI for extraperitoneal colorectal anastomosis but scant literature on the role of DLI for intraperitoneal colonic anastomosis. After the extensive search, we got nine articles which have studied the role of prophylactic DLI for intraperitoneal colonic anastomosis [Table/Fig-1]. There were one review article, five retrospective studies, one interventional study and two case series [Table/Fig-2] [6-14]. These articles range from emergency to elective surgery and from traumatic to non-traumatic etiology and may seem heterogenous but they all have one common factor i.e., they have studied the role of DLI in the high risk intraperitoneal colonic anastomosis.
Flowchart of study selection.
Literature review [6-14].
| S. No. | Study Name | Year of Study | Study design | Number Patients/Article |
|---|
| 1. | Alves A et al., [6] | 2002 | Retrospective | 707 |
| 2. | Hedrick TL et al., [7] | 2006 | Retrospective | 15 |
| 3. | Steele SR et al., [8] | 2007 | Retrospective | 129 |
| 4. | Bax TW et al., [9] | 2007 | Case series | 13 |
| 5. | Rahman MS et al., [10] | 2013 | Case series | 09 |
| 6. | Bugiantella W et al., [11] | 2014 | Interventional | 14 |
| 7. | Midura EF et al., [12] | 2015 | Retrospective | 13,684 |
| 8. | Hawkins AT et-al., [13] | 2016 | Retrospective | 186 |
| 9. | Steele SR et al., [14] | 2011 | Review | 108 articles 3 abstract |
Literature Review
Alves A et al., proposed the first study on intraperitoneal anastomosis for which discussion on whether to create a protective stoma was relevant and on whom a multivariate analysis was performed [6]. A total of 707 consecutive patients who underwent colonic or rectal resection between 1990 and 1997 were reviewed retrospectively. Multivariate analysis showed that preoperative leukocytosis (p=0.03), intraoperative septic conditions (p=0.001), difficulties encountered during the anastomosis (p=0.007), colo-colic anastomosis (p=0.004), and amount of homologous transfused blood (p=0.0007) were independent factors associated with the anastomotic leak. They suggested that temporary stoma can be proposed for these high-risk patients, especially for those with two or more risk factors among the five independent factors for anastomotic leak.
Hedrick TL et al., did a retrospective study in which they did DLI along with drainage of the collection in 15 patients of colonic anastomotic leak and avoided dismantling the anastomosis [7]. Only one patient needed an additional drainage procedure after diversion. They suggested that DLI can even salvage an already disrupted colonic anastomosis and can take care of its septic complications.
Steele SR et al., did a retrospective study to analyse the management and clinical outcomes of patients suffering from colorectal injury at a combat hospital during Iraq war between September 2003 to December 2004 [8]. Management data of 160 patients with colorectal injury was available and 129 patients had right, left or transverse colon injury and 40 patients had rectal injury. Prophylactic DLI was made in 86 patients of which 11 patients had a leak. DLI was associated with lower leak rates (odds ratio, 0.06; p=0.04) but did not demonstrate impact on the incidence of sepsis or mortality.
Ninety-four consecutive patients undergoing DLI were evaluated from a prospective database between 2003 and 2006 by Bax TW et al., [9]. A total of 13 patients had segmental colonic resection for diverticulitis and colon cancer while the rest had rectal resections and low anastomosis. In patients with high-risk anastomosis due to acute infection or obstruction treatment was with resection anastomosis and foecal diversion using a loop ileostomy. They achieved anastomotic failure rate of 1%, a clinically significant leak rate of 3%, and an asymptomatic, radiologically identified leak rate of 2%. They believe that there is a cost associated with the ileostomy but benefits outweigh the costs.
Rahman MS et al., reported a case series on the management traumatic bowel injury. They did primary repair or resection anastomosis with a proximal diversion in 30% of colonic injury and reported acceptable outcome [10]. Bugiantella W et al., suggested that DLI may be beneficial to protect intra-peritoneal colonic anastomosis in elderly in emergency surgeries as it may be a difficult anastomosis due to the discrepancy in bowel diameter, localized or diffuse peritonitis or doubtful bowel vascularity [11]. They reported a novel method of diverting by a percutaneous ileostomy which did not require a second surgery for closure in ten patients with intra-peritoneal colorectal anastomosis and four patients with colo-colic anastomosis. None of the patients treated had evidence of clinical or radiological leakage of anastomosis.
Midura EF et al., did a retrospective analysis of 13,684 patients who underwent segmental colectomy with anastomosis at American College of Surgeons, National Surgical Quality Improvement Program–affiliated hospitals in 2012 [12]. They concluded that DLI was protective against overall anastomotic leak and specifically major anastomotic leaks that required reoperation but not for minor leaks. Multivariate analysis of DLI associated with anastomotic leak was-OR 0.55, 95% CI 0.31-0.97 and p-value=0.04.
Hawkins AT et al., reported the first study on the role of DLI to prevent open ileocolic anastomosis leak [13]. The American College of Surgeons National Surgical Quality Improvement Program (NSQIP) data was queried from 2012-2013. A total of 186 patients underwent a DLI. They concluded that DLI was not associated with a decrease in odds of anastomotic leak. There were no serious leaks requiring reoperation in DLI group but absolute risk reduction was minor as 40 loop ileostomies were required to prevent one serious anastomotic leak. Further, a DLI was associated with the almost two-fold increase in the odds of readmissions.
Steele SR et al., did the evidence-based review of 108 articles and three abstracts to determine the ideal treatment of non-iatrogenic traumatic injuries to the colon and rectum and concluded that non-destructive colonic injury can be repaired primarily and destructive injury without hypotension and comorbidities can be managed with resection and anastomosis [14]. Patients with the destructive colonic injury with shock requiring transfusion of greater than four units of packed red blood cells or with significant comorbidities, resection anastomosis with prophylactic DLI can be done as an alternative to Hartman’s procedure. Also, there was no difference between management of right and left colonic traumatic injuries.
Discussion
Management of colonic perforations has changed over time. During the era of World War One, there was the trend of primary anastomosis for emergency colonic perforations but the leak rate and mortality were high. During the second world war Ogilvie described in his 1945 article, “Surgical Lessons of War Applied to Civil Practice”: “The treatment of colon injuries was based on the known insecurity of suture and the dangers of leakage.” So exteriorizing the colon as stoma was the safest procedure and colonic repair or anastomosis was discouraged in emergency surgeries. This continued for decades. The loop ileostomy was first described by Turnbull RB et al., [15], using it in combination with two colostomies to decompress patients with toxic megacolon. In recent times many centres reported primary closure or anastomosis for emergency colonic perforations from penetrating injury with good results [16-20]. In pathological perforations of large bowel also the approach has changed. In perforated diverticular disease, the mandatory colonic exteriorization with Hartman’s procedure was being questioned [21] and retrospective studies and metanalysis has shown some advantage of primary anastomosis with or without diverting ileostomy, but in the absence of proper RCTs, sufficient conclusion cannot be made [22-25]. The Cochrane Systemic review demonstrated that the primary repair of penetrating colon injuries was not only as safe as the diversion but may in fact be safer. The mortality rate was similar in diversion and non-diversion groups [26]. Haemorrhagic shock with a transfusion requirement of greater than four units of packed red blood cells was the major factor that had been shown to be associated with inferior outcomes in primary repair group [27,28].
The number of published studies is not large but they give some scientific evidence on the role of DLI for intraperitoneal colonic anastomosis. To add or not to add DLI to a colonic anastomosis has to be decided depending on the bowel as well as the patient’s condition. For destructive colonic injury with hypotension requiring more than four units of packed red blood cells or with significant co-morbidities the high risk anastomosis becomes safer with a prophylactic DLI. For patients with pathological perforations, DLI can be added to safeguard colonic anastomosis if there are two or more risk factors for anastomotic leak. Patients not falling in the above groups may not require DLI for colonic anastomosis, as DLI has its own problems. These range from minor local care, to devastating requiring reoperation with prolonged inpatient care [29,30] and also will require a second reoperation with all the risks of a surgery. So as with extraperitoneal rectal anastomosis, DLI is to be added to intraperitoneal colonic anastomosis only when there are risk factors for anastomotic leak.
Limitation
The limitation of this study is that the number of published articles available for review is not large and most of them are retrospective study.
Conclusion
Prophylactic DLI should be done to safeguard intraperitoneal colonic anastomosis only when there are multiple risk factors for anastomotic leak.
[1]. Nesbakken A, Nygaard K, Lunde OC, Outcome and late functional results after anastomotic leakage following mesorectal excision for rectal cancerBr J Surg 2001 88(3):400-04.10.1046/j.1365-2168.2001.01719.x11260107 [Google Scholar] [CrossRef] [PubMed]
[2]. Parc Y, Frileux P, Schmitt G, Dehni N, Ollivier JM, Parc R, Management of postoperative peritonitis after anterior resection: experience from a referral intensive care unitDis Colon Rectum 2000 43(5):579-89.10.1007/BF0223556510826415 [Google Scholar] [CrossRef] [PubMed]
[3]. Csendes A, Burdiles P, Papapietro K, Diaz JC, Maluenda F, Burgos A, Results of gastric bypass plus resection of the distal excluded gastric segment in patients with morbid obesityGastrointest Surg 2005 9(1):121-31.10.1016/j.gassur.2004.05.00615623453 [Google Scholar] [CrossRef] [PubMed]
[4]. Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, Preen M, Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patientsDis Colon Rectum 2005 48(2):243-50.10.1007/s10350-004-0771-015714246 [Google Scholar] [CrossRef] [PubMed]
[5]. Isbister WH, Anastomotic leak in colorectal surgery: a single surgeon’s experienceANZ J Surg 2001 71(9):516-20.10.1046/j.1440-1622.2001.02189.x11527260 [Google Scholar] [CrossRef] [PubMed]
[6]. Alves A, Panis Y, Trancart D, Regimbeau JM, Pocard M, Valleur P, Factors associated with clinically significant anastomotic leakage after large bowel resection: multivariate analysis of 707 patientsWorld J Surg 2002 26(4):499-502.10.1007/s00268-001-0256-411910487 [Google Scholar] [CrossRef] [PubMed]
[7]. Hedrick TL, Sawyer RG, Foley EF, Friel CM, Anastomotic leak and the loop ileostomy: friend or foe?Dis Colon Rectum 2006 49(8):1167-76.10.1007/s10350-006-0602-616826334 [Google Scholar] [CrossRef] [PubMed]
[8]. Steele SR, Wolcott KE, Mullenix PS, Martin MJ, Sebesta JA, Azarow KS, Colon and rectal injuries during operation Iraqi freedom: Are there any changing trends in management or outcome?Dis Colon Rectum 2007 50(6):870-77.10.1007/s10350-007-0235-417468976 [Google Scholar] [CrossRef] [PubMed]
[9]. Bax TW, McNevin MS, The value of diverting loop ileostomy on the high-risk colon and rectal anastomosisThe American Journal of Surgery 2007 193(5):585-87.10.1016/j.amjsurg.2007.01.00517434360 [Google Scholar] [CrossRef] [PubMed]
[10]. Rahman MS, Khair MA, Khanam F, Haque S, Bhuiyan MR, Hoque MM, Traumatic gut injury: a study of 100 cases in Mymensingh Medical College HospitalMymensingh Med J 2013 22(3):452-59. [Google Scholar]
[11]. Bugiantella W, Rondelli F, Mariani L, Boni M, Ermili F, Avenia N, Temporary percutaneous ileostomy for faecal diversion after intestinal resection for acute abdomen in elderly: how to avoid the conventional loop ileostomyInt J Surg 2014 12(Suppl 2):S144-47.10.1016/j.ijsu.2014.08.36125157995 [Google Scholar] [CrossRef] [PubMed]
[12]. Midura EF, Hanseman D, Davis BR, Atkinson SJ, Abbott DE, Shah SA, Risk factors and consequences of anastomotic leak after colectomy: a national analysisDis Colon Rectum 2015 58(3):333-38.10.1097/DCR.000000000000024925664712 [Google Scholar] [CrossRef] [PubMed]
[13]. Hawkins AT, Dharmarajan S, Wells KK, Krishnamurty DM, Mutch MG, Glasgow SC, Does diverting loop ileostomy improve outcomes following open ileo-colic anastomoses? A nationwide analysisJ Gastrointest Surg 2016 20(10):1738-43.10.1007/s11605-016-3230-z27507555 [Google Scholar] [CrossRef] [PubMed]
[14]. Steele SR, Maykel JA, Johnson EK, Traumatic injury of the colon and rectum: the evidence vs dogmaDis Colon Rectum 2011 54(9):1184-201.10.1007/DCR.0b013e3182188a6021825901 [Google Scholar] [CrossRef] [PubMed]
[15]. Turnbull RB Jr, Hawk WA, Weakley FL, Surgical treatment of toxic megacolon. Ileostomy and colostomy to prepare patients for colectomyAm J Surg 1971 122(3):325-31.10.1016/0002-9610(71)90252-2 [Google Scholar] [CrossRef]
[16]. Stone HH, Fabian TC, Management of perforating colon trauma: randomization between primary closure and exteriorizationAnn Surg 1979 190(4):430-36.10.1097/00000658-197910000-00002384941 [Google Scholar] [CrossRef] [PubMed]
[17]. Burch JM, Feliciano DV, Mattox KL, Colostomy and drainage for civilian rectal injuries: is that all?Ann Surg 1989 209(5):600-10.10.1097/00000658-198905000-000132705824 [Google Scholar] [CrossRef] [PubMed]
[18]. Al-Qasabi QO, Katugampola W, Singh ND, Management of colon injuriesInjury 1991 22(1):32-34.10.1016/0020-1383(91)90157-A [Google Scholar] [CrossRef]
[19]. Demetriades D, Penetrating injuries of the colon-changing perspectivesS Afr J Surg 1991 29(1):25-25. [Google Scholar]
[20]. Pachter HL, Hoballah JJ, Corcoran TA, Hofstetter SR, The morbidity and financial impact of colostomy closure in trauma patientsJ Trauma 1990 30(12):1510-13.10.1097/00005373-199012000-000122258963 [Google Scholar] [CrossRef] [PubMed]
[21]. Cirocchi R, Afshar S, Saverio S, Popivanov G, Sol AD, Gubbiotti F, A historical review of surgery for peritonitis secondary to acute colonic diverticulitis: from Lockhart-Mummery to evidence-based medicineWorld J Emerg Surg 2017 12:1410.1186/s13017-017-0120-y28293278 [Google Scholar] [CrossRef] [PubMed]
[22]. Salem L, Flum DR, Primary anastomosis or Hartmann’s procedure for patients with diverticular peritonitis? A systematic reviewDis Colon Rectum 2004 47(11):1953-64.10.1007/s10350-004-0701-115622591 [Google Scholar] [CrossRef] [PubMed]
[23]. Constantinides VA, Tekkis PP, Athanasiou T, Aziz O, Purkayastha S, Remzi FH, Primary resection with anastomosis vs. Hartmann’s procedure in nonelective surgery for acute colonic diverticulitis: a systematic reviewDis Colon Rectum 2006 49(7):966-81.10.1007/s10350-006-0547-916752192 [Google Scholar] [CrossRef] [PubMed]
[24]. Abbas S, Resection and primary anastomosis in acute complicated diverticulitis, a systematic review of the literatureInt J Colorectal Dis 2007 22(4):351-57.10.1007/s00384-005-0059-416437211 [Google Scholar] [CrossRef] [PubMed]
[25]. Lorusso D, Gilberti A, Bianco M, Gioacchino Non-elective surgery for acute complicated diverticulitis. Primary resection-anastomosis or hartmann’s procedure? A systematic review and meta-analysisJournal of Surgery 2016 12(2):43-49.10.7438/1584-9341-12-2-1 [Google Scholar] [CrossRef]
[26]. Nelson R, Singer M, Primary repair for penetrating colon injuriesCochrane Database Syst Rev 2003 (3):CD00224710.1002/14651858.CD002247PMC7003569 [Google Scholar] [CrossRef] [PubMed]
[27]. Miller PR, Fabian TC, Croce MA, Magnotti LJ, Elizabeth Pritchard F, Minard G, Improving outcomes following penetrating colon wounds: application of a clinical pathwayAnn Surg 2002 235(6):775-81.10.1097/00000658-200206000-0000412035033 [Google Scholar] [CrossRef] [PubMed]
[28]. Hudolin T, Hudolin I, The role of primary repair for colonic injuries in wartimeBr J Surg 2005 92(5):643-47.10.1002/bjs.491515800953 [Google Scholar] [CrossRef] [PubMed]
[29]. Harris DA, Egbeare D, Jones S, Benjamin H, Woodward A, Foster ME, Complications and mortality following stoma formationAnn R Coll Surg Engl 2005 87(6):427-31.10.1308/003588405X6071316263009 [Google Scholar] [CrossRef] [PubMed]
[30]. Shellito PC, Complications of abdominal stoma surgeryDis Colon Rectum 1998 41(12):1562-72.10.1007/BF022373089860339 [Google Scholar] [CrossRef] [PubMed]