Vitamin D is pivotal for healthy bone mineralisation. The foundation of peak bone mass; an important determinant of osteoporotic fracture risk, is laid down in early infancy [1]. Vitamin D deficiency (<20 ng/mL), leads to defective bone mineralisation and decreased bone mineral content [2]. Its prevalence in term healthy breastfed infants has been reported variably as 20-82% in various studies [3,4]. The deficiency is rising in correspondence with increasing exclusive breastfeeding rates, breast milk being a poor source of vitamin D and inadequate vitamin D supply would imply defective bone mineralisation [5,6]. Vitamin D levels inversely correlate with TALP and BSALP [7]. Osteoblasts, which exhibit receptors for Parathormone (PTH) and vitamin D, secrete TALP and BSALP during bone formation which provide an indirect estimation of dynamics of the bone mineralisation process and have been shown to be a significant marker of Whole Body Bone Mineral Content (WBBMC) in the newborn [7]. Breast milk contains 15-50 IU/L vitamin D, which is insufficient to meet the needs of neonates [5,6]. There exist international recommendations to supplement exclusively breast fed babies with oral vitamin D, however the same has not been substantiated by evidence based studies in India [8]. It was felt that there is a requirement of Indian studies in the matter given that the handling of vitamin D in the body differs in the people of different races, colour and ethnicity. The presence of dark skin, decreased activity of 25(OH) hydroxylase (an enzyme involved in the synthesis of an active form of vitamin D) in Asian population lack of fortification policies in India predispose mothers and their infants to vitamin D deficiency [9]. Another fact is that there is a paucity of data from India regarding the impact of vitamin D supplementation on bone mineralisation in a neonate.
Present study was conceptualised to study the impact of vitamin D supplementation on biochemical markers for bone mineralisation, vitamin D status in the body and growth (first six months), in term healthy exclusively breastfed neonates.
Materials and Methods
Subjects and setting: It was an open-label (unblinded), parallel, superiority randomised controlled trial with 1:1 allocation ratio, conducted in post-natal ward setting of Postgraduate Institute of Medical Education and Research and Dr Ram Manohar Lohia Hospital Hospital, New Delhi, India from January 2013 to February 2014 Consecutively born full term healthy neonates born to mothers who were residents of Delhi and chose to exclusively breastfeed their infant and consent for participation in this follow-up study were eligible. Babies with life threatening congenital malformations or born to HIV positive mothers were excluded. Hundred babies were randomised to receive the intervention (study group) or no intervention (control group).
Ethical approval: The study was undertaken after approval from Institutional Ethics Committee and was in accordance with declaration of Helsinki 1975 modified in 2000.
Sample size: As per the previous study and assuming 20%±5% change in levels of TALP and BSALP in two groups, a sample size of 42 in each group was required at an alpha error of 5% and power of 80% [7]. Giving an allowance for 20% losses in the follow-up a total of 100 babies with 50 infants in each group were needed.
Randomisation: A series of computer-generated random number sequence was prepared by Inclen Trust, New Delhi, using Stata 9.0 software. Block randomisation was done using alternate block sizes of 4 and 6. Allocation concealment was achieved using sequentially numbered opaque sealed envelopes; safely secured with a person not involved in the study until subject enrolment. Vitamin D containing bottles were numbered as per enrolment number of each participant. No placebo was used.
Intervention: After written consent, blood samples from umbilical cord and mother were collected simultaneously, centrifuged, separated, transported to and stored in laboratory at -80°C untill batch analysis. Calcium, Phosphorus and TALP were analysed within 24 hours of collection. After randomisation, each baby of the intervention group received 30 mL bottle of vitamin D (Containing 400 IU/mL Cholecalciferol). At discharge, each parent was explained to store the bottle away from sunlight and administer 1 mL daily from this preparation to his/her baby, maintaining a compliance log chart. Each parent was required to deposit the empty bottle on the same day its contents were empty. A new vitamin D bottle was issued and number of missed doses of vitamin D documented at that visit. The control group received no supplement as Ethics Committee did not approve the use of any placebo in neonates. Infants in both groups were followed at 2, 6, 10, 14 weeks and 6 months, Importance to maintain exclusive breastfeeding until 6 months and compliance to intervention where applicable, were reinforced at each visit. Clinical, biochemical and ultrasonographic screenings for symptoms of vitamin D toxicity (decreased feeding/vomiting/constipation/ irritability/lethargy/hypercalciuria by urinary calcium creatinine ratio/ nephrocalcinosis by renal ultrasound) and also weight, head circumference and length measurements in all babies at respective follow-up were done. The pattern of breastfeeding was defined as per WHO definitions [10]. Compliance was categorised as optimal, good, unsatisfactory and poor if vitamin D intake was >75%, 50-75%, 25-50% and <25% of the total days respectively.
Outcome variables: Primary-change in TALP and BSALP levels from birth until six months of daily 400 IU oral vitamin D supplementation in term healthy exclusively breastfed newborn infants as compared to control group.
Secondary-change in anthropometry and Vitamin D status (vitamin D, PTH, calcium, phosphorus) within and between two groups from birth to six months.
Outcome measurement BSALP: Immunoassay using a monoclonal anti-BAP antibody coated on the strip to capture BAP in sample using pNPP (p-Nitrophenyl Phosphate) as substrate (BAP OSTASE kit). TALP, calcium, phosphorus, Vitamin D and PTH: by chemiluminescence on VitrosEci Immunoassay analyser. Observed values were compared to reference values [Table/Fig-1]. Weight was measured on the same digital electronic scale (Global Medical Systems, New Delhi) to nearest 5 gm, length and head circumference to nearest 0.1 cm using infantometer and nonstretchable measuring tape (Khanna Surgicals, Delhi) respectively.
Reference values for Biochemical Parameters used in study.
| Parameter | Cord blood | Six months | Unit |
|---|
| Calcium | 7-11 | 9-11 | mg/dL |
| Phosphorus | 5-7.8 | 4-6.5 | mg/dL |
| Vitamin D | >20 | >20 | ng/mL |
| PTH | 4.5±2.3 | 38±12.5 | pg/mL |
| BSALP | 64±17 | 68±20 | mcg/L |
| TALP | 60-220 | 60-220 | IU/L |
# Reference values from Nelson Textbook of Pediatrics 19th edition
PTH: Parathormone; BSALP: Bone specific alkaline phosphatase; TALP: Total alkaline phosphatase; mg: Milligrams; ng: Nanograms; pg: Picograms; IU: International units
Statistical Analysis
Stata 11.0 (College Station, Texas, USA) was used for analysis. Qualitative and quantitative data were presented as number (%) and mean+SD/median (Min-Max) respectively with 95% confidence interval. Baseline quantitative and qualitative characteristics were compared between two groups using Student’s t-test for independent samples and chi-square test respectively.
BSALP and TALP (primary outcome), calcium, phosphorus, vitamin D, PTH and somatic growth profile (secondary outcomes), were compared between two groups using unpaired t-test and a Paired t-test within the group. ANCOVA was used to compare the difference in mean between two groups after adjusting for baseline vitamin D and PTH. The non-normal variables were compared between two groups using Wilcoxon ranksum test. Correlation between two continuous variables was done using Pearson’s correlation test. The p-value of <0.05 was considered statistically significant. There was no protocol deviation throughout the study and intention to treat analysis was carried out for the results.
Results
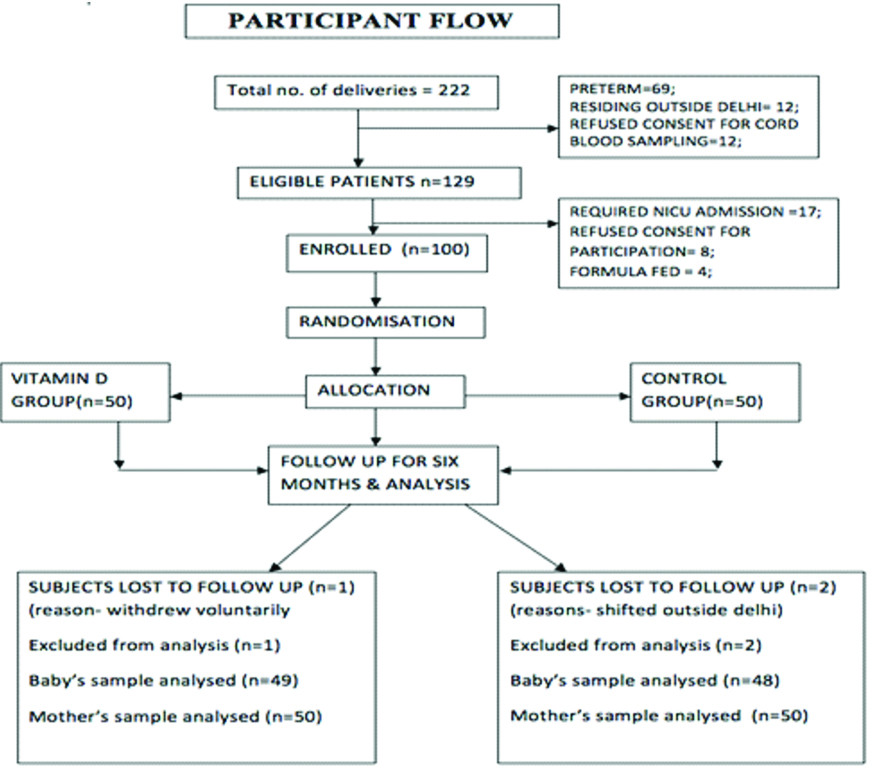
A total of 222 babies were delivered in a tertiary care hospital in New Delhi from April 2013 to July 2013. Out of which 129 were eligible (69 preterms, 12 did not consent for cord blood samples and 12 residing outside Delhi), of the eligible 17 required NICU admission, 8 refused consent for participation. A total of 100 babies meeting inclusion criteria were enrolled and randomised to respective groups within 24 hours of birth. Two were lost to follow-up (shifted out of Delhi) and one withdrew consent within initial one week of the study [Table/Fig-2]. The baseline demographic characteristics of two groups were comparable [Table/Fig-3]. There was statistically significant difference in levels of vitamin D, PTH and TALP at baseline in between two groups (p<0.05). This difference was adjusted and taken into account for the possible impact on primary outcomes. There was no significant difference in baseline values for other biochemical parameters (Calcium, Phosphorus and BSALP) and baseline anthropometric indices were also comparable. All the babies were exclusively breastfed at birth in both groups. By three months, 98% of the babies in each group were exclusively breast-fed and at six months 92% were exclusively breast fed in vitamin D group and 86% in the control group.
Baseline Characteristics.
| Characteristics | | Vitamin D Groupn=50 (%) | Control Group n=50 (%) | p-value$ |
|---|
| Maternal |
| Vaginal delivery* | | 36 (72%) | 42 (84%) | 0.09 |
| Primiparous* | | 33 (66%) | 36 (72%) | 0.55 |
| Housewives* | | 41 (82%) | 40 (80%) | 0.49 |
| Education (Graduate and above)* | | 37 (74%) | 43 (86%) | 0.45 |
| Vegetarian dietary habit* | | 23 (46%) | 27 (54%) | 0.10 |
| Antenatal supplements | Calcium* | 49 (98%) | 49 (98%) | 0.67 |
| vitamin D* | 49 (98%) | 49 (98%) |
| Maternal age (mean+SD) in Years# | 27.1±3.9 | 26.9±3.3 | 0.76 |
| Maternal vitamin D status |
| Calcium (mg/dl)# | | 9.18±0.63 | 9.11±0.6 | 0.64 |
| Phosphorus (mg/dl)# | | 4.3±3.9 | 3.9±0.9 | 0.55 |
| TALP (IU/L)# | | 145.9±84.8 | 145.88±45.2 | 0.27 |
| Vitamin D (ng/ml)# | | 11.3±10.3 | 12±11.4 | 0.58 |
| PTH (pg/ml)# | | 22.3±19.1 | 17.55±12.5 | 0.25 |
| NEONATE* | | | | |
| Male* | | 31 (62%) | 24 (48%) | 0.15 |
| Females* | | 19 (38%) | 26 (52%) | |
| Gestational age (mean+SD) in wks# | | 38.1±0.87 | 38.3±0.82 | 0.07 |
| Vitamin D status of baby |
| BSALP (IU/L)# | | 87.8±28.7 | 80±23.9 | 0.14 |
| TALP (IU/L) | | 155.8±41.8 | 122.32±36.6 | <0.001 |
| Calcium (mg/dl)# | | 9.6±0.55 | 9.5±0.39 | 0.2 |
| Phosphorus (mg/dl)# | | 4.07±0.91 | 3.89±0.69 | 0.3 |
| Vitamin D (ng/dl)# | | 15.6±14.6 | 21.9±8.3 | <0.001 |
| PTH (pg/ml)# | | 5.8 (3-193.6) | 7.4 (3,43.7) | 0.02 |
SD: Standard deviation; PTH: Parathormone; BSALP: Bone specific alkaline phosphatase; TALP: Total alkaline phosphatase; mg: Milligrams; ng: Nanograms; pg: Picograms; IU: International units; mg: Milligrams; ng: Nanograms; pg: Picograms; IU: International units; *Test of significance- Chi square test, #Test of significance- Independent samples t test; $Level of significance 0.05, 95% Confidence interval
Primary outcome: Change in TALP was found to be significantly different compared to the control group (p<0.001). However, BSALP between the two groups was not statistically significant (p=0.6251) at six months. The difference in values of BSALP (-12.77 and -16.5) in each group was adjusted for baseline difference in levels of vitamin D, PTH and TALP in between the two groups and was 9.86 (-3.12, 22.8), which was not statistically significant (p>0.05) [Table/Fig-4].
Change in Primary Outcome Variables between Two Groups and within the Group at 6 months.
| Time points* | Vitamin D group Mean±SD | Control group Mean±SD | p-value$ |
|---|
| Baseline | 87.8±28.7 | 80±23.9 | 0.14 |
| Six months | 73.7±31.9 | 64±25.8 | 0.15 |
| p-value | 0.02 | <0.001 | |
| Change in BSALP$ | -12.77 [-24.15, -1.38] | -16.5 [-26.7, -6.26] | |
| BSALP$ | 3.732 [-11.38, 18.84] | 0.6251 |
| Adjusted difference$ | 9.86 [-3.12, 22.8] | 0.135 |
SD: Standard deviation; BSALP: Bone specific alkaline phosphatase; $Level of significance 0.05, 95% Confidence interval; *Test of significance-independent samples t-test between two groups and paired t-test for comparison within the group
Secondary outcome: There was significant increase in level of vitamin D and calcium in vitamin D group at six months, unlike the control group. No significant differences were seen between anthropometric indicis of the two groups. There was no evidence of vitamin D toxicity in any of the babies [Table/Fig-5,6]. There was poor correlation between newborn baby’s and mother’s vitamin D levels at birth. (Correlation coefficient r=0.052, significance=0.609). In study group, 60% of infants were vitamin D deficient at birth as compared to 34% in the control group at the time of enrolment, whereas deficiency status reversed to 40% and 76% in study and control group respectively at the end of the study [Table/Fig-7].
| Anthropometry* | | Vitamin D group Mean±SD | Control group Mean±SD | p-value# |
|---|
| Birth weight (mean±SD) (in Kilograms) | At birth | 2.89±0.34 | 2.95±0.43 | 0.42 |
| At six months | 6.61±0.46 | 6.55±0.44 | 0.50 |
| weight# | 0.0918 [-0.121, 0.3055] | 0.39 |
| Length at birth (mean±SD) (in centimeters) | At birth | 48.11±1.92 | 47.6±2.14 | 0.217 |
| At six months | 62.54±3.5 | 61.6±2.85 | 0.16 |
| length# | 0.324 [-0.827, 1.477] | 0.57 |
| HC at birth (mean±SD) (in centimeters) | At birth | 34.6±0.9 | 34.7±0.87 | 0.504 |
| At six months | 41.23±1.29 | 41.26±1.06 | 0.90 |
| HC# | 0.045 [-.0424, 0.514] | 0.84 |
| MAC at birth (mean±SD) (in centimeters) | At birth | 10.6±0.56 | 10.8±0.54 | 0.98 |
| At six months | 13.07±0.707 | 13.2±0.61 | 0.10 |
| MAC# | 0.215 [-0.0709, 0.502] | 0.13 |
SD: Standard deviation; HC: Head circumference; MAC: Mid arm circumference
*Test of significance-independent samples t-test between two groups and paired t-test for comparison within the group; #95% confidence Interval, Level of significance 0.05
Showing change in Secondary Outcome Variables.
| Parameter (units)* | Time points | Vitamin D group Mean±SD | Control group Mean±SD | p-value$ |
|---|
| Vitamin D(ng/ml)#$ | Baseline | 15.6±6.39 | 22.7±8.88 | <0.001 |
| Six months | 30.2±18.3 | 26.9±16.2 | 0.35 |
| p-value | <0.001 | 0.35 | |
| Difference | 14.7 [9.53, 20.03] | 4.9 [0.21, 9.77] | |
| V | 9.79 [2.780, 16.806] | 0.006 |
| PTH(pg/ml)#$ | baseline | 5.8 (3-229.7] | 4.6 (3-68.6] | 0.02 |
| Six months | 7.4 (3-43.7] | 4.35 (3-193.6] | 0.008 |
| p-value | 0.16 | 0.63 | |
| Difference | -1.5 [-11.9, 8.96] | 4.55 [-5.23, 14.3] | |
| P | -6.063 [-20.18, 8.054] | 0.39 |
| Calcium(mg/dl)$ | baseline | 9.6±0.55 | 9.5±0.39 | 0.2 |
| Six months | 10.2±0.51 | 9.5±0.47 | <0.001 |
| p-value | <0.001 | 0.9 | |
| Difference | 0.55 [0.35, 0.746] | 0.01 [0.17, 0.19] | |
| C | 0.54 [0.278, 0.804] | <0.001 |
| Phosphorus$ (mg/dl) | baseline | 4.07±0.91 | 3.8±0.69 | 0.3 |
| Six months | 4.37±0.69 | 4.13±0.73 | 0.12 |
| p-value | 0.12 | 0.8 | |
| Difference | 0.247 [-0.074, 0.57] | 0.237 [-0.032, 0.507] | |
| iP | 0.010 [-0.404, 0.425] | 0.96 |
| TALP(IU/L)$ | baseline | 155.8±41.8 | 122.32±36.6 | <0.001 |
| 6 months | 106±40.4 | 109.6±35.8 | 0.6 |
| p-value | <0.001 | <0.001 | |
| Difference | -50.02 [-64.01, -36.03] | -12.44 [-21.76, -3.13] | |
| TALP | -37.57 [-54.09, -21.04] | <0.001 |
SD: Standard deviation; PTH: Parathormone; TALP: Total alkaline phosphatase; Test of significance-independent samples t-test between two groups and paired t-test for comparison within the group; #ANCOVA used for calculation of adjusted difference; $95% confidence Interval, Level of significance 0.05
Shows the reduction in percentage of vitamin D deficient babies after six months of vitamin D supplementation.
| % vitamin D deficient babies | vitamin D group | Control group |
|---|
| At birth | 60% | 34% |
| At six months | 40% | 76% |
Discussion
Vitamin D supplemented group of babies showed a statistically significant decline in TALP after six months compared to the control group; however, difference of fall in levels of BSALP between the two groups was not significant. TALP reflects bone turnover and its bone isoform i.e., BSALP is a marker of osteoblastic activity. There is increase in alkaline phosphatase as bone growth occurs but there are also studies that link vitamin D deficiency with increased ALP levels and both share an inverse relationship. The exact role of alkaline phosphatase in bone mineralisation is unknown; however, it is proposed that its bone isoform BSALP might provide valuable information in dynamics of mineralisation process over a period of time. Adult studies show a reduction in BSALP after supplementation with vitamin D. BSALP, unlike TALP, is relatively less used marker with respect to status in vitamin D deficiency and we also don’t have standard norms for the same in neonates [11]. From the observation of significant fall in TALP between the groups at six months unlike its bone isoform, it appears that TALP responded earlier while change in BSALP did not and it is possible that it may require a sustained supplementation for an extended period to document a significant fall.
According to a recent study, vitamin D threshold to initiate change in TALP and BSALP is 20-24 ng/mL; levels higher than observed in present study [12]. Given the heterogeneity in vitamin D status of the population, probably we need to study effect of supplementation on a large population group and for an extended period of time to document a significant change in BSALP similar to TALP and thereby improvement in bone mineralisation reflecting it as a specific marker of the same. A significant observation in this study was high prevalence of vitamin D deficiency in the study population of mothers and babies in both the groups at the outset [Table/Fig-3]. This observation was similar to studies in other Asian countries [9,13] the possible reasons for this have been discussed earlier. It was also noted that supplementation with vitamin D at a dose of 400 IU/day was effective in reduction in the deficiency status in the study group as compared to the control group [Table/Fig-6,7]. In the study group, 60% of infants were vitamin D deficient at birth as compared to 34% in the control group at the time of enrolment, whereas deficiency status reversed to 40% and 76% in study and control group respectively at the end of the study [Table/Fig-7]. Vitamin D supplementation in healthy term exclusively breastfed infants is advocated in view of the fact that there is decreased bone turnover as compared to unsupplemented group and possibly improvement in bone mineralisation as well. There is a high prevalence of vitamin D deficiency in mothers despite antenatal vitamin D supplementation as well as newborns and mother with sufficient vitamin D does not ensure vitamin D sufficiency in the baby because there is poor correlation amongst mother and baby pair. There are studies that show mother’s level of vitamin D <10 ng/mL, correlate poorly with that of the baby’s, otherwise at higher levels there is a positive correlation and in the present study we found ~91% of the mothers had <15 ng/mLof vitamin D [14]. The observation of marked fall in percentage of newborn with vitamin D deficiency from 60% to 40% after six months of vitamin D supplementation further adds to benefit of supplementation. The need of vitamin D in a baby should be individualised and fulfilled with adequate doses to prevent risk of osteoporosis later in life. This study holds promise and improves future scope for usage of more specific marker for risk of osteopenia in neonates. Vitamin D supplementation did not cause any toxicity in dose of 400 IU per day and to recommend it’s supplementation to all neonates and measurement of BSALP as surrogate marker of improved mineralisation would require further studies on a larger population.
Limitation
The present study had some limitations. It was an unblinded study and we did not use a placebo as it was not approved by ethics committee. BSALP samples were stored at -80°C for batch analysis. Whether this difference in time measurement influenced the results cannot be said with certainty. In addition we do not have standardised methods to estimate BSALP. In the present study enzyme immunoassay was used to determine BSALP levels though there are other methods like IRMA, RIA and electrophoresis also available and the accuracy of all the methods is not yet established.
Conclusion
Vitamin D deficiency has a high prevalence in newborns and majority of the mothers remain deficient despite supplements. There is a reduction in the percentage of vitamin D deficient babies after six months of vitamin D supplementation. This has a beneficial effect on bone mineralisation as evidenced by a significant decrease in TALP levels. We need to supplement healthy term neonates, who are exclusively breastfed, with 400 IU per day of vitamin D daily. This is a safe dose without any adverse effects. Whether we require higher doses of vitamin D for a better outcome or we need to conduct longer duration studies for a significant change in markers of bone formation and growth parameters still remains unanswered and needs to be dealt with in future high quality studies.
# Reference values from Nelson Textbook of Pediatrics 19th edition
PTH: Parathormone; BSALP: Bone specific alkaline phosphatase; TALP: Total alkaline phosphatase; mg: Milligrams; ng: Nanograms; pg: Picograms; IU: International units
SD: Standard deviation; PTH: Parathormone; BSALP: Bone specific alkaline phosphatase; TALP: Total alkaline phosphatase; mg: Milligrams; ng: Nanograms; pg: Picograms; IU: International units; mg: Milligrams; ng: Nanograms; pg: Picograms; IU: International units; *Test of significance- Chi square test, #Test of significance- Independent samples t test; $Level of significance 0.05, 95% Confidence interval
SD: Standard deviation; BSALP: Bone specific alkaline phosphatase; $Level of significance 0.05, 95% Confidence interval; *Test of significance-independent samples t-test between two groups and paired t-test for comparison within the group
SD: Standard deviation; HC: Head circumference; MAC: Mid arm circumference
*Test of significance-independent samples t-test between two groups and paired t-test for comparison within the group; #95% confidence Interval, Level of significance 0.05
SD: Standard deviation; PTH: Parathormone; TALP: Total alkaline phosphatase; Test of significance-independent samples t-test between two groups and paired t-test for comparison within the group; #ANCOVA used for calculation of adjusted difference; $95% confidence Interval, Level of significance 0.05