Non-communicable diseases which are also called the “New World Syndrome”, has taken a toll on the health economics throughout the world [1]. Since then the WHO, as well as researchers from various fields, have been researching for data regarding the global impact of non-communicable diseases both at the national and international level.
Though the causes of non-communicable diseases are many, lifestyle-related causes, leads the way in the uprise of non-communicable diseases. Lifestyle is a subjective concept of the way of living which is directly linked to one’s own behavioural patterns in activities, attitudes, interests, opinion and so on. These behavioural patterns can be altered according to the individual needs and interest. Recently the biorhythm of lifestyle among the general population has been unstable due to decline in daily upkeep of health, altered living habits by stressors and change in thinking habits as well as misperception regarding body types and lifestyle related diseases [2,3].
Obesity is one of the serious outcomes of lifestyle that erodes the socioeconomic and public health burden all over the world. India was once upon a time, considered to face under the category of malnutrition, and is now reported to be gaining a large number of overweight and obese individuals [1]. Obesity occurs when energy intake exceeds its output for an extended period of time [4]. According to the National Family Health Survey (NFHS) -4 released on 17 January, 2017, obesity in India has doubled in the past 10 years [5]. Furthermore, underweight and overweight/obesity are both higher among the women than men [1,5]. In India, the prevalence of adult obesity is not only rising but also seen is a rise in overweight and obese adolescents which has been reported to be between 10-30% [1].
Weight not only comprises of lean mass or fat mass but also includes water and visceral fat [5]. Multiple methods exist to measure adiposity such as BMI, waist circumference, waist height ratio, underwater weighing, Bioelectrical Impedance Analysis (BIA), Dual Energy X-Ray Absorptiometry (DEXA), Magnetic Resonance Imaging (MRI) to name a few [6]. In spite of their accurate measurements, MRI and DEXA are expensive, non-portable, time consuming and require skilled workers to operate the devices. BMI and BIA can be used to determine adiposity in a population-based survey. However, BMI is one of the clinical tools that is easily used to classify subjects into underweight, overweight or obese category [6,7]. However, the major drawback is that it cannot distinguish between lean mass and fat mass leading to underestimation of subjects with invisible obesity and overestimation of those with muscular obesity [5-8]. BIA is a quick, safe, non-invasive procedure that estimates total body water determined by impedance from which free fat mass is estimated [5,9]. Recently many scholars have tried to introduce the concept of determination of BFP as an aid to determine the health status of an individual. Body fat can be distinguished as subcutaneous fat and visceral fat. Both play a role in the normal physiological functions of the body. It was generally accepted that if the visceral fat increases it causes the development of NCD [10]. Besides, Indians have the tendency of accumulating abdominal fat more compared to other regions of the body putting them in the category of metabolically obese, normal weight individuals [11]. Even though the study on BFP is vast, it does not provide conclusive answers to the questions related to lifestyle. Hence, the need for further investigation of these concepts is absolutely necessary.
Due to the highly demanding and time-consuming first-year curriculum, less time availability for physical activity or healthy eating, medical students are more likely to have increased body fat mass, which makes us wonder whether the budding health caregivers and keepers of today’s world are healthy? Since the young medical students are our future health educators, directing advice to them can bring a change to this pandemic of lifestyle associated diseases.
The present study assesses the lifestyle in the undergraduate first year medical students and also to determines if lifestyle has any influence on BMI and BFP.
Materials and Methods
The present cross-sectional study was conducted at Jubilee Mission Medical College and Research Institute across a period of one month after approval from the Institutional Ethics Committee. The sample size included 100 first-year medical students. The participation was voluntary and all the 100 students consented to participate in the study. The subjects included 66 female and 34 male subjects. The students with any kind of illness, those who were menstruating (female subjects) and those who showed disinterest in participation were excluded from the study. The first-year medical students who were between the ages of 18-25 years, were included in the study.
Body composition: Body composition analysis was performed using body composition analyser (OMRON–HBF 375) during 10 am under controlled conditions since fluctuation of body water levels and situations such as after a large meal, menstruation, exercising, and illness can alter the body composition readings. General information such as date of birth, gender and height have to be fed to the device earlier. Height was measured to the nearest 0.1 cm using a wall-mounted stadiometer. The analyser determines the body composition using bioelectrical impedance or biological resistance method by using weak currency (50 KHz, 500 μA) flowing through both hands and feet [5,9]. The device provides us with weight, BMI and total BFP which has been used in the present study to correlate with lifestyle.
BMI was categorised based on Asian standards (WHO) which shows <18.5 kg/m2 (underweight), 18.5-22.9 kg/m2 (normal), 23.0-24.9 kg/m2 (overweight), >/=25 kg/m2 (obese) [12]. Body fat levels were categorised based on gender (male(M)/female(F)) provided by the device; ≥25% (M)/≥35% (F)-very high; 20-25 % (M)/30-35% (F)-high; 10-20% (M)/20-30% (F)-normal;<10% (M)/<20% (F)-low.
Questionnaire: Lifestyle data was obtained through the Fantastic lifestyle Questionnaire developed by Douglas and Donna [13]. The questionnaire consists of random questions with multiple choices that consider the behaviours of individual towards their daily life style. It includes 25 questions with nine areas arranged in the form of Likert’s Scale namely: 1) family and friends; 2) physical activity; 3) nutrition; 4) tobacco and toxins; 5) alcohol; 6) Sleep, seat belt, stress, safe sex; 7) type of personality; 8) insight; and 9) career from which 23 questions have 5 possible answers and 2 questions with 2 possible answers. The questionnaire was encoded by points; 0 points for almost never; 1 point for seldom; 2 points for some of the time, 3 points for fairly often and 4 points for almost always. The sum of all points gives the total score which is categorised as excellent (85-100 points), very good (70-84 points), good (55-69 points), fair (35-54 points) and poor (0-34 points). In the present study, we clubbed the excellent, very good, good and fair as “good lifestyle category (>35 points)” and “poor lifestyle category (<35 points)” [13].
Statistical Analysis
The results were tabulated using Microsoft Office Excel spreadsheet and charted using bivariate analysis for correlation and Fisher’s-Exact test for associations through cross-tabulation using SPSS version 20.0 to find the correlation and significance respectively of the lifestyle with BMI and BFP. The correlation and significance values have been explained in each table. In the present study, p-values of <0.05 were considered statistically significant.
Results
Out of 100 frist-year medical students, 66 were females and 34 were male subjects aged between 18-25 years. After the scoring of lifestyle questionnaire, it was found that majority of present students belonged to poor lifestyle group. The [Table/Fig-1] describes 72% of students in poor lifestyle group and 28% of the students in the good lifestyle group.
Distribution of good lifestyle and poor lifestyle among the students.
| n=100 | Frequency | Percent (%) |
|---|
| Lifestyle | Good | 28 | 28.0 |
| Poor | 72 | 72.0 |
| Total | 100 | 100.0 |
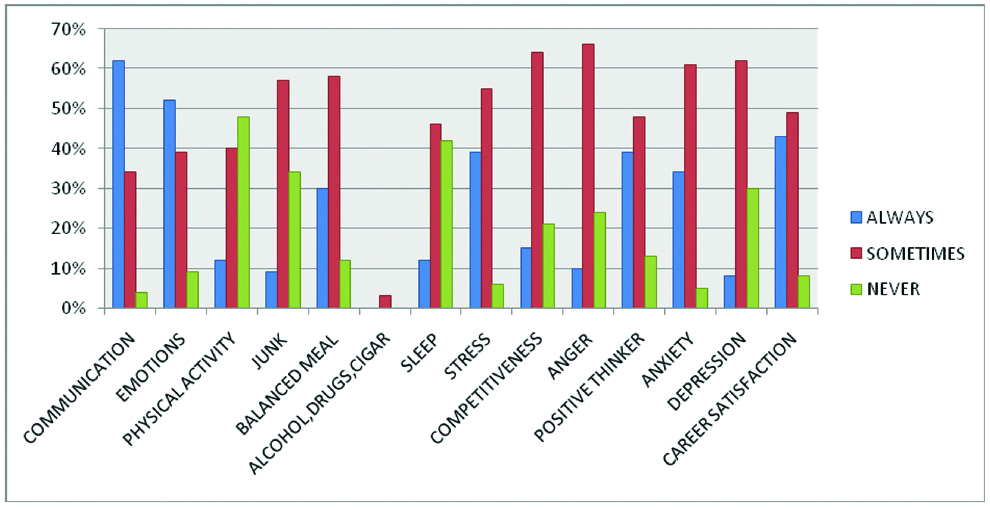
We grouped the students into each category of the various lifestyle parameters opted by them and counted the percentage of students among them which is explained through the bar chart. “Always”, “sometimes” and “never” are the three readings for the parameters and out of this, the highest percentage has been taken to explain the scenario of lifestyle adopted by the students. 62% had good communication skills, 52% were emotionally appreciated, 48% lacked physical activity, 57% sometimes preferred junk foods, 58% had a balanced meal regularly, 3% used either alcohol, drugs or cigarettes, 42% lacked 7-8 hours of sleep, 55% had stress, 64% had competitive personality, 66% has sense of anger most of the time, only 13% had a positive thinking mind, 34% were having anxiety all the time, 8% had depression and 43% had career satisfaction [Table/Fig-2].
Bar chart showing the percentage of various components of lifestyle followed by our students.
In the [Table/Fig-3], demonstrate the cross tabulation between BMI and lifestyle. Of the 72 students belonging to poor lifestyle, group showed 24 students to be overweight/obese, 44 students to be normal and 4 students to be underweight but among 28 students belonging to good lifestyle, 9 students belonged to the overweight/obese category. Here, the lifestyle was found to be influencing BMI but due to the smaller sample size, the significance of this analysis (r=0.062, p-value=0.346) was not achieved.
BMI version Lifestyle cross tabulation.
| n=100 | Lifestyle | Total | p-value |
|---|
| Good | Poor |
|---|
| BMI | Underweight | Count | 4 | 4 | 8 | 0.346 |
| %Within BMI | 50.0% | 50.0% | 100.0% |
| Normal | Count | 15 | 44 | 59 |
| %Within BMI | 25.4% | 74.6% | 100.0% |
| Overweight/Obese | Count | 9 | 24 | 33 |
| %Within BMI | 27.3% | 72.7% | 100.0% |
| Total | Count | 28 | 72 | 100 |
| %Within BMI | 28.0% | 72.0% | 100.0% |
Categorical measurements are presented in number (%). Significance is assessed at 5% level of significance (p<0.05, r=0.062) and Fishers-Exact test was used to find out the p-value.
BMI: Body mass index
In the [Table/Fig-4], describes the cross-tabulation of BFP with lifestyle. Of the 72 students belonging to poor lifestyle group, 31 students have high BFP, 48 students have normal BFP and 1 student had low BFP. Under the good lifestyle category (28 students), 17 students had normal BFP, 3 students had low BFP and 8 students had high BFP. Lifestyle was found to be influencing BFP but due to the smaller sample size, the significance of this analysis (r=0.090, p-value=0.102) was not achieved.
PBF vs. Lifestyle cross tabulation.
| n=100 | Lifestyle | Total | p-value |
|---|
| Good | Poor |
|---|
| BFP | Low | Count | 3 | 1 | 4 | 0.102 |
| %Within Fat% | 75.0% | 25.0% | 100.0% |
| Normal | Count | 17 | 48 | 65 |
| %Within Fat% | 26.2% | 73.8% | 100.0% |
| High | Count | 8 | 23 | 31 |
| %Within Fat% | 25.8% | 74.2% | 100.0% |
| Total | Count | 28 | 72 | 100 |
| %Within Fat% | 28.0% | 72.0% | 100.0% |
Categorical measurements are presented in number (%). Significance is assessed at 5% level of significance (p<0.05, r=0.090) and Fishers-Exact test was used to find out the p-value.
PBF: Percent body fat
[Table/Fig-5] describes the cross tabulation between BMI and BFP. From this table it’s clearly evident that BMI is positively correlated ((r)=0.654) with BFP with p-value=0.000.
BMI vs. BFP cross tabulation.
| n=100 | BFP | Total | p-value |
|---|
| Low | Normal | High |
|---|
| BMI | Underweight | Count | 3 | 5 | 0 | 8 | 0.000* |
| % Within BMI | 37.5% | 62.5% | 0.0% | 100.0% |
| Normal | Count | 1 | 51 | 7 | 59 |
| % Within BMI | 1.7% | 86.4% | 11.9% | 100.0% |
| Overweight/Obese | Count | 0 | 9 | 24 | 33 |
| % Within BMI | 0.0% | 27.3% | 72.7% | 100.0% |
| Total | Count | 4 | 65 | 31 | 100 |
| % Within BMI | 4.0% | 65.0% | 31.0% | 100.0% |
Categorical measurements are presented in number (%). Significance is assessed at 5% level of significance (p<0.05, r=0.654) and Fishers-Exact test was used in this table.
BFP: Body fat percentage; BMI: Body mass index
Discussion
It is already known that poor lifestyle forms the sure pathway for the development of non-communicable diseases [14]. The question we must ask ourselves is “when does a poor lifestyle start affecting the health of our youth?” To answer the question we must first collect information regarding the prevalent lifestyle among our youth. In this regard, the present study was conducted which included youth between the age of 18-25 years who are, in addition, the future health caregivers. The alarming reports by WHO stating that 15 million people aged between 30-70 years die due to non-communicable diseases out of which 23% deaths are premature also fuels the sense of growing urgency to analyse the cause of poor lifestyle in our young population [14].
The [Table/Fig-1], describes the distribution of good and poor lifestyle among the students that shows 72 students having a poor lifestyle and 28 students having the good lifestyle. This data is extremely alarming as we have collected the data during their first semester and expected majority to have a good lifestyle rather than poor lifestyle since the academic overload and stress was yet to begin. These findings were also reported by studies performed by Anand T et al., and Lakshmi Y and Devi BV, [2,7]. We speculate that most of the students had poor lifestyle before they have joined the medical college. Kanikowska D et al., and Baxter SD et al., have reported that many school going children have a poor lifestyle and when they enter into adulthood around 18-29 years, they develop many obstacles for healthy living which ultimately leads to the development of disease trajectories [4,15]. Moreover, Karla S and Unnikrishnan AG, Majeed F, and Alswat KA et al., have pointed out that the transitional period between childhood and adulthood would also affect the energy balance leading to weight gain [1,16,17].
The [Table/Fig-2], demonstrate the percentage of various components of lifestyle followed by the present students using the bar chart. From our study, we found that 48% of the students were sedentary, 42% lack adequate sleep time, 34% had anxiety issue and 13% lack positive thinking which are the main highlights of this chart. Suresh N and Reddy RPL, Bowen L et al., and Barbosa RR et al., to name a few have pointed out similar findings in their studies. The addiction aspect of lifestyle was not found in the present students, however, both the physical and emotional components of lifestyle were found in the students resulting in a negative impact on lifestyle. Inadequate physical activity can be bidirectional that is due to the adoption of sedentary lifestyle leading to low muscle mass with increased fat mass or due to obesity resulting in deteriorating conditions leading to reduced physical activity [5,11,13].
[Table/Fig-3,4] describes the cross-tabulation between BMI and BFP with lifestyle respectively. Out of 72 students leading a poor lifestyle, 24 students were overweight and 23 of the students had high BFP. This tells us that these students are already showing the development of the consequence of a bad lifestyle, which will ultimately make them prone to various detrimental health conditions and diseases like cardiovascular disease, diabetes, sleep apnea, degenerative joint disorders, the list keeps going on. Anand T et al., Lakshmi Y and Devi BV Majeed F, and Pribis P et al., have found out similar findings with increase in the number of students in the overweight and obese category [2,7,16,18]. Due to the consequence of sedentary lifestyle, BFP was found to be high in those people which was described by Kim J, Suresh N and Reddy RPL., Swainson MG et al., and Bowen L et al., [3,5,10,11]. Kanikowska D et al., has highlighted the fact that increasing BMI at the age of 18 years was strongly considered to be a predictive of obesity later in adulthood [4]. It came to author’s notice that few students had low BMI and BFP. Nutrition plays a very important role in our body health which is essential for the prevention of complications such as loss of memory, slow heart rates, decreased hormone production to name a few [7,17]. Many studies have described the relationship between BMI and academics with which nutrition playing a role in it, however Baxter SD et al., and Alswat KA et al., showed no correlation between BMI and academics [15,17]. Lastly, in the present study we found that 59 students had normal BMI out of which 44 students belonged to poor lifestyle and 65 students with normal BFP, 48 students belonged to the poor lifestyle. The explanation of this scenario would probably be that there are other physiological outcomes towards the discrepancy of lifestyle such as gender-specific lipolytic changes, storage and distribution of body fat in the body, psychological distress, dysregulation of stress system, genetic alteration in HOX genes and signalling pathways, which needs to be further investigated as these students are young and imbalance of hormones and other physiological consequences is a normal phenomenon [2,7,17,19].
The [Table/Fig-5] demonstrates the correlation between BMI and BFP. There is a close association between BMI and BFP which was also found in the study of Suresh N and Reddy RPL, Akindele MO et al., and Carpenter CL et al., [5,6,8]. This means that with each increase in BMI there is a proportional increase in BFP and vice versa. However, there is also another concept that needs to be kept in mind about the muscular obesity and invisible obesity. People belonging to muscular obesity are those with higher BMI values with lower BFP [5,18]. Suresh N and Reddy RPL Swainson MG et al., and Pribis P have described similar findings and have highlighted that BMI may be misleading regarding the health status of an individual [5,10,18]. These people cannot be considered as unhealthy since they have increased lean mass and low-fat mass. The weight is mostly due to their muscle build up. People belonging to the invisible obesity group, are those with normal BMI but with higher BFP [5,18]. It is this group that is often neglected due to their lower BMI values and becoming susceptible to the degeneration of health leading to non-communicable diseases in the near future. Hence they require special observation and advice to improve their lifestyle. The point that has to be stressed is that young adults could bring about a change in their lifestyle and practice good health habits sooner than any other age group and would highly benefit them in the future personally as well as professionally. To reset the biological and behavioural carryover effect of good health status from childhood to adulthood can be achieved through the improvement of childhood lifestyle itself. The current study highlights the importance of maintaining BMI and BFP as it has an impact on the quality of lifestyle.
Limitation
Even though present study analyses and provides the important observation that provides vital information about the health status of our young medical students, there are yet many areas to be explored and investigated. The sample size of this study was small; therefore we were not able to achieve the significance we have anticipated. We have not included many other parameters such as gender and the distribution of body fat which could bring a lot of changes in the results of the study. Lastly present students were more of belonging to urban society and the study between rural and urban students can provide more information to the lifestyle pattern practised in both communities.
The lifestyle questionnaire is an important tool to screen those individuals following a poor lifestyle but since it is subjective in nature there can be overestimation or underestimation of the various parameters provided by the questionnaire.
Conclusion
We began the study assuming that present young budding healthcare providers would have a healthy lifestyle, only to find that most of them had already succumbed to a poor lifestyle. Along with academic pressures, a sedentary lifestyle, lack of sleep, anxiety issues and lack of positive thinking, they are on a perfect path for the development of non-communicable diseases. These findings are alarming in the light of the fact that lifestyle is modifiable and therefore its consequences can be altered. Since, BMI and BFP reflect an unhealthy lifestyle as shown in the study, they can be used as a screening tool to identify the early onset of lifestylerelated diseases. Hence, we conclude that an adoption of healthy lifestyle along with periodic monitoring of BMI and BFP would have a positive impact on health status of our population.
Categorical measurements are presented in number (%). Significance is assessed at 5% level of significance (p<0.05, r=0.062) and Fishers-Exact test was used to find out the p-value.
BMI: Body mass index
Categorical measurements are presented in number (%). Significance is assessed at 5% level of significance (p<0.05, r=0.090) and Fishers-Exact test was used to find out the p-value.
PBF: Percent body fat
Categorical measurements are presented in number (%). Significance is assessed at 5% level of significance (p<0.05, r=0.654) and Fishers-Exact test was used in this table.
BFP: Body fat percentage; BMI: Body mass index