Supraclavicular brachial plexus block is the preferred anaesthetic technique for upper limb surgeries which provides complete muscle relaxation, stable intraoperative haemodynamics and smooth transition to postoperative pain relief. Brachial plexus block was first described by Halstead and later improvised by Kulenkempff (the classical supraclavicular approach) and Winnie (the perivascular approach) [1]. The effects of single-injection brachial plexus block dissipate after several hours unmasking the moderate-to-severe pain of the surgical insult. The LA dose can be increased but only to some extent as their therapeutic window is narrow [2]. Thus, the addition of adjuvant not only augments the anaesthetic action of the drug but also reduces the dose required thus improving the safety margin. A variety of perineural adjuvants [3-6] have been tried to hasten the time of onset and prolong the duration of analgesia of nerve blocks with varying degrees of success.
The present study was conducted with the aim of assessing the efficacy adding dexmedetomidine, at two doses of 20 μg and 40 μg, added to 0.5% bupivacaine, in patients posted for upper limb surgeries under supraclavicular brachial plexus block. The secondary outcomes measured were the onset and duration of sensorimotor blockade, haemodynamic variables and adverse events.
Materials and Methods
After approval from the hospital ethical committee (CTRI NO:2014/10/007755) and with patients written consent, 99 American Society of Anaesthesiologists (ASA) physical Status I and II patients, aged 18-60 years, undergoing upper limb surgeries under supraclavicular brachial plexus block, were enrolled in this prospective, randomised controlled study. Patients with diabetes, peripheral neuropathy, with known allergy to local anaesthetics, coagulopathy, infection at the site of block, pregnancy, and patients on beta blockers were excluded from the study.
Assuming, a 45 minutes difference in prolongation of sensory analgesia and taking the power of study at 90% by keeping Type I error (α=0.05) and Type II error (β=0.1), the sample size was calculated as 30 patients in each group. We enrolled 33 patients in each group for the better validation of study results. Patients were randomly allocated by computer generated randomization number into 3 groups. Single blinding was done to avoid bias. The participants were unaware of the group to which they are allocated.
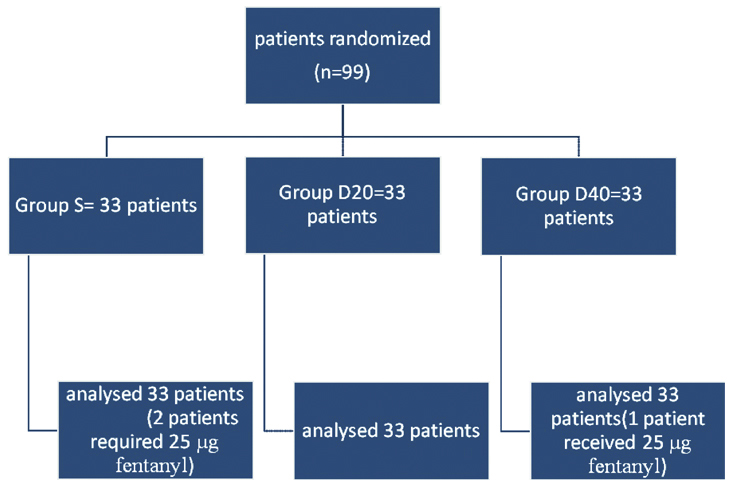
D20 Group: Patients received 25 mL of 0.5% bupivacaine with 20 μg of Dexmeditomidine in 2 mL of NS (total volume 27 mL) D40 Group: Patients received 25 mL of 0.5% bupivacaine with 40 μg of Dexmeditomidine in 2 mL of NS (total volume 27 mL) and S Group: Patients received 25 mL of 0.5% bupivacaine with 2 mL of NS (total volume 27 mL) [Table/Fig-1]. There were no drop outs from the study.
Consort diagram showing the number of patients included and analysed.
After connecting the patients to pre induction monitors, an 18G cannula was secured and oxygen was delivered through the face mask. Under aseptic precautions, supraclavicular brachial plexus block was performed using a B Braun simuplex needle under ultrasound guidance with a linear probe with a frequency of 6-13 Hz and the study drug was deposited into the brachial plexus sheath. Sensory block was assessed by pin prick method every five minutes after drug injections at the dermatomes corresponding to median, radial, ulnar and musculocutaneous nerves. Sensory block was considered complete when the patient experienced complete loss of sensation to pin prick. Sensory block was graded using a three-point scale: Grade 0- sharp pain felt; Grade 1- moderate analgesia, dull pain felt; Grade 2- good analgesia, no sensation. Assessment of motor block was carried out using the three-point scale every five minutes till complete motor blockade was achieved. Motor blockade was assessed using a modified Bromage scale for upper extremities on a three-point scale [10]: Grade 0– normal motor function with full flexion and extension of elbow, wrist and fingers; Grade 1– decreased motor strength with ability to move fingers only; Grade 2– complete motor blockade with inability to move fingers too. When a patient experienced pain in the segments supplied by median, radial, ulnar or the musculocutaneous nerves even after 30 minutes, the block was considered incomplete and supplemented by IV Fentanyl 1 μg/kg and Midazolam 0.04 μg/kg. The block was considered to be a failed block if more than one nerve remained unaffected, in which case general anaesthesia was given and the patient was excluded from the study. Parameters observed were: Duration of sensory blockade and motor blockade (time from local anaesthetic administration to complete recovery of sensory and motor functions), duration of analgesia (time from administration of supraclavicular block to time of first request to analgesics). Rescue analgesics (inj. Tramadol 1-2 mg/kg) was given if Visual Analog Scale was more than 3. Total requirement of tramadol in the first hour was also noted. Patient was observed for any side effects like postoperative nausea and vomiting, bradycardia, hypotension, pruritus, respiratory depression or local anaesthetic toxicity.
For statistical analysis, data were collected and entered in MS Excel 2010. Statistical analysis was performed using SPSS software 18 (SPSS, Inc., Chicago, IL, USA). Interval data are expressed as mean and standard deviation. Statistical analysis was done using ANOVA test and intergroup comparison was done with Bonferoni’s correction. The p-value <0.05% was considered significant.
Results
The average age of the patients was 34.67 years, the youngest being 19 years and oldest being 49 years. The average weight of the patients was 69.18 kg, ranging from 42 kg to 89 kg. The baseline haemodynamic parameters such as heart rate, blood pressure were comparable in all the three groups [Table/Fig-2,3].
| S group | D20 group | D40 group | |
|---|
| Age (years) | 34.67±10.463 | 35.55±13.889 | 34.73±8.289 | p=0.010 |
| Weight (kg) | 69.18±8.199 | 63.52±14.142 | 66.64±13.617 | p=0.177 |
| Gender (M/F) | 28/5 | 24/9 | 25/8 | p=0.468 |
Preoperative haemodynamics.
| Variable | S group | D20 group | D40 group | |
|---|
| Pre op HR | 80.24 (10.494) | 78.36 (14.084) | 80.39 (11.051) | p=0.746 |
| Pre op SBP | 127.39 (13.313) | 126.55 (16.914) | 131.18 (16.183) | p=0.438 |
| Pre op DBP | 80.03 (8.600) | 81.55 (9.563) | 85.70 (10.221) | p=0.47 |
Among the three groups, the onset of sensorimotor blockade was faster in D40 group when compared to D20 and S group. Inter group comparison by Bonferoni’s correction showed a faster onset in D20 group than S group. The duration of sensory blockade and motor blockade was also longer in D40 than in D20 and S groups [Table/Fig-4].
| Variable | Sensory block onset (min) | Motor block onset (min) | Duration of sensory block (hours) | Duration of motor block (hours) |
|---|
| D40 group | 8.94±2.9 | 10.15±2.92 | 14.47±0.97 | 13.09±1.182 |
| D20 group | 14.55±2.89 | 16.97±4.6 | 12.51±1.3 | 11.16±1.25 |
| S group | 21.36±4.37 | 24.55±4.5 | 7.27±1.2 | 6.24±1.22 |
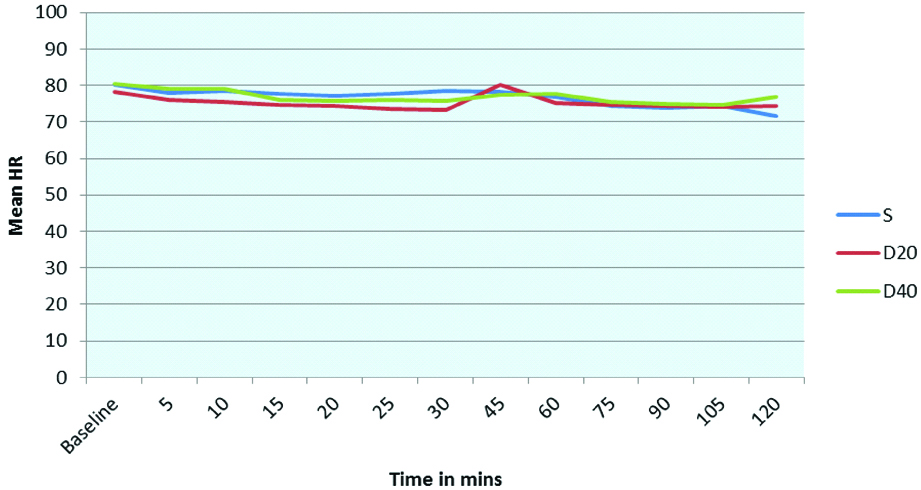
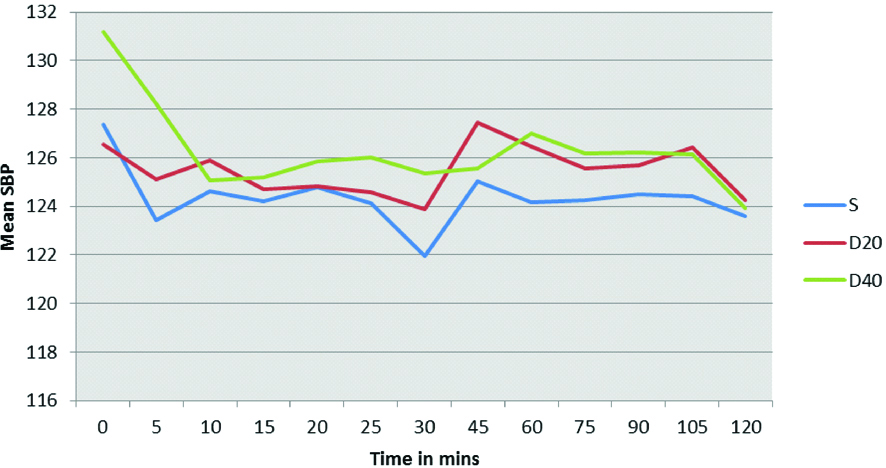
There was no statistically significant difference in the intraoperative haemodynamics such as mean heart rate and blood pressure at 5, 10, 15,20,25, 30,45,60,75,90,105 and 120 minutes among the three groups. A p-value of <0.05 was considered significant [Table/Fig-5,6,7 and 8].
Comparison of mean heart rate among the three groups.
| Time (minutes) | Study groups | p-value |
|---|
| S group | D 20 | D 40 |
|---|
| (Mean±SD) | (Mean±SD) | (Mean±SD) |
|---|
| 5 | 77.94±9.536 | 75.8±13.984 | 79.18±10.457 | 0.501 |
| 10 | 78.45±9.028 | 75.52±13.148 | 78.94±9.028 | 0.369 |
| 15 | 77.73±8.966 | 74.64±13.642 | 76.12±10.136 | 0.529 |
| 20 | 77.2±8.264 | 74.24±13.304 | 75.82±8.988 | 0.514 |
| 25 | 77.2±8.264 | 73.42±13.777 | 75.82±8.988 | 0.268 |
| 30 | 78.42±11.355 | 73.18±13.742 | 75.73±8.776 | 0.184 |
| 45 | 78.12±9.720 | 80.15±9.230 | 77.39±9.497 | 0.475 |
| 60 | 76.73±10.757 | 75.24±9.953 | 77.64±9.813 | 0.888 |
| 75 | 74.27±10.147 | 74.73±8.719 | 75.39±9.287 | 0.630 |
| 90 | 73.76±9.763 | 74.42±8.804 | 74.88±9.086 | 0.884 |
| 105 | 74.48±12.647 | 74.00±8.500 | 74.41±9.883 | 0.952 |
| 120 | 71.67±9.252 | 74.24±10.871 | 76.76±11.667 | 0.157 |
Comparison of mean heart rate among the three groups.
p-value <0.05 is considered statistically significant
Comparison of mean systolic blood pressure between the three groups.
| Time (minutes) | Study groups | p-value |
|---|
| S group | D20 | D 40 |
|---|
| (Mean±SD) | (Mean±SD) | (Mean±SD) |
|---|
| 5 | 123.42±15.900 | 125.12±17.453 | 128.24±16.047 | 0.487 |
| 10 | 124.64±13.397 | 125.06±15.939 | 125.06±15.939 | 0.947 |
| 15 | 124.21±13.131 | 124.70±17.191 | 124.70±17.191 | 0.966 |
| 20 | 124.79±12.789 | 124.82±17.218 | 125.85±14.759 | 0.948 |
| 25 | 124.15±14.036 | 124.58±17.086 | 126.03±14.306 | 0.871 |
| 30 | 123.88±19.705 | 125.36±15.781 | 123.74±17.226 | 0.729 |
| 45 | 125.03±12.496 | 127.45±16.943 | 125.55±11.958 | 0.760 |
| 60 | 124.18±12.413 | 126.45±16.000 | 127 .00±12.867 | 0.682 |
| 75 | 124.27±12.598 | 125.55±15.863 | 126.18±12.131 | 0.846 |
| 90 | 124.27±12.598 | 125.55±15.863 | 125.55±15.863 | 0.846 |
| 105 | 124.42±12.199 | 124.42±12.199 | 126.42±15.732 | 0.819 |
| 120 | 123.58±15.264 | 124.27±19.504 | 123.92±13.724 | 0.985 |
Comparison of mean systolic blood pressure between the three groups.
p-value<0.05 is considered statistically significant
No patients required tramadol for pain relief in the first hour. There was no incidence of postoperative nausea and vomiting, hypotension, bradycardia, pruritus, respiratory depression or local anaesthetic toxicity.
Discussion
Brachial plexus block is a preferred anaesthetic technique for forearm and hand pathologies. Although peripheral nerve stimulator was considered gold standard to locate the peripheral nerves, the introduction of ultrasound guided nerve blocks had gained immense popularity and interest [11]. Among all the adjuvants, α2 agonist has shown a promising effect in quickening the onset of blockade and prolonging the block [12]. There have been four proposed mechanism of action of α2 agonist on the peripheral nerve. They are centrally mediated analgesia, α2 mediated vasoconstrictive effects, attenuation of inflammatory response and direct action on peripheral nerves [5]. Dalle C et al., had proposed that α2 agonists, by enhancing activity dependent hyperpolarization generated by Na/K pump during repetitive stimulation, increases the threshold for initiating action potential causing blockade of conduction [13]. Kosugi T et al., in their study found Dexmeditomidine in high concentrations, inhibit CAPs in frog sciatic nerves without α2adrenoreceptor activation. Also, Dexmeditomidine decreased the peak amplitude of CAPs reversibly and in a concentration dependent manner. Their action was not antagonized with α2 adrenoreceptor antagonist like Yohimbine and Atipamezole [14]. In a randomized double blind controlled study done by Swami SS et al., on 60 ASA I and II patients posted for upper limb surgeries, Dexmeditomidine at 1 μg/kg enhanced the duration of analgesia when compared to clonidine at 1 μg/kg. The time for rescue analgesia was also prolonged in the Dexmeditomidine group [12].
Onset of Sensorimotor Blockade
In our study, sensory blockade was assessed by loss of pin prick sensation. Among the three groups, D40 group where 40 μg of Dexmeditomidine had a faster onset of sensory blockade (8.99 min) when compared to D20 group where 20 μg of Dexmeditomidine was used (14.55 minutes) and S group where saline was used (21.36 minutes). Intergroup comparison between D40 and D20 showed a faster onset of sensory block in D40 group then D20 group. Motor blockade was assessed by modified bromage scale every five minutes. The onset of motor blockade was 24.55 minutes, 16.97 minutes and 10.15 minutes in S group, D20 group and D40 groups respectively. In the study conducted by Nallam SR et al., where two doses of Dexmeditomidine 50 μg/kg and 100 μg/kg were added to Levobupivacaine also showed higher doses of Dexmeditomidine hastens the onset of sensorimotor blockade [15]. Kaygusuz K et al., in his study had used Dexmeditomidine in the dose of 1 μg/kg as an adjuvant to Levobupivacaine to shorten the onset of sensorimotor blockade [16]. We conclude that the onset of sensorimotor blockade was faster when Dexmeditomidine was used as an adjuvant and it was dose dependent.
Duration of Sensorimotor Blockade and Analgesia
We observed that the total duration of effective sensory blockade in D40, D20 and S group were 14.47 hours, 12.52 hours and 7.27 hours, respectively. Also, the total duration of motor blockade lasted for 13 hours in D40 groups compared to 11 hours in D20 groups and 6 hours in S group. Increasing the dose of Dexmeditomidine from 20 μg to 40 μg had not only fastened the onset of sensorimotor blockade but also resulted in a longer pain free period. Agarwal S et al., had concluded in their study that Dexmeditomidine as an adjuvant to bupivacaine in brachial plexus block prolongs the duration of sensorimotor blockade and analgesia thereby [17]. Kathuria et al., in his study proved that the actions of Dexmeditomidine were probably local than central [18].
Haemodynamic Changes
In our study, the intraoperative haemodynamic parameters like heart rate, blood pressure were recorded and analysed. All the three groups showed a stable haemodynamics and there was no incidence of bradycardia or hypotension in any of the three groups. Agarwal S et al., also had observed that there was no incidence of bradycardia or hypotension when he compared Dexmeditomidine at a dose of 100 μg was used as an adjuvant to 0.375% bupivacaine in supraclavicular brachial plexus block [17]. In another study conducted by Zhang Y et al., Dexmeditomidine as an adjuvant to ropivacaine in axillary brachial plexus block in doses of 100 μg had shown bradycardia and hypotension. This could have been because of the relatively larger doses of Dexmeditomidine [7].
Conclusion
From the results of the present study, we conclude that 40 μg of Dexmeditomidine produces a faster onset of blockade and prolongs the duration of postoperative analgesia compared to 20 μg of Dexmeditomidine without any side effects.