The ‘Laterally Inverted’ Laparoscopic Cholecystectomy: Unlearning the Learning Curve Helps, but Old Habits Die Hard
Sukumar Santosh Kumar1, Anamika Sinha2
1 Professor, Department of Surgery, Base Hospital and ACMS, Delhi Cantt, New Delhi, India.
2 Associate Professor, Department of Pathology, Base Hospital and ACMS, Delhi Cantt, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sukumar Santosh Kumar, Professor, Department of Surgery, Base Hospital and ACMS, Delhi Cantt-110010, New Delhi, India.
E-mail: sskumar9169@gmail.com
Situs Inversus is a rare condition (1 in 5000-10000 hospital admissions) and Laparoscopic Cholecystectomy (LC) for symptomatic gallstones in such patients is even rarer. Only about 70 cases have been reported so far. This otherwise commonly performed surgery takes on a whole new avatar due to the unique challenges of disorientation induced by the ‘mirror image’ positioning of the viscera and its attendant ergonomic difficulties. The instincts and habits acquired by a laparoscopic surgeon after climbing the learning curve, though definitely an advantage in this situation, can serve as a handicap as well. Our experience of managing such a case is presented in this article.
Gallstones, Mirror image, Risk factors, Technique, Situs Inversus
Case History
A 34-year-old lady had reported to the Surgery Outpatient Department of a zonal hospital of Indian Armed Forces Medical Services (IAFMS) with recurrent epigastric pain of two months duration. There was no associated history of jaundice. Abdominal ultrasonography done at that hospital revealed Situs Inversus Totalis (SIT) with liver and gallbladder on left side and dextrocardia. The gallbladder showed ‘wall echo shadow’ complex, suggestive of chronic calculous cholecystitis. The common bile duct and intrahepatic biliary radicals were not dilated. She was advised Open Cholecystectomy by the surgeon as Laparoscopic Cholecystectomy (LC) was deemed technically challenging. However, she reported to the Surgical Gastroenterology Department of our hospital, a tertiary care hospital of IAFMS. Abdominal examination revealed a midline infraumbilical surgical scar of previous caesarean section. All laboratory parameters including the liver function tests were normal. Magnetic Resonance Imaging done at this hospital showed SIT with chronic calculous cholecystitis and no biliary tree anomalies. She underwent pre-anaesthetic assessment and was taken up for LC.
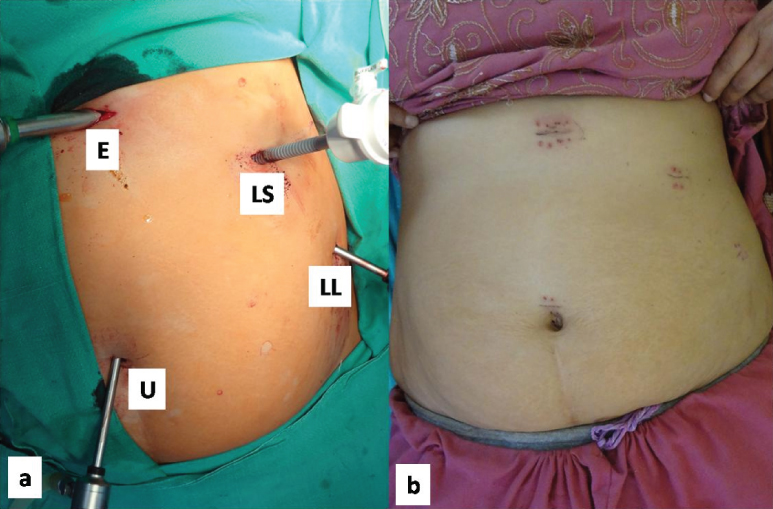
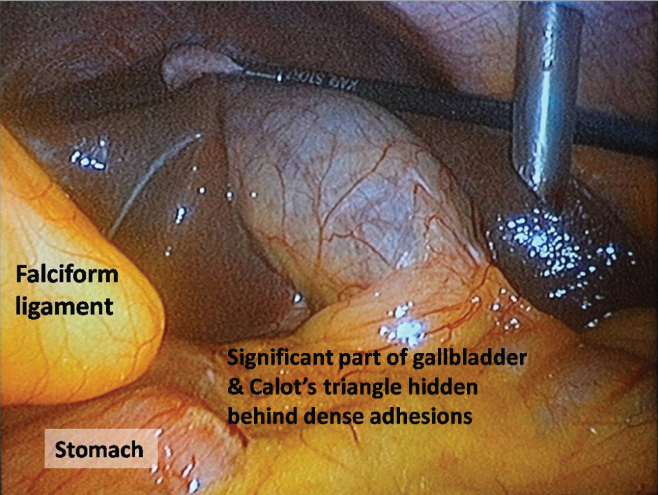
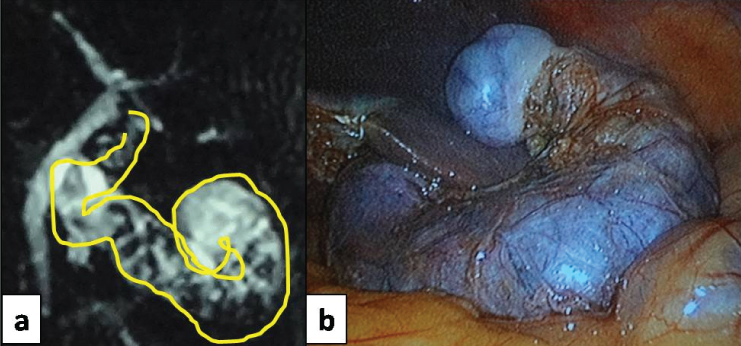
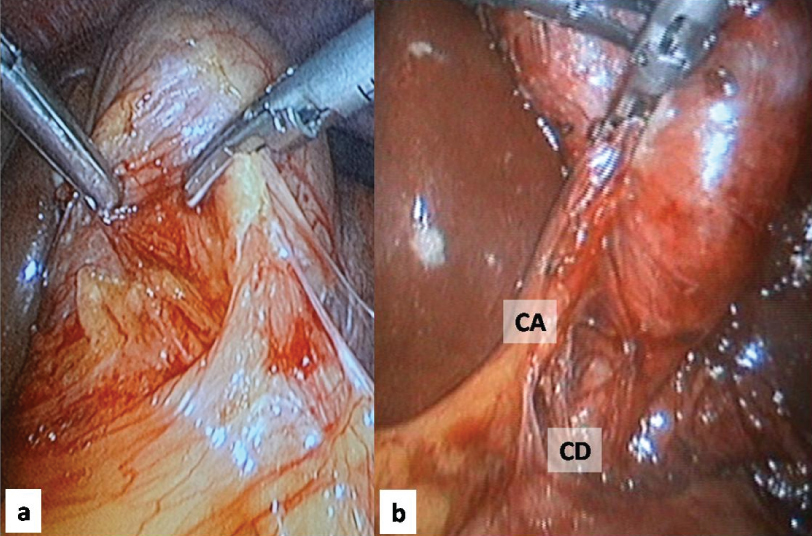
The operating room setup was arranged in a ‘mirror image’ fashion in relation to the position used in standard LC. The surgeon and the camera holding assistant stood on the right side of the patient, while the assistant with the instrument trolley stood on the left. ‘Mirror image’ positioning of the usual 4-port technique was done – one 5-mm camera port (umbilical), one 10-mm port (epigastric) and two 5-mm ports (left subcostal and left lumbar) [Table/Fig-1]. Laparoscopy revealed the Situs Inversus positioning of the organs [Table/Fig-2]. The gallbladder was long and serpentine; and packed with multiple stones, it was adherent to the duodenum, hepatic flexure of colon and the omentum [Table/Fig-2,3]. The Calot’s triangle also had multiple adhesions. The surgeon was right-handed, and most part of the surgery, especially the division of the adhesions, was done with the dominant hand through the left subcostal port while using the epigastric port for traction [Table/Fig-4]. This reversal was done to avoid crossing of the hands but the orientation was the opposite of what is encountered during LC on normally sited gallbladder. It took some effort to get re-oriented to the ‘laterally inverted’ anatomy. The left lumbar port was mostly used for traction on the fundus of the gallbladder, but as lot of dense adhesions were encountered, instruments were interchanged in the ports as per the changing orientation. However, dissection in the Calot’s triangle and clipping of the cystic duct and artery were performed through the epigastric port by the surgeon’s non-dominant left hand. This tested the ambidexterity of the surgeon as he also had to ensure that the clips were secure. The gallbladder was separated from its bed by electrocautery and then extracted through the epigastric port. The total operation time was 120 minutes and the blood loss was minimal.
a) ‘Mirror image’ placement of ports, E–Epigastric 10 mm port, U–Umbilical 5 mm camera port, LS–Left Subcostal 5 mm port, LL–Left Lumbar 5 mm port; b) Port site wounds after removal of skin staples.
Laparoscopic view of the left sided gallbladder and Situs Inversus, only part of gallbladder is visible as the rest is covered by adhesions.
a) Magnetic Resonance Cholangiographic image of the long, serpentine left sided gallbladder; b) Laparoscopic view of the same, just before extraction.
a) Adhesiolysis being done with Ultrasonic Scalpel introduced through the left subcostal port; b) View of Calot’s Triangle after adhesiolysis.
CD: Cystic Duct; CA: Cystic Artery
The patient recovered well. On her request, her discharge was deferred till removal of skin staples, as she lived in a remote area. She was asymptomatic on follow up.
Discussion
Gallstone disease is a major cause of morbidity and mortality worldwide and LC is considered the ‘gold standard’ for treating symptomatic gallstones [1]. LC, after its introduction in 1987, has gone on to become an extensively performed surgery globally; but it continues to be associated with the major morbidity of bile duct injury [2]. Various patient related factors have been evaluated that can predict a difficult LC preoperatively [3]. However, finding the viscera itself laterally inverted like a ‘mirror image’ can be a unique challenge to any laparoscopic surgeon.
Lateral transposition of viscera or ‘Situs Inversus’ is a congenital anomaly and is rarely encountered in surgical practice. SIT is a condition when both the abdominal and thoracic viscera are laterally inverted and the reported incidence is one in 10000-20000 births or one in 5000-10000 hospital admissions [4,5]. The exact aetiology is still not clear but it can be caused by a single autosomal recessive gene with incomplete penetration, or an X linked mutation [6]. The person is usually asymptomatic but may harbour various anomalies, some of which may be life-threatening [7]. Patients with Situs Inversus who are scheduled for surgery should be assessed preoperatively for any potentially serious cardiac or respiratory abnormalities.
There is no reported predisposition to gallstones in these patients [4]. However, as SIT is an uncommon entity and the patient is usually unaware of the condition, the clinical presentation of patients with gallstones may be misleading. The presentation with left upper abdominal pain may delay the diagnosis of gallstones [8]. About 30% of patients with Situs Inversus having symptomatic gallstones present with epigastric pain and 10% of patients may present with pain on the right side [9].
Cholecystectomy in SIT is uncommon and has only been reported in occasional case reports or small series [7,10]. In the pre-laparoscopic era, less than 40 ‘open’ cholecystectomies in Situs Inversus were published [7]. Since Campos and Sipes reported the first successful LC in a Situs Inversus patient in 1991, another 70 cases have been recorded in the literature [10]. However, no such case has been reported from the IAFMS so far.
Our experience showed us that the ‘mirror image’ like orientation while operating on a left sided gallbladder can be challenging for a laparoscopic surgeon as his brain is already ‘wired’ in a certain way after doing hundreds of LC on the regular right sided gallbladders. He has to actually unlearn this ‘learning curve’ and consciously work against his habitual thinking associated with a conventional LC. He has to be dextrous enough to reorient his ‘hand-eye co-ordination’ to the altered field and also should be prompt in dealing with any developing difficult intraoperative situation which can be potentially harmful. In addition, he has to introduce some modifications in operation theatre arrangement and position of the surgical team.
A ‘mirror image’ positioning of the surgical team and the laparoscopy ports are recommended [4]. This orientation may require entire dissection to be performed with one‘s left hand, but this may be easier for a left-handed surgeon [7]. However, a right-handed surgeon, who is standing on the right side of the patient, may have to cross his hands so as to allow his right hand to operate through the epigastric port; or he may use the assistant to retract the Hartmann’s pouch from the left side to allow him to work in a more ergonomic position [7]. The surgeon may use the epigastric port to retract with his left hand and operate with the right hand through the left subcostal port, as was done, for the most part, in our case [7]. Alternatively, the surgeon may stand between the abducted legs of the patient (the French position) and operate [7].
Although, there is no evidence to suggest that there is a higher risk of bile duct injuries in these patients, the operation time tends to be longer due to the challenges involving orientation and ergonomics [4]. Nonetheless, no conversion to open surgery has been reported so far [10]. This could be either due to special care taken while carrying out the laparoscopic surgery or more likely due to the authors’ tendency to report only successful cases in such a challenging situation. However, it is needless to state that conversion to open surgery should always be an option, in the interest of patient safety.
Conclusion
The rarity of presentation of SIT, coupled with the technical challenge posed by the ‘mirror image’ anatomy, places a special demand on the skills of any laparoscopic surgeon. Not with standing this, LC for symptomatic gallstones in patients with Situs Inversus can be done safely if performed by an experienced laparoscopic surgeon.
[1]. Gollan JL, Bulkley GB, Diehl AM, Elashoff JD, Federle MP, Hogan WJ, Gallstones and laparoscopic cholecystectomyJAMA 1993 269(8):1018-24.10.1001/jama.1993.03500080066034 [Google Scholar] [CrossRef]
[2]. Pucher PH, Brunt LM, Davies N, Linsk A, Munshi A, Rodriguez HA, Outcome trends and safety measures after 30 years of laparoscopic cholecystectomy: a systematic review and pooled data analysisSurg Endosc 2018 32(5):2175-83.10.1007/s00464-017-5974-229556977 [Google Scholar] [CrossRef] [PubMed]
[3]. Kulkarni SV, Kumar SS, Preoperative predictors of a difficult laparoscopic cholecystectomyInt Surg J 2018 5:608-13.10.18203/2349-2902.isj20180362 [Google Scholar] [CrossRef]
[4]. Salama IA, Abdullah MH, Houseni M, Laparoscopic cholecystectomy in situs inversus totalis: Feasibility and review of literatureInt J Surg Case Rep 2013 4(8):711-15.10.1016/j.ijscr.2013.02.03023810920 [Google Scholar] [CrossRef] [PubMed]
[5]. Kamitani S, Tsutamoto Y, Hanasawa K, Tani T, Laparoscopic cholecystectomy in situs inversus totalis with “inferior” cystic artery: A case reportWorld J Gastroenterol 2005 11(33):5232-34. [Google Scholar]
[6]. Splitt MP, Burn J, Goodship J, Defects in the determination of left-right asymmetryJ Med Genet 1996 33(6):498-503.10.1136/jmg.33.6.4988782051 [Google Scholar] [CrossRef] [PubMed]
[7]. Kumar S, Fusai G, Laparoscopic cholecystectomy in situs inversus totalis with left sided gall bladderAnn R Coll Surg Engl 2007 89(2):W16-W18.10.1308/147870807X16046117346394 [Google Scholar] [CrossRef] [PubMed]
[8]. Borgaonkar VD, Deshpande SS, Kulkarni VV, Laparoscopic cholecystectomy and appendicectomy in situs inversus totalis: A case report and review of literatureJ Minim Access Surg 2011 7(4):242-45.10.4103/0972-9941.8564922022115 [Google Scholar] [CrossRef] [PubMed]
[9]. Hall TC, Barandiaran J, Perry EP, Laparoscopic cholecystectomy in situs inversus totalis: is it safe?Ann R Coll Surg Engl 2010 92(5):e30-e32.10.1308/147870810X1269966298027720529478 [Google Scholar] [CrossRef] [PubMed]
[10]. Ren JJ, Li SD, Geng YJ, Xiao R, Modified laparoscopic cholecystectomy technique for treatment of situs inversus totalis: A case reportJ Int Med Res 2017 45(3):126-67.10.1177/030006051770325828417652 [Google Scholar] [CrossRef] [PubMed]