Subcutaneous Cryptococcosis Mimicking Cold Abscess
Ranjeev Bhagat1, Vinisha Bansal2, Uma Handa3, Reetu Kundu4, Jagdish Chander5
1 Assistant Professor, Department of Pathology, Govt Medical College and Hospital, Sec 32, Chandigarh, India.
2 Senior Resident, Department of Pathology, Govt Medical College and Hospital, Sec 32, Chandigarh, India.
3 Professor, Department of Pathology, Govt Medical College and Hospital, Sec 32, Chandigarh, India.
4 Assistant Professor, Department of Pathology, Govt Medical College and Hospital, Sec 32, Chandigarh, India.
5 Professor, Department of Microbiology, Govt Medical College and Hospital, Sec 32, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjeev Bhagat, Department of Pathology, level 3 E block Govt Medical College and Hospital, Sec 32, Chandigarh-160030, India.
E-mail: ranjeevbhagat@gmail.com
Cryptococcosis is a fungal infection caused by the yeast belonging to the Cryptococcus species which includes broadly two categories Cryptococcus neoformans and Cryptococcus gattii. It most commonly affects the lungs and central nervous system, particularly in immunocompromised patients. Other sites of dissemination include skin, ends of long bones, joints, liver, spleen, kidneys, prostate and other tissues. A 32-year-old male patient came to surgical OPD with complaints of a right posterior thigh swelling extending up to knee measuring approximately 8x6 cm. There was a past history of receiving Anti-Tubercular Treatment (ATT) for three months but without any improvement in symptoms. MRI of the thigh suggested a possibility of cold abscess or chronic haematoma. Fine Needle Aspiration Cytology (FNAC) of the thigh showed numerous spherical encapsulated yeast cells with only few macrophages in the background. Special stains like Periodic Acid–Schiff (PAS) highlighted the fungus while mucicarmine highlighted the capsule of fungi. Ziehl Neelsen stain for acid fast bacilli was negative. A final cytological diagnosis of cryptococcosis was given which was confirmed by the culture reports. In developing countries like India where there is high incidence of tuberculosis, fungal infection like cryptococcosis is likely to be missed particularly if high index of clinical suspicion for tuberculosis is present.
Cytological, Capsule, Immunocompromised, Tuberculosis
Case Report
A 32-year-old male patient came to surgical OPD with the complaint of large right posterior thigh swelling extending up to knee for the last 10 days. The swelling was progressively increasing in size and was associated with pain and difficultly in walking. The overlying skin was slightly tense with prominent veins [Table/Fig-1]. There was history of low grade fever and cough for which he was given a trial of anti tubercular treatment for three months; however his symptoms were not relieved. Subsequently patient developed a large swelling on thigh after the trial for which he was investigated in our institute.
Large thigh swelling with cverlying tense skin.

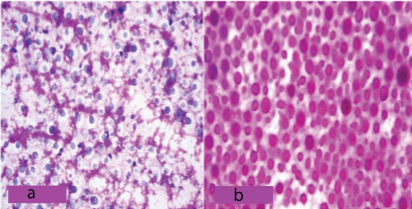
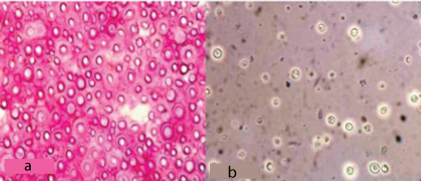
MRI thigh swelling showed a large solid collection with partial liquefaction, measuring 10×9×3.5 cm. A possibility of cold abscess or chronic haematoma was suggested. FNAC of the thigh yielded 5 ml of straw coloured fluid. Smears prepared from the fluid showed numerous spherical encapsulated yeast cells with only occasional macrophages in the background [Table/Fig-2a]. Special stains like PAS highlighted the fungus [Table/Fig-2b] while Mucicarmine and India ink highlighted the capsule of fungi [Table/Fig-3]. Ziehl Neelsen stain for acid fast bacilli was negative.
a) Numerous spherical encapsulated yeast cells seen on FNAC smear (H&E 100X); b) Highlighted on PAS stain (PAS 400X).
a) Capsule of cryptocouus highlighted on Mucicarmine stain (Mucicarmine 400X); b) Capsule highlighted on India ink preperation (India ink 400X).
A final cytological diagnosis of cryptococcosis was given which was confirmed by the culture reports which showed growth of Cryptococcus. Further genotyping confirmed it to be Cryptococcusgattii. There was no evidence of acquired immune deficiency as the patient was non diabetic and his HIV status was non-reactive as confirmed by the Coomb’s test followed by rapid test trispot method. Since the patient had anti-tubercular treatment for three months, he was referred to clinician for further management. Clinical re-evaluation of the patient indicated that the previous diagnosis of pulmonary tuberculosis was never confirmed and it was purely a therapeutic trial. Patient also developed a large swelling on thigh after three months of uninterrupted treatment for tuberculosis. So it was assumed that the patient might be a case of a primary pulmonary cryptococcosis which was misinterpreted as tuberculosis.
Patient was put on anti fungal drugs and was advised workup for primary immune deficiency, however patient never came back for follow-up.
Discussion
Cryptococcosis is a fungal infection caused by the yeast of the Cryptococcus species which includes broadly two categories Cryptococcus neoformans (which is further divided into var. neoformans and var. grubii) and Cryptococcus gattii [1]. It can cause disease in any organ of the body but most commonly affects the lungs and central nervous system, particularly in immunocompromised patients [2].
Cryptococcus neoformans var. grubii is the most common cause of human cryptococcosis worldwide which accounts for more than 95% of total cryptococcal cases. Majority of the patient infected by C. neoformans are immunocompromised while C. gatti causes infection in immunocompetent persons also [3,4].
Subcutaneous cryptococcosis can be primary which is very rare or secondary from other primary source like lung or CNS. Cutaneous involvement may either be due to direct contact or by dissemination from the primary site of infection. Occasionally, it may be the only presentation of a disseminated disease in some cases. So a case of cutaneous cryptococcosis should be thoroughly evaluated to rule out a systemic cause of cryptococcosis [5].
A survey conducted by the French cryptococcosis study group concluded that among 28 cases of primary cutaneous cryptococccosis, 50% were immune-competent and only 11% had HIV infection, suggesting that primary cutaneous cryptococcosis can develop regardless of immune status [6].
FNAC is a quick and easy method to diagnose cryptococcosis as the organisms are easily seen on routine cytological stains and can be highlighted by special stains like PAS, Mucicarmine and India ink. A case of cryptococcosis involving multiple lymph nodes was reported in a young male and was clinically suspected to be tuberculosis. FNAC of the lymph nodes showed epithelioid cell clusters with numerous budding yeast cells. The capsule was highlighted by Periodic Acid Schiff and Mucicarmine stain. Ziehl Neelsen staining did not reveal any acid-fast bacilli, ruling out any coexisting tuberculous infection [7].
Cases of pulmonary cryptococcosis are usually underdiagnosed because of highly variable clinical presentation. In countries where tuberculosis is endemic disease, it can easily be misdiagnosed as tuberculosis as there is high degree of overlap in clinical, laboratory and radiographic presentation. In equivocal cases fungal culture or molecular identification is required [8].
Conclusion
In developing countries like India where there is high incidence of tuberculosis, fungal infection like cryptococcosis is likely to be missed particularly if high index of clinical suspicion for tuberculosis is present. This case highlights the fact that before starting the therapeutic trial of anti tubercular treatment, the diagnosis should confirmed by all the available investigations.
[1]. Lin X, Heitman J, The biology of the Cryptococcus neoformans species complexAnnu Rev Microbiol 2006 60:69-105.10.1146/annurev.micro.60.080805.14210216704346 [Google Scholar] [CrossRef] [PubMed]
[2]. Chayakulkeeree M, Perfect JR, CryptococcosisInfect Dis Clin North Am 2006 20:507-544.10.1016/j.idc.2006.07.00116984867 [Google Scholar] [CrossRef] [PubMed]
[3]. Bennett JE, Kwon-Chung KJ, Howard DH, Epidemiologic differences among serotypes of Cryptococcus neoformansAm J Epidemiol 1977 105(6):582-86.10.1093/oxfordjournals.aje.a112423326036 [Google Scholar] [CrossRef] [PubMed]
[4]. Kwon-Chung KJ, Bennett JE, Epidemiologic differences between the two varieties of Cryptococcus neoformansAm J Epidemiol 1984 120(1):123-30.10.1093/oxfordjournals.aje.a1138616377880 [Google Scholar] [CrossRef] [PubMed]
[5]. Pan B, Chen M, Jia H, Pan W, Liao W, Multiple subcutaneous abscesses: A rare presentation of cutaneous cryptococcosisIndian J Dermatol Venereol Leprol 2013 79:118-19.10.4103/0378-6323.10468723254747 [Google Scholar] [CrossRef] [PubMed]
[6]. Neuville S, Dromer F, Morin O, Dupont B, Ronin O, Lortholary O, Primary cutaneous cryptococcosis: a distinct clinical entityClinical Infectious Diseases 2003 36(3):337-47.10.1086/34595612539076 [Google Scholar] [CrossRef] [PubMed]
[7]. Manjunath GV, Sheeladevi CS, Suchitha S, Sunila R, Fine needle aspiration diagnosis of cryptococcal lymphadenitis: A window of opportunityJournal of Cytology 2008 25(4):147-49.10.4103/0970-9371.50801 [Google Scholar] [CrossRef]
[8]. Naima F, Kauser J, Tazeen F, Rashida A, Ali B, Afia Z, Pulmonary cryptococcosis mimicking tuberculosis in an immunocompetent hostAsian Pacific J of Tropical Disease 2015 5(1):S114-15.10.1016/S2222-1808(15)60870-2 [Google Scholar] [CrossRef]