Heterotrophic Calcifications (HC’s) are often encountered as incidental findings in dental radiographic examinations. Inexperienced clinicians may misdiagnose these tame calcifications and levy unnecessary treatments to patients. Awareness and information regarding the prevalence and the nature of these calcifications are necessary to interpret any dental radiographic examination. We are reporting one such incidental finding of HC in right submandibular region of a 65-year-old patient in Cone Beam Computed Tomography (CBCT) and Orthopantomographic (OPG) evaluation.
Heterotrophic calcifications, Lymphnode, Orthopantomogram
Case History
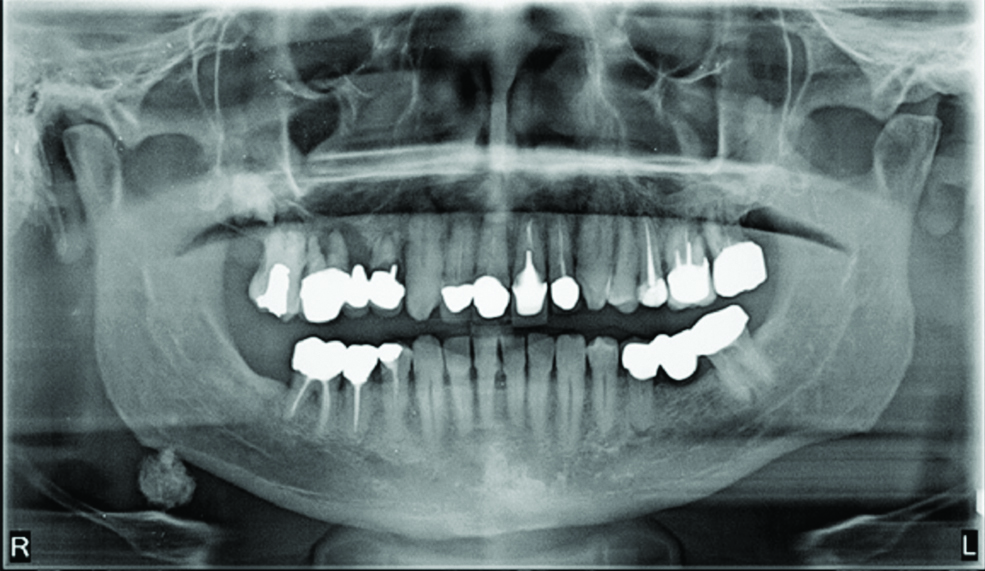
A 65-year-old patient was referred from a private dental clinic for radiographic evaluation prior to surgical implant placement. Patient had a history of tuberculosis and was treated for the same ten years ago. The patient was advised OPG and CBCT examination. During the radiographic evaluation of both the OPG (Planmeca, Promax, Finland, with the voltage of 66 kV, current of 9 mA and the minimum exposure time of 16s) and CBCT volumetric data an incidental finding was observed. The incidental finding in OPG revealed the presence of a unilateral, solitary heterogeneous radiopaque mass in the right submandibular region, inferior to the antegonial notch, with a well defined, irregular and lobulated or cauliflower like outline. Radiolucent serrations in the radiopaque mass were evident. The superior aspect of mass seemed attached to the antegonial notch of mandible [Table/Fig-1].
OPG revealing HC in right submandibular region.
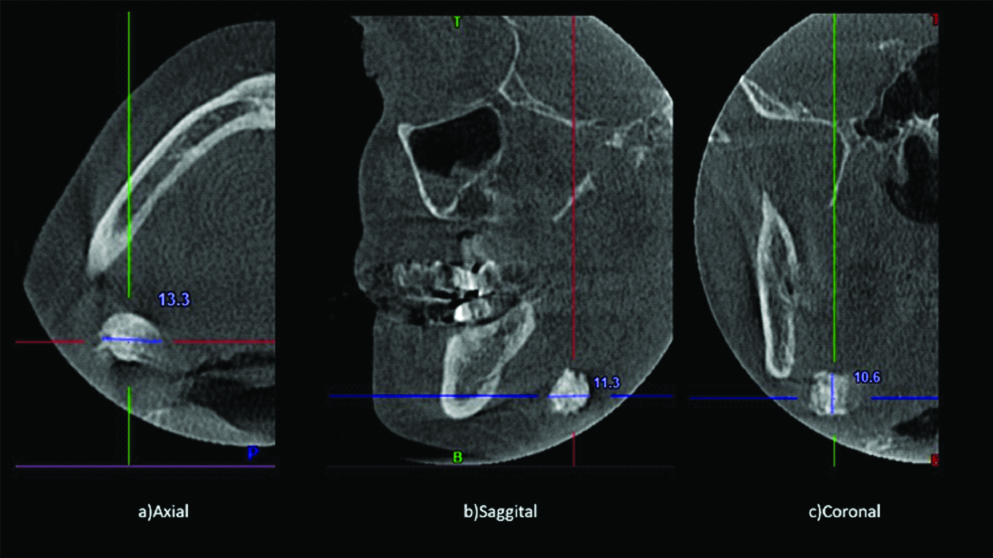
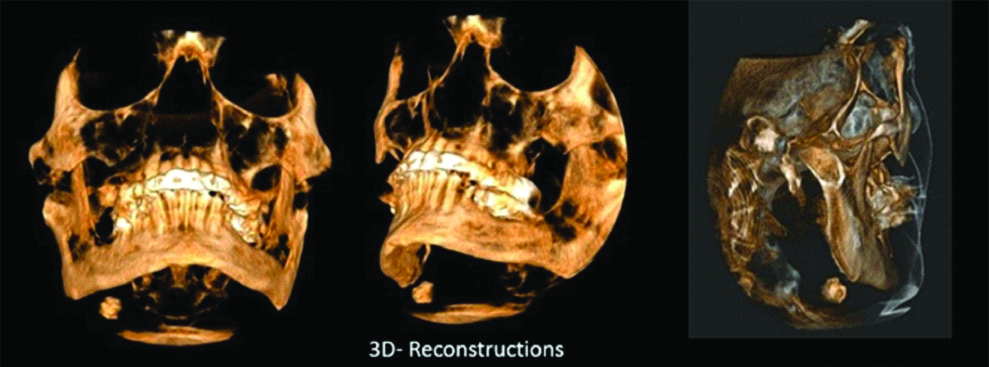
CBCT volumetric data was taken (using SkyView CBCT scanner (MyRay, Imola, Italy), with an exposure settings of 90 kVp, 92 mAs and Large FOV) that confirmed the presence of same, measuring 10.6×13.3×11.3 mm [Table/Fig-2]. CBCT rendered three-dimensional clarity relating to position of the mass; evident in the right submandibular region; inferior to the antegonial notch; above the hyoid and between posterior border of ramus; and cervical vertebrae. The mass was evident in all the three orthogonal planes and seemed detached from the hard tissue structure of craniofacial region [Table/Fig-3].
Cropped axial, saggital and coronal planes depicting HC.
3D-CBCT reconstructed views.
Submandibular lymph node calcification, submandibular sialolith or remotely phlebolith were the suspected differential diagnosis. Sialolith has a uniform smooth outline compared to the irregular outline in the present case. Phleboliths are relatively smaller and have concentric radiopaque and radiolucent rings also known as bull’s eye or target appearance, their shape mimics a portion of blood vessel typically seen as straight or slightly curved sausages. Thus, ruling out sialolith and phlebolith, concluding with radiographic diagnosis of submandibular lymph node calcification [1].
Discussion
Deposition of calcium salts, primarily calcium phosphate, usually occurs in hard tissues, but when deposited extra-skeletally in an unorganised manner they are termed as HC’s [1]. HC’s are classified into three types namely Dystrophic, Idiopathic and Metastatic calcifications.
Dystrophic calcification refers to calcification in dead tissues despite normal serum calcium and phosphate levels. Idiopathic calcification occurs in normal tissues despite normal serum calcium and phosphate levels. Metastatic calcification refers to calcification occurring in normal tissues as a result of abnormal serum calcium and phosphate levels, e.g., Hyperparathyroidism.
HC’s may develop in a wide variety of unrelated disorders and degenerative processes, may not cause significant signs or symptoms. Frequently detected as incidental findings during radiographic examination. Some HC’s require no intervention or supervision, whereas others might be life-threatening and mandates immediate attention [1].
HC’s are visible on about 4% of panoramic radiographs (OPG) [1,2]. Correct identification in two dimensional radiographs are difficult due to superimposition of structures, especially to locate whether the calcification lies within or adjacent to the bony or soft tissue landmark [3].
Accurate identification of HC’s necessitates thorough knowledge of the hard and soft tissue anatomies and associated positions, to treat the underlying conditions and adopt necessary referrals.
HC’s in lymph nodes falls under dystrophic calcification. Chronically inflamed lymphoid tissues due to various disease gets replaced by calcium salts eventually effacing the nodal architecture [1,2]. Lymph nodal calcifications entails either active or previously treated disease.
Dystrophic lymph nodal calcifications have been frequently associated with granulomatous disorders or chronic inflammation related to various diseases. Tuberculosis was most common disease causing lymph nodal calcification; other well known causes may include Bacille Calmette-Guérin vaccination, sarcoidosis, cat-scratch disease, rheumatoid arthritis systemic sclerosis, post-treated lymphomas, fungal infections and malignancies [1]. The present case had history of tuberculosis and was treated for same in the past.
Cervical lymph node calcification is a rare condition, often encountered on a routine panoramic survey. The differentials for submandibular lymph node calcification include submandibular sialolith and phlebolith. Submandibular lymph nodes are the third most common group involved, after upper deep jugular and jugulo-omohyoid nodes [4]. The present case showed involvement of the submandibular region. Calcifications may affect a solitary node or a linear series of nodes, termed as lymph node “chaining”. Present case showed involvement of a solitary node [1].
Variable radiodensities of calcified lymph nodes have been reported, they may be radiopaque, laminated, or may show both radiopaque cum radiolucent areas and resembles a cauliflower shape, which was also appreciated in the present case [5,6].
One percent of 2300 neck Computed Tomographic (CT) scans have revealed cervical lymph node calcifications in a study [7]. Volumetric imaging has been increasingly used as a diagnostic tool. According to the guidelines by the American Academy of Oral and Maxillofacial Radiology, CBCT images constitute a valuable tool for determining the location of HC’s by oral and maxillofacial radiologists. CBCT allows acquisition of high-quality images using lower doses of radiation along with multi-planar reformations rendering precise diagnosis for an effective treatment planning compared to two-dimensional radiography which suffers from overlapping of structures and ghost images [3]. OPG of the present case displayed the superior aspect of mass being attached to the inferior border of the mandibular antegonial notch, which was clearly refuted in the CBCT images, confirming no such association between the mass and hard tissue structures.
Five lymph node calcifications (0.77%) were reported out of 400 CBCT scan data in a study by Barghan S [8]. In another study 37 (15%) out of 246 CBCT scans of mandible had shown evidence of HC’s [3]. The present study was an incidental finding reported in CBCT and OPG. In a recent study by Khojastepour L et al., stated that soft tissue calcifications in mandibular region were relatively common finding especially in posterior region and more likely to be seen in men and in older age group, which is in agreement with the present case report [9]. The greatest inconvenience in assessing CBCT scans is absenteeism of soft tissue landmarks for identifying exact location of the calcifications. CBCT images do not allow to determine whether the calcification is inside a soft tissue lesion, such as a malignant neoplasm, creating a diagnostic dilemma. The present case also suffered because of this deficit in displaying soft tissues.
Present case was initially devoid of medical history and clinical examination, as the case was referred from another dental clinic for radiological consult prior to surgical implant placement, the radiographic diagnosis of the incidental finding vested upon the radiographic appearance and anatomical location of the findings, following which differential diagnosis of submandibular lymph node calcification, submandibular sialolith or phlebolith were suspected. However, sialolith tends to have a uniform smooth outline compared to the irregular outline in the present case and phleboliths are relatively smaller and have bull’s eye or target appearance and their shape resemble straight or slightly curved sausages, thus eliminating submandibular sialolith and phlebolith, leaving us with submandibular lymph node calcification as a final radiographic diagnosis. Later the medical history of the patient was shared, upon intimating the incidental finding encountered in the radiological examination. HC’s occurs in lymph nodes that have been chronically inflamed because of various diseases, frequently granulomatous disorders. Here the lymphoid tissue gets substituted by hydroxyapatite-like calcium salts, nearly effacing all of the nodal structure. The presence of calcifications in lymph nodes entails disease, either active or the result of formerly treated pathosis [1].
CBCT images with low-contrast resolution are not sufficient enough to allow the differentiation among soft tissue structures. Large field of view CBCT scans may demonstrate a relatively high incidence of incidental findings in the head and neck region and outside of the maxillofacial skeleton, which may or may not require referral to specialist or additional diagnostic tests and interventional treatment strategies.
Conclusion
Incidental findings may assist the radiologist to help the referring dentist and patient in identifying the underlying unknown or known conditions of the patient. Knowledge regarding anatomy of the maxillofacial region assists in determining the tissue origin of HC’s visible in CBCT scan. Clinical examination and medical history supports in eliminating unnecessary differential diagnosis thereby enhancing the radiographic diagnosis.
[1]. Carter LC, Soft tissue calcifications and ossification. In: White SC, Pharoach MJ, edsOral Radiology: Principles and Interpretation 2009 6th ednSt LouisMosby Elsevier:526-540. [Google Scholar]
[2]. Freny R Karjodkar, Soft Tissue Calcifications and Ossifications. In: Freny R KarjodkarEssentials of Oral and maxillofacial radiology 2014 1st ednNew DelhiJaypee Brothers Medical Publishers (P) Ltd:503-515.10.5005/jp/books/12300_27 [Google Scholar] [CrossRef]
[3]. Nunes LFS, Santos KCP, Junqueiraa JLC, Oliveira JX, Prevalence of soft tissue calcifications in cone beam computed tomography images of the mandibleRev Odonto Cienc 2011 26(4):297-303.10.1590/S1980-65232011000400004 [Google Scholar] [CrossRef]
[4]. Aydin U, Tuberculous lymph node calcification detected on routine panoramic radiography: a case reportDentomaxillofac Radiol 2003 32:252-54.10.1259/dmfr/5657926013679357 [Google Scholar] [CrossRef] [PubMed]
[5]. Wood NK, Goaz PW, Lehnert JF, Periapical radiopacities. In: Wood NK, Goaz PW (eds)Differential diagnosis of oral and maxillofacial lesions 1997 5th ednSt Louis, MOMosby-Year Book:474 [Google Scholar]
[6]. Almog DM, Tsimidis K, Moss ME, Gottlich RH, Carter LC, Evaluation of a training program for detection of carotid artery calcifications on panoramic radiographsOral Surg Oral Med Oral Pathol Oral Radiol Endod 2000 90:111-17.10.1067/moe.2000.10705610884646 [Google Scholar] [CrossRef] [PubMed]
[7]. Eisenkraft BL, Som PM, The spectrum of benign and malignant etiologies of cervical node calcificationAm J Roentgenol 1999 172:1433-37.10.2214/ajr.172.5.1022753310227533 [Google Scholar] [CrossRef] [PubMed]
[8]. Barghan S, TahmasbiArashlow M, Nair MK, Incidental findings on cone beam computed tomography studies outside of the maxillofacial skeletonInt J Dent 2016 2016:919650310.1155/2016/919650327462350 [Google Scholar] [CrossRef] [PubMed]
[9]. Khojastepour L, Haghnegahdar A, Sayar H, Prevalence of soft tissue calcifications in CBCT images of mandibular regionJ Dent (Shiraz) 2017 18(2):88-94. [Google Scholar]