Retroperitoneal Lipoblastoma-A Rare Entity
Suhitha Gajanthody1, Harshavardhan Gowda2, Ashraf Ahamed3, Anuradha CK Rao4, MR Shashidhar5
1 Assistant Professor, Department of Pediatric Surgery, Yenepoya Medical College Hospital, Mangalore, Karnataka, India.
2 Resident, Department of General Surgery, Yenepoya Medical College Hospital, Mangalore, Karnataka, India.
3 Associate Professor, Department of Pediatric Surgery, Yenepoya Medical College Hospital, Mangalore, Karnataka, India.
4 Professor, Department of Pathology, Yenepoya Medical College Hospital, Mangalore, Karnataka, India.
5 Assistant Professor, Department of Pathology, Yenepoya Medical College Hospital, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Suhitha Gajanthody, Suprasada, 6th Cross, Lohithnagar, Mangalore-575006, Karnataka, India.
E-mail: suhith@rediffmail.com
Lipoblastomas are uncommon tumours which can achieve enormous size and volumes occurring in young paediatric population predominantly. Retroperitoneal locations of these tumours are very rare and only a few cases have been noted in the literature. In spite of their large size and at times infiltrative nature, they can be surgically excised successfully with low complication rates. They usually present due to pressure effect on adjacent structures or due to mass effect with no malignant potential. We describe a case of large retroperitoneal lipoblastoma and review the current literature and management.
Benign, Cytogenetics, Histology, Lipoblasts, Paediatric
Case Report
A one-year-old male child presented with a progressive abdominal distension of 2 months duration and a mass palpated by the child’s mother since 1 month. There was no history of fever, pain, vomiting or abdominal distention. The child weighed 10.5 kg and had normal cry and activity. General physical examination was normal.
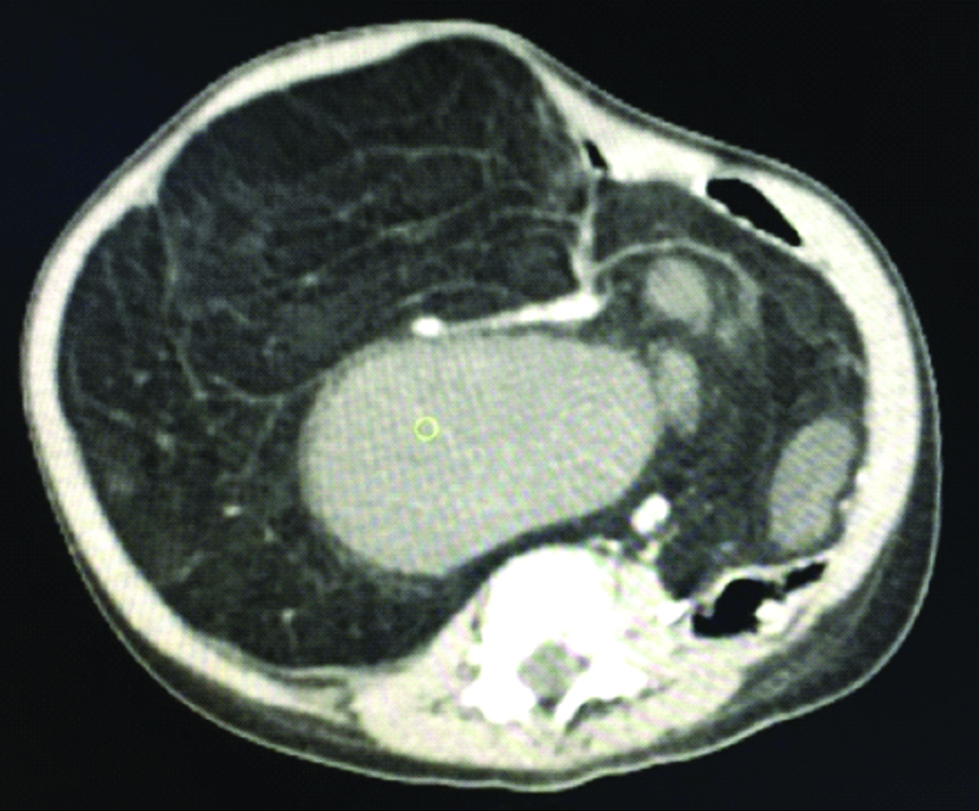
On examination, a non tender, firm, retroperitoneal mass was palpated in the right hypochondrium, umbilical and right lumbar region. The biochemical reports were normal including a normal beta HCG and AFP levels. A provisional diagnosis of a retroperitoneal tumour was made. Ultrasonography of the abdomen showed echogenic lobulated mass lesion occupying the right upper and lower quadrants with right mild hydronephrosis. Contrast Enhanced Computerised Tomography (CECT) of abdomen showed large infra and retroperitoneal fat and fluid density lesion enhancing the great abdominal vessels, displacing the bowel loops, urinary bladder, kidneys and pancreas suggestive of a large retroperitoneal tumour [Table/Fig-1].
CECT abdomen showing large retroperitoneal tumour displacing the bowel and kidneys.
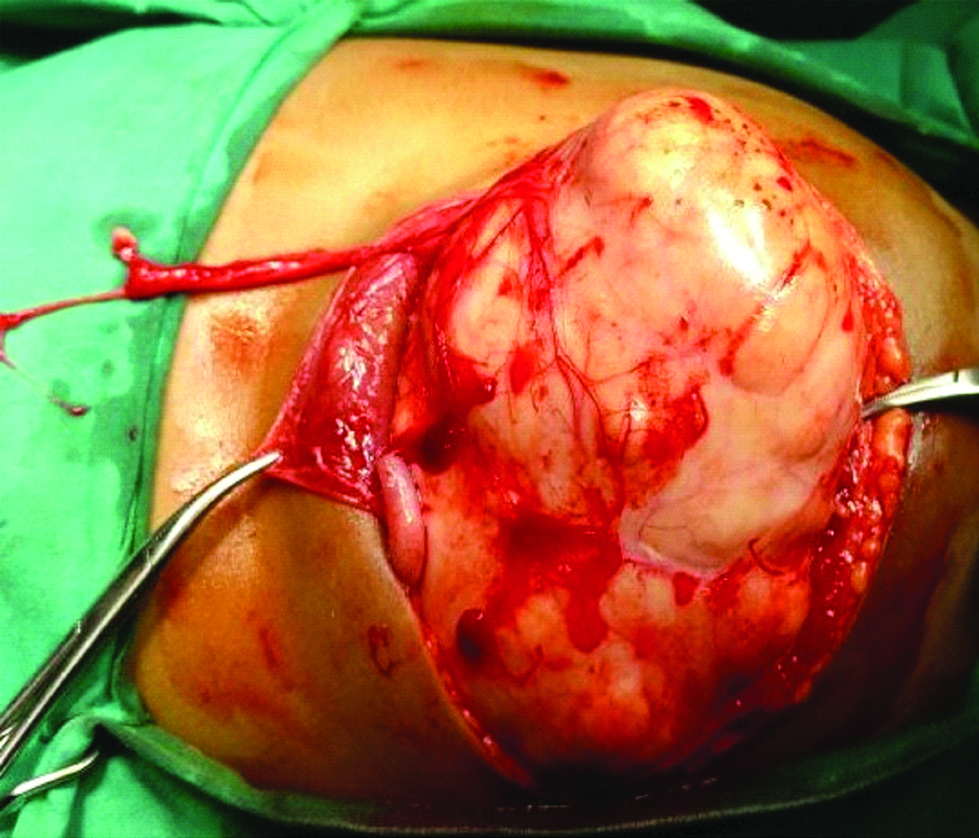
Explorative laparotomy revealed a large retroperitoneal tumour, pressing on the right ureter, displacing the bowel to the left and a thin walled inferior venacava due to pressure effect [Table/Fig-2]. The tumour was completely removed and rest of abdomen explored thoroughly to exclude other abnormalities.
Intraoperatively yellowish white tumour with lobulations.
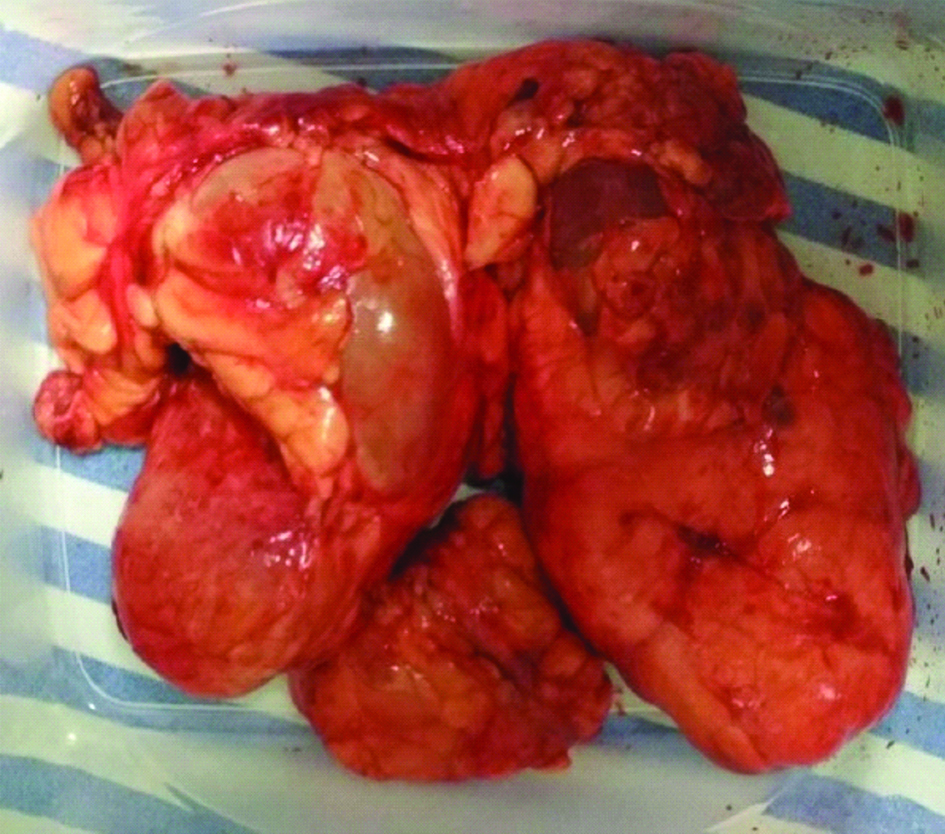
Grossly the tumour was 29.5×19×8.5 cm in dimensions and weighed 814 gm [Table/Fig-3]. Microscopically sections studied showed hypocellular lobules of adipocytes in various stages of differentiation including preadipocytes separated by prominent fibrous septa of varying thickness along with myxoid change. Histopathological features were suggestive of Lipoblastoma with myxoid change [Table/Fig-4,5 and 6].
Excised tumour measuring 29.5×19×8.5 cm.
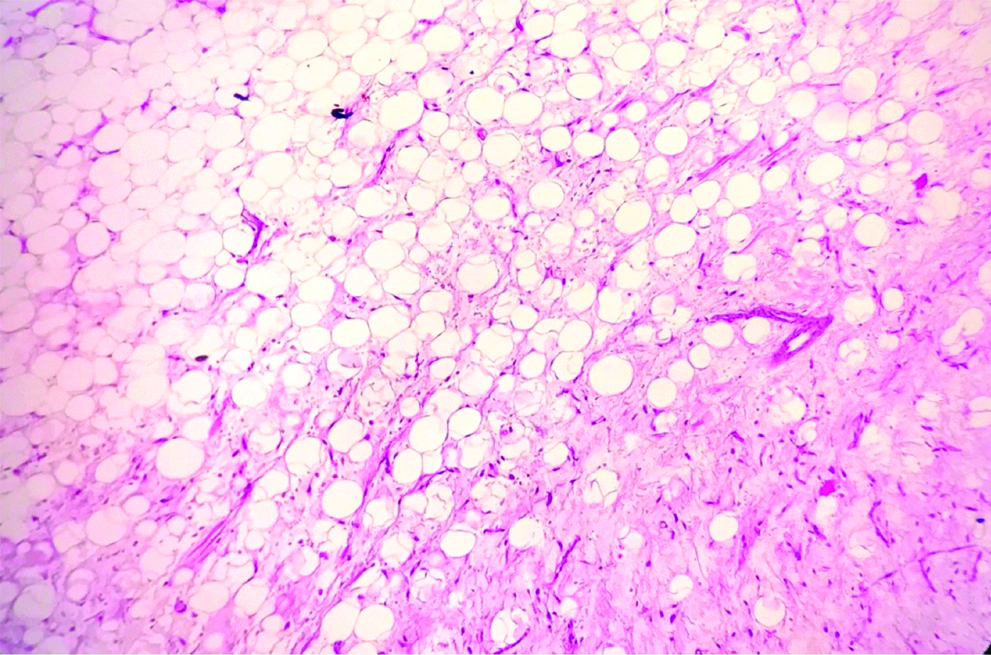
Photomicrograph showing hypocellular adipocytes with extensive plexiform pattern of blood vessels (H&E stain, 10X).
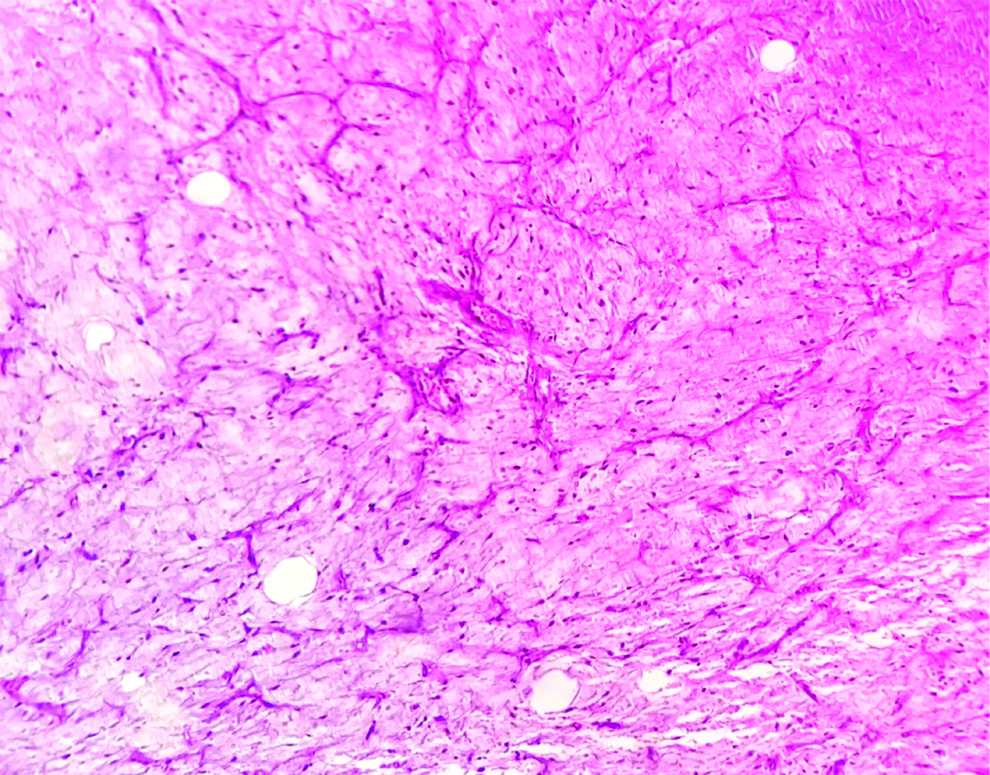
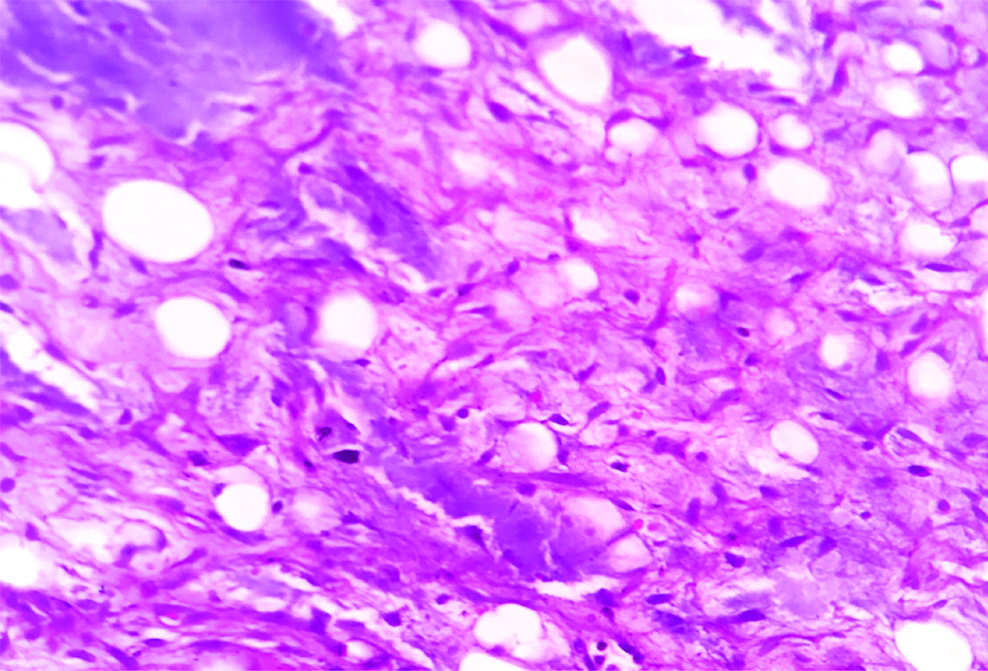
Photomicrograph showing hypocellular lobule of adipocytes in various stages of differentiation including preadipocytes separated by fibrous septa along with myxoid change (H&E stain, 40X).
Photomicrograph showing adipocytes in various stage of differentiation (H&E stain, 10X).
The child had an uneventful postoperative period and was completely asymptomatic at 6 months follow-up.
Discussion
Adipose tissue tumours are quite rare in childhood and comprises of only less than 6% of soft tissue tumours [1]. Chung E et al., described two forms: a localized, superficial, lobulated, encapsulated, or circumscribed form called lipoblastoma and a diffuse, infiltrative form called lipoblastomatosis [2]. Lipoblastomas usually occurs in the subcutaneous plane of extremities, while lipoblastomatosis have a tendency to infiltrate into body compartments (retroperitoneum, abdomen, thorax) [1]. However, rare sites with lipoblastomas have been documented in the literature which includes- mesentric, inguinolabial, perineal and intrascrotal types [3].
The utility of ultrasonography, Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are well documented in the evaluation, but surgical removal of the tumour is mandatory to exclude the possibility of malignancy. In absence of any malignant changes (histologically), additional studies to stage the disease is not required, as lipoblastomas have no known malignant potential [4].
A lipoblastoma can be confused with a myxoid liposarcoma due to the presence of lipoblasts and the plexiform vascular pattern in a myxoid background. In these histologically borderline or difficult cases, cytogenetics can be of diagnostic value [5]. Rearrangements of chromosomal region 8q11-33 are found in the majority of lipoblastomas, whereas a distinctive translocation t(12;16) (q13;p11) is found in myxoid liposarcoma [6-8]. Lipoma, hybernoma, rhabdomyosarcoma and teratomas may be considered as alternative differential diagnosis.
Recommended treatment for lipoblastomas is complete surgical excision considering only one case has been reported with spontaneous resolution [7]. However, if critical structures are involved, a staged approach can be adapted [7]. Recurrence rates of up to 26% have been documented, especially in lipoblastomatosis with a mean follow-up of up to 3 years. Hence, regular follow-up for a period of 5 years is advocated [5,7,9].
Conclusion
Lipoblastoma is a very uncommon diagnosis in the retroperitoneal location. CT or MRI evaluation helps in delineating the tumour, its extent and involvement of other structures. Complete surgical removal is the recommended modality of treatment with a proper advice of rate of recurrence. A minimum follow-up of 5 years is recommended.
[1]. Hicks J, Dilley A, Patel D, Barrish J, Zhu S, Brandt M, Lipoblastoma and lipoblastomatosis in infancy and childhood: histopathologic, ultrastructural, and cytogenetic featuresUltrastructural Pathology 2001 25(4):321-33.10.1080/01913120175313635911577778 [Google Scholar] [CrossRef] [PubMed]
[2]. Chung E, Enzinger F, Benign lipoblastomatosis. An analysis of 35 casesCancer 1973 32(2):482-92.10.1002/1097-0142(197308)32:2>482::AID-CNCR2820320229>3.0.CO;2-E [Google Scholar] [CrossRef]
[3]. Eyssartier E, Villemagne T, Maurin L, Machet M, Lardy H, Intrascrotal lipoblastoma: A report of two cases and a review of the literatureJournal of Pediatric Urology 2013 9(6):e151-54.10.1016/j.jpurol.2013.03.01623664430 [Google Scholar] [CrossRef] [PubMed]
[4]. Moaath A, Raed E, Mohammad R, Mohammad S, Lipoblastoma: a rare mediastinal tumourThe Annals of Thoracic Surgery 2009 88(5):1695-97.10.1016/j.athoracsur.2009.03.03319853146 [Google Scholar] [CrossRef] [PubMed]
[5]. Dilley A, Patel D, Hicks M, Brandt M, Lipoblastoma: Pathophysiology and surgical managementJournal of Pediatric Surgery 2001 36(1):229-31.10.1053/jpsu.2001.2006011150471 [Google Scholar] [CrossRef] [PubMed]
[6]. Kloboves-Prevodnik V, Us-Krašovec M, Gale N, Lamovec J, Cytological features of lipoblastoma: A report of three casesDiagnostic Cytopathology 2005 33(3):195-200.10.1002/dc.2032216078242 [Google Scholar] [CrossRef] [PubMed]
[7]. Speer A, Schofield D, Wang K, Shin C, Stein J, Shaul D, Contemporary management of lipoblastomaJournal of Pediatric Surgery 2008 43(7):1295-300.10.1016/j.jpedsurg.2007.10.06818639685 [Google Scholar] [CrossRef] [PubMed]
[8]. Deen M, Ebrahim S, Schloff D, Mohamed A, A novel PLAG1-RAD51L1 gene fusion resulting from a t(8;14)(q12;q24) in a case of lipoblastomaCancer Genetics 2013 206(6):233-37.10.1016/j.cancergen.2013.05.01923890983 [Google Scholar] [CrossRef] [PubMed]
[9]. Kok K, Telisinghe P, Lipoblastoma: clinical features, treatment, and outcomeWorld Journal of Surgery 2010 34(7):1517-22.10.1007/s00268-010-0466-820151124 [Google Scholar] [CrossRef] [PubMed]