Bilateral Pneumothorax-rare Manifestation of Melioidosis
Allen Aloysius D’Silva1, Jayasenan Jayannan2, Ali Hazan Karnam3, Sanjay R Nair4, Natarajan Vasanthi5
1 Postgraduate Resident, Department of General Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India.
2 Postgraduate Resident, Department of General Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India.
3 Assistant Professor, Department of Emergency Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India.
4 Associate Professor, Department of Cardiothoracic Surgery, Pondicherry Institute of Medical Sciences, Puducherry, India.
5 Associate Professor, Department of General Medicine (Endocrinology), Pondicherry Institute of Medical Sciences, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Natarajan Vasanthi, Associate Professor, Department of General Medicine, Kalapet, Kanagachetikulam, Puducherry-605014, India.
E-mail: vasanthikarthi2004@yahoo.co.in
Melioidosis is caused by gram negative bacilli called Burkholderia pseudomallei. It is an infectious threat to southeast Asian population. It predominantly affects the diabetic people who have got exposure to the contaminated soil. As it affects multiple organs, it mimics other disease like-tuberculosis. Here we report an unusual pulmonary manifestation of Burkholderia infection in a diabetic patient. A 46-year-old male presented with neck swelling and bilateral pulmonary nodules with pneumothorax. His blood culture and pus culture from neck swelling confirmed Burkholderia pseudomallei. He was managed with bilateral intercostal drainage, sensitive antibiotics and showed improvement. Melioidosis causing bilateral pneumothorax with nodules and its complete recovery was not reported earlier.
Intercostal drainage, Pulmonary manifestation, Pulmonary nodule
Case Report
A 46-year-old man with recently detected type 2 diabetes mellitus presented to emergency department with the history of swelling in the anterior aspect of the neck for last 40 days duration. He had fever for last 40 days, which was low grade and intermittent. He was on irregular intake of medication Tab Glimepiride 1 mg once daily and Tab. Metformin 500 mg twice daily. He used to consume alcohol occasionally but never smoked. Also, the patient informed that he used to play football. He had similar swelling 1-year back, for which he was treated at local hospital, of which medication details were not available. Following that his swelling size decreased and remained asymptomatic.
On examination he was conscious, oriented and dyspneic. There was 2×2 cm soft, painless swelling present in the right side of the neck. Vitals-BP-110/70 mmHg, pulse rate-140/min, respiratory rate-45/min, SpO2-95% with 10 L oxygen. On clinical examination, Chest-bilateral normal vesicular breath sounds were heard. Per abdomen-liver was enlarged, 3 cm below costal margin, non-tender. His blood investigation revealed Hb-10g%, total count 6000/c.mm, neutrophils-80%, lymphocytes-14%. Renal function was normal. His liver function showed elevated liver enzymes SGOT-122 U/L, SGPT-106 U/L, total protein-5.2 g/dl, albumin 2.6 g/dl, Alkaline phosphatase-370 u/l. His virology was non-reactive. His serum procalcitonin was very high-100 ng/mL.
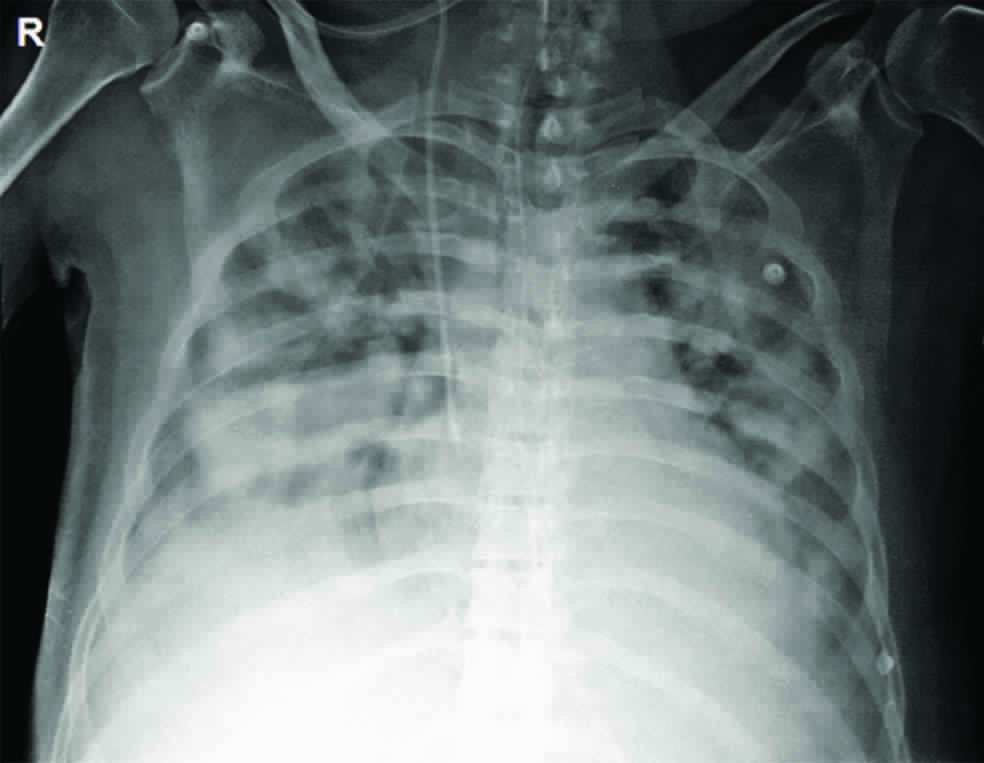
His x-ray chest showed bilateral mid and lower zone infiltrations [Table/Fig-1]. Arterial Blood Gas (ABG) showed hypoxia-P02-40 mmHg. With the history of persistent fever, neck swelling for 40 days duration with bilateral pulmonary infiltration in a diabetic patient-differential diagnosis considered at this stage was disseminated tuberculosis. Ultrasound guided Fine Needle Aspiration Cytology (FNAC) of neck swelling was done, one ml of pus was drained, which was negative for gram stain and AFB. He was started on inj. Imipenem 500 mg IV q 8 hrly. Subsequently his blood culture revealed Burkholderia pseudomallei. His pus culture also grew Burkholderia pseudomallei. Inj Ceftazidime 2 g IV q 8 hrly was added as per culture sensitivity.
X-ray chest showing bilateral lung infiltrations on admission.
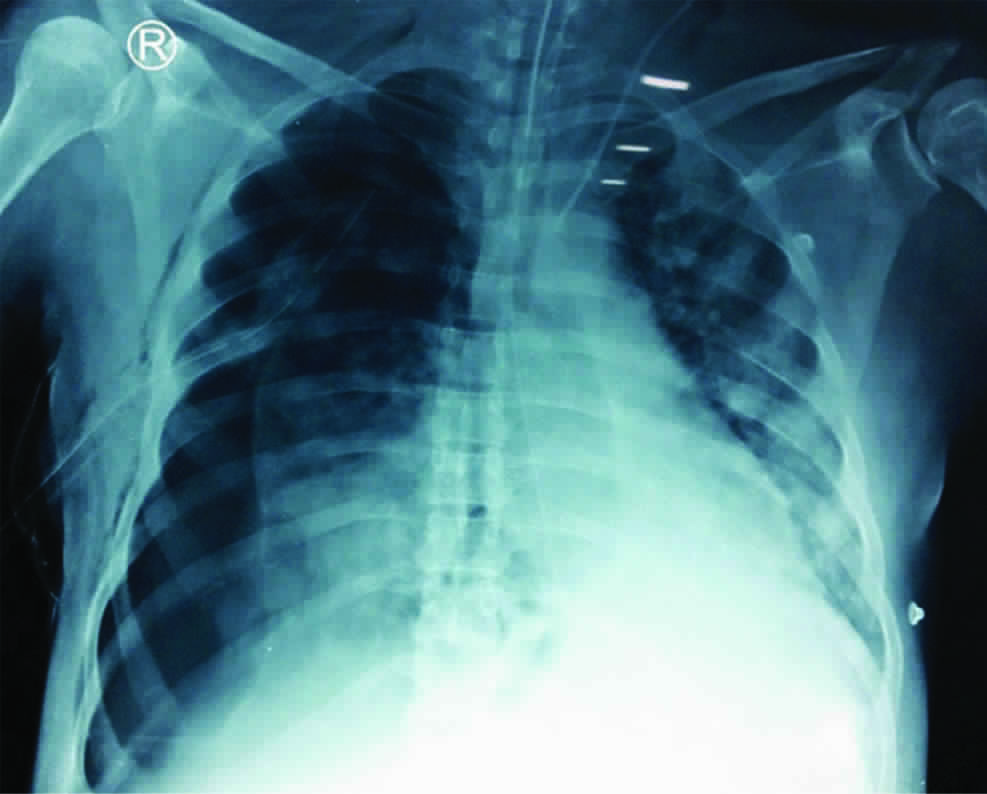
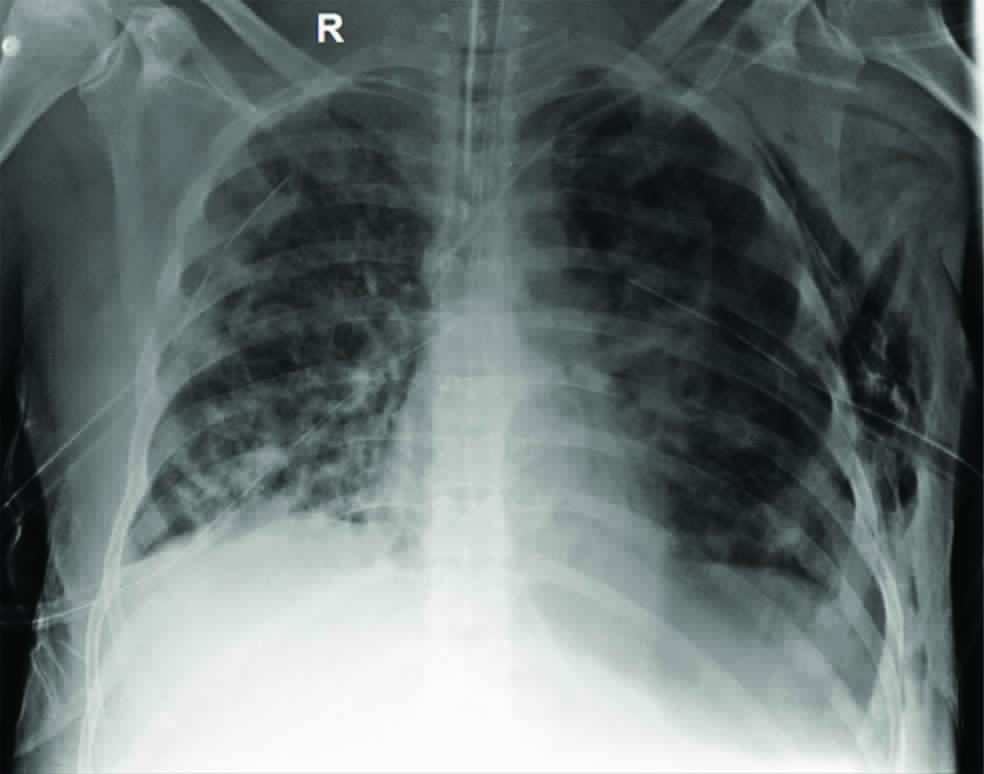
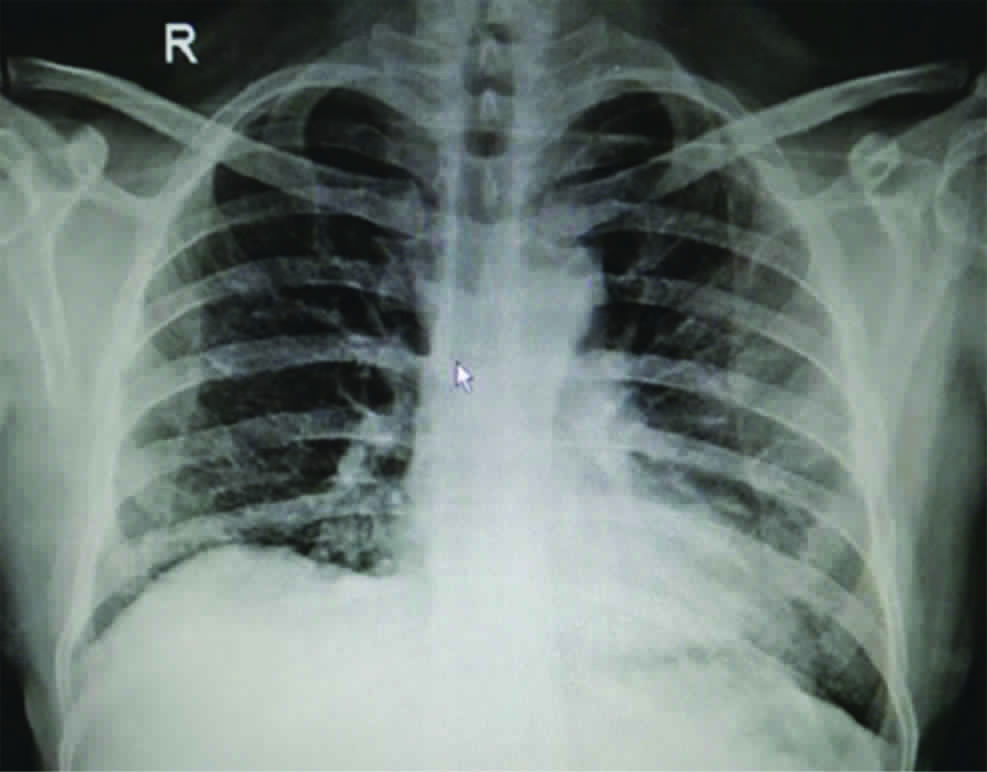
As he was dyspneic and hypoxic, he was intubated and mechanically ventilated. On 4th day he had right sided pneumothorax and Intercostal Drainage (ICD) was placed, chest expanded [Table/Fig-2]. After 24 hours there was right-sided tube block and another ICD was placed. Repeat X-ray chest showed expanded right lung. Next day he had left sided diminished air entry, found to have left sided pneumothorax and ICD was placed [Table/Fig-3]. He was continued on ventilator support with bilateral ICD. Serial arterial blood gas analysis and X-ray were taken. As he was haemodynamically unstable since admission, requiring ventilatory support, inotropes with bilateral ICD, Computed Tomography of chest was not planned at that time. He showed gradual improvement with initiation of sensitive antibiotics. As he had multiple X-ray chest previously, the risk of radiation with further CT chest was considered. As the risk outweigh the benefit, CT chest was not considered. He underwent tracheostomy and gradually weaned from ventilator. In the meantime left ICD followed by right ICD was removed. He was continued on inj. Imipenem and inj. Ceftazidime for 4 week followed by Tab. Trimethoprim/Sulfamethoxazole double strength twice daily was continued for 20 week. On follow up his chest X-ray showed clearing of bilateral lung lesion [Table/Fig-4].
X-ray chest showing right sided pneumothorax with Intercostal drainage insitu.
X-ray chest showing right sided expanded lung with left sided pneumothorax with Intercostal drainage, bilateral pulmonary nodules.
X-ray chest on follow up after completion of antibiotics showing complete resolution of bilateral lung nodules.
Discussion
Melioidosis is caused by a gram negative bacterium called Burkholderia pseudomallei which is a natural habitant of water and soil. It is otherwise called Whitmore disease. The infection mainly spreads by ingestion, inhalation or direct contact with the contaminated water and soil over the abraded skin. This infection predominantly occurs in rainy season. This can infect both humans and animals. People with the immunosuppression such as diabetes mellitus, alcoholism, chronic kidney disease, malignancy are at high risk of getting this infection [1].
It affects multiple organs of the body. Its systemic manifestations are multiple cutaneous, visceral abscess (liver, spleen, prostate, abdominal wall), pneumonia, septic arthritis, osteomyelitis, acute cholangitis [1] and septicaemia [2].
Lung is the most predominantly affected organ. Pulmonary melioidosis manifest as pneumonia, single and multiple cavitation, lung abscess, mass lesion [3], pleural effusion, empyema [4]. Among the pulmonary manifestations acute pneumonia is the commonest presentation with the predominant X-ray features of localized patchy alveolar infiltrations. Pneumothorax as a complication of pulmonary melioidosis occurs in 1.2% of people [5]. Dhiensiri T et al., reported 183 cases with X-ray features of pulmonary melioidosis have revealed that disseminated nodules, alveolar lesion, rapidly progressing and cavitations are more common in acute septicaemic patients. Pleural effusion or empyema was reported in 21% of cases [6]. Cavitatory lung lesion can rupture and present as pneumothorax. Hsu KY has reported a case of melioidosis with single nodule complicated by right sided pneumothorax, had persistence leak with defect which was closed by video assisted thoracoscopic procedure [7]. With the adequate literature search bilateral pneumothorax as a complication of pulmonary melioidosis was not reported earlier. In present case he had bilateral multiple nodules and pneumothorax, with the antibiotic cover, his lung lesions improved gradually and were able to remove the ICD without the need of any thoracoscopic procedure.
In most of the cases its clinical and imaging findings are mimicking either pulmonary or disseminated tuberculosis. In our case fever, neck swelling for 40 days, bilateral pulmonary infiltrates with elevated alkaline phosphatase initially suspected of disseminated tuberculosis. Later on his blood culture confirmed Burkholderia infection. In a state of acute worsening bilateral multiple nodules/abscesses, melioidosis should be differentiated from Staphylococcus aureus infection. In severe septicaemia, even with the confirmed diagnosis and appropriate antibiotics the mortality is high upto 40% [8]. Earlier suspicion of this systemic threat by Burkholderia should be addressed in a patient with risk factor and in an endemic area.
Conclusion
In an immunocompromised septicaemic patient, with persistent fever and bilateral pulmonary nodules, underlying Burkholderia infection should be suspected and confirmed by blood culture. Among the pulmonary manifestation of melioidosis bilateral multiple nodules with pneumothorax is the rarest manifestation. With the earlier identification, initiation of sensitive antibiotics and ICD insertion will improve the clinical outcome.
[1]. Lai CH, Huang CK, Chin C, Chen WF, Yang YT, Chen YL, Acute septicaemic melioidosis presenting with acute cholangitisInfection 2007 35(6):461-64.10.1007/s15010-006-6624-017710373 [Google Scholar] [CrossRef] [PubMed]
[2]. Muttarak M, Peh WC, Euathrongchit J, Lin SE, Tan AG, Lerttumnongtum P, Spectrum of imaging findings in melioidosisBr J Radiol 2009 82(978):514-21.10.1259/bjr/1578523119098086 [Google Scholar] [CrossRef] [PubMed]
[3]. Truong KK, Moghaddam S, Al Saghbini S, Saatian B, Case of a lung mass due to melioidosis in MexicoAm J Case Rep 2015 16:272-75.10.12659/AJCR.89318225943405 [Google Scholar] [CrossRef] [PubMed]
[4]. Burivong W, Wu X, Saenkote W, Stern EJ, Thoracic radiologic manifestations of melioidosisCurr Probl Diagn Radiol 2012 41(6):199-209.10.1067/j.cpradiol.2012.01.00123009770 [Google Scholar] [CrossRef] [PubMed]
[5]. Reechaipichitkul W, Clinical manifestation of pulmonary melioidosis in adultsSoutheast Asian J Trop Med Public Health 2004 35(3):664-69. [Google Scholar]
[6]. Dhiensiri T, Puapairoj S, Susaengrat W, Pulmonary melioidosis: clinical-radiologic correlation in 183 cases in northeastern ThailandRadiology 1988 166(3):711-15.10.1148/radiology.166.3.33407663340766 [Google Scholar] [CrossRef] [PubMed]
[7]. Hsu KY, Chang JM, Pulmonary melioidosis complicated by pneumothoraxAnn Thorac Surg 2013 95(6):15910.1016/j.athoracsur.2012.12.06423706470 [Google Scholar] [CrossRef] [PubMed]
[8]. Lie J, Maxwell S, Keeling-Roberts C, Dev D, A case of pulmonary melioidosisRespiratory Medicine CME 2010 3(2):109-110.10.1016/j.rmedc.2009.04.002 [Google Scholar] [CrossRef]