Analysis of Exhaled Breath Condensate pH in Asthma among Indian Population: A Pilot Study
Manjit Sharad Tendolkar1, Amita Athavale2, Jairaj Nair3, Sneha Tirpude4, Rajwardhan Ghatge5, Rahul Kendre6, Anurag Deshpande7, Aditi Punwani8
1 Medical Officer, Department of Medicine, INHS Asvini, Mumbai, Maharashtra, India.
2 Professor and Head, Department of Pulmonary Medicine, Seth GS Medical College, Mumbai, Maharashtra, India.
3 Associate Professor, Department of Pulmonary Medicine, Sion Hospital, Mumbai, Maharashtra, India.
4 Consultant, Department of Pulmonary Medicine, KRIMS, Nagpur, Maharshtra, India.
5 Consultant, Department of Pulmonary Medicine, Apple Saraswati, Kolhapur, Maharashtra, India.
6 SMO, Department of Pulmonary Medicine, KEM Hospital, Mumbai, Maharashtra, India.
7 SMO, Department of Pulmonary Medicine, GTB Hospital, Mumbai, Maharashtra, India.
8 SMO, Department of Pulmonary Medicine, KEM Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manjit Sharad Tendolkar, B-3/2, SBI Colony, Sector 13, Nerul, Navi Mumbai-400706, Maharshtra, India.
E-mail: tendolkarmanjits@gmail.com
Introduction
Asthma is an inflammatory disorder of lungs and analysis of Exhaled Breath Condensate (EBC) pH may give insights on control of asthma. To the best of our knowledge, this is the first study of EBC pH among Indian population.
Aim
To study EBC pH among asthmatics in Indian population.
Materials and Methods
In this cross-sectional study, EBC pH was compared with the control of asthma as well as severity of obstruction. There were 17 males and 33 females of bronchial asthma without exacerbation in a tertiary care hospital of a metro city. EBC pH was measured without deaeration using the Arterial Blood Gas (ABG) analyser and a pH electrode. Severity of asthma was defined as per Global Initiative of Asthma (GINA) guidelines into mild, moderate and severe based on treatment required to maintain control over asthma.
Results
Mean age of participants was 36 years. Mean EBC pH of the study participants was 7.341. Mean EBC pH in males was 7.391. Mean EBC pH in females was 7.316. Mean EBC pH among well controlled asthmatics was 7.330. Mean EBC pH among partially controlled asthmatics was 7.354. There was no significant correlation between EBC pH in well controlled and partially controlled asthmatics (p=0.71). Among subjects with normal spirometry, mean EBC pH was 7.34. Mean EBC pH among patients with moderate obstruction was 7.30. There was a consistent difference in pH of EBC when measured by a pH electrode as compared to ABG machine. Samples measured by pH electrode were acidic by pH difference of 0.8.
Conclusion
We found no correlation of EBC pH with asthma control. Method used for testing pH of EBC affects the result and has to be considered while interpreting studies.
Bronchial asthma, Breath analysis, Spirometry
Introduction
Bronchial asthma is defined as a heterogeneous disease, usually characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness and cough that vary over time and in intensity, together with variable expiratory airflow limitation [1].
EBC analysis is a method of condensing the exhaled air into liquid by exposing it to a cold surface in an EBC collecting device. This liquid is a matrix of biomarkers like other body fluids [2]. This liquid is then analysed for its individual constituents as per requirement.
EBC pH is a non-invasive, effort independent way of monitoring airway inflammation and simple assay that can be performed repeatedly without adversely affecting a patient, and can be collected safely both orally and from endotracheal and tracheostomy tubes. EBC pH measures remain the most successful manner to date to evaluate the role of airway acidification in respiratory disease [3]. Measurement of pH in EBC is very reproducible, relatively easy to perform, and provides almost real-time results [4].
By assessing the EBC pH and correlating with the control of asthma and severity of obstruction we tried to find out if this method can be used to gauge the control and severity of asthma. Previous studies have reported conflicting results on this subject, and no study has been done in Indian population.
Also, if there is a correlation of EBC pH and control of asthma, it can be used to titrate the use of anti-inflammatory medications. This being a non-effort dependent method, has the potential of contributing to asthma management.
Materials and Methods
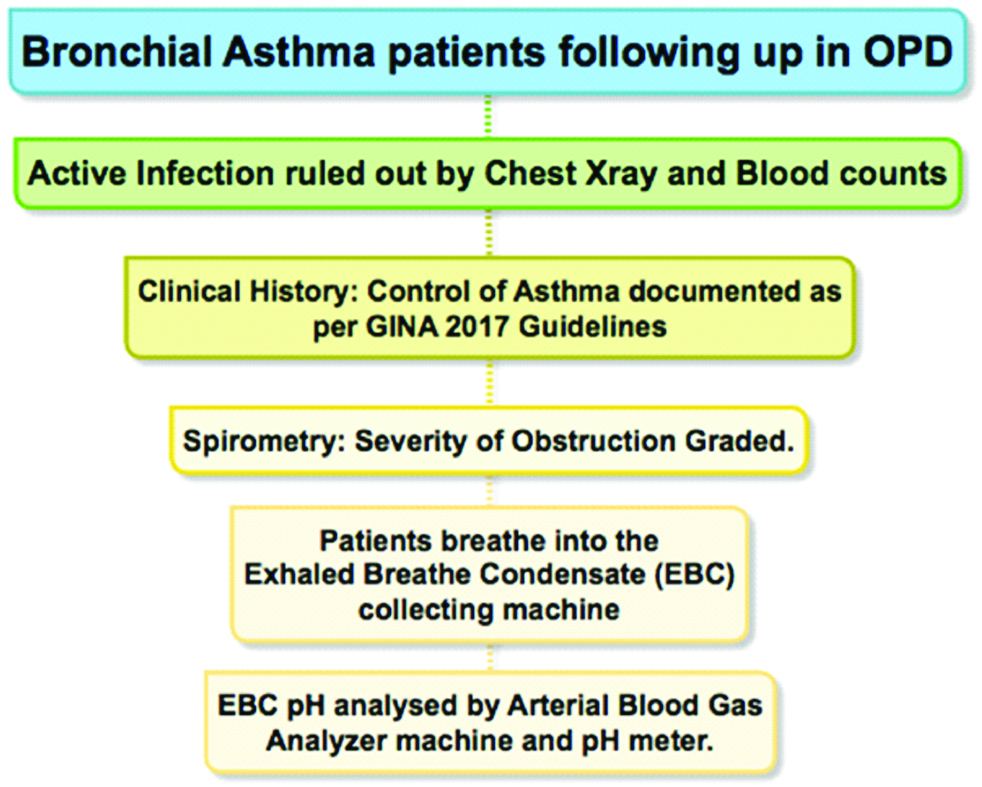
This was a cross-sectional study on 50 bronchial asthma patients following up in OPD of a tertiary care hospital in a metro city of India. This study was conducted from September 2013 to September 2015. An approval by Ethics committee was taken (EC/78/2014). Patient verbal consent was obtained. Sample size was limited to 50 as this was a pilot study. Non-smoking population between 12-70 years of age were included in this study. Active infection was ruled out by blood haemogram and chest radiograph. Asthma control was documented as per GINA 2015 guidelines into well controlled and partially controlled. Uncontrolled asthma was excluded from the study.
After appropriate instructions patients underwent EBC collection using EcoScreen. EBC collection method involved patients rinsing their mouth and breathing at total volume in the mouth piece of EcoScreen for approximately 10 minutes, thus giving us approximately 3 mL of exhaled breath fluid for analysis. This fluid was analysed by ABG analyser machine. Initial 20 samples were simultaneously analysed on ABG analyser machine and pH electrode {ISFET electrode (Sentron, the Netherlands)} [Table/Fig-1]. Samples were analysed within 5 mins of collection. No deaeration was done. After collection of EBC, patients were made to perform spirometry. As per 2015 Global Initiative for Obstructive Lung Diseases guidelines obstruction on spirometry was documented when FEV1/FVC <0.70. Severity of obstruction based on FEV1 (% of predicted) was as follows, Mild 80-100%, Moderate 50-80%, Severe 30-50%, Very Severe <30% (GOLD 2015).
Methodology of the study.
Data so obtained was analysed using one-way ANOVA and regression analysis.
Results
In our study involving 50 bronchial asthma patients, 17 were males and 33 females. A pH values were reported as recorded by ABG analyser. Mean EBC pH of the participants was 7.341.
Mean EBC pH in males and females was 7.391 and 7.316 respectively. There was no significant association between gender and EBC pH (p=0.13).
Age of the study population ranged from 13 to 66 years (mean: 36.52). There was no correlation between age and EBC pH (r=-0.08, p=0.54) [Table/Fig-2].
| Gender | Number | EBC pH Minimum | EBC pH Maximum | EBC pH Mean | Standard Deviation |
|---|
| Males | 17 (34%) | 7.12 | 7.64 | 7.391 | 0.171 |
| Females | 33 (66%) | 7.05 | 7.65 | 7.316 | 0.162 |
Asthma symptoms of 34 were well controlled and 16 patients were partially controlled. Mean EBC pH of the study in asthmatics was 7.341. Mean EBC pH among well controlled asthmatics was 7.330. Mean EBC pH among partially controlled asthmatics was 7.354. There was no significant correlation between EBC pH in well controlled and partially controlled asthmatics (p=0.71) [Table/Fig-3].
Asthma control and EBC pH.
| Asthma Control | Number | EBC pH Minimum | EBC pH Maximum | EBC pH Mean | Standard Deviation |
|---|
| Well Controlled | 34 (68%) | 7.05 | 7.65 | 7.33 | 0.181 |
| Partially Controlled | 16 (32%) | 7.12 | 7.63 | 7.354 | 0.149 |
A total of 37 (74%) patients had normal spirometry, 2 (4%) had mild obstruction, 8 (16%) had moderate obstruction, 2 (4%) had severe obstruction, 1 (2%) had very severe obstruction. Among subjects with normal spirometry, mean EBC pH was 7.34. Mean EBC pH among patients with moderate obstruction was 7.30. There was no significant association between severity of obstruction and EBC pH (p=0.85) [Table/Fig-4].
Severity of airway obstruction and EBC pH.
| Spirometry | Number | EBC pH Minimum | EBC pH Maximum | EBC pH Mean | Standard Deviation |
|---|
| Normal | 37 (74%) | 7.05 | 7.65 | 7.34 | 0.167 |
| Mild Obstruction | 2 (4%) | 7.28 | 7.56 | 7.42 | 0.197 |
| Moderate Obstruction | 8 (16%) | 7.12 | 7.46 | 7.3 | 0.122 |
| Severe Obstruction | 2 (4%) | 7.2 | 7.34 | 7.27 | 0.09 |
| Very Severe Obstruction | 1 (2%) | NA | NA | 7.33 | NA |
There was a consistent difference in pH of EBC when measured by a pH electrode as compared to ABG machine. Samples measured by pH electrode were acidic by pH difference of 0.8.
Discussion
Objective assessment of asthma control has a significance is modulating treatment. We rely on patients subjective reporting of complains and modify treatment accordingly. Often this leads to improper stepping up or stepping down of treatment. Hence there is a need of an objective parameter to gauge asthma control.
Exhaled nitric oxide (FeNO) is being often used for assessing asthma control and has been found to be significantly correlating to asthma control [5]. However, due to significant limitations of various studies assessing role of FeNO in asthma including small number of subjects and short-term follow up, routine assessment of FeNO in assessment of asthma has not been recommended [6].
EBC condensate level of leukotriene E4 is increased in asthma but is not detectable in normal subjects or in patients with Chronic Obstructive Pulmonary Disease (COPD) [7]. EBC level of hydrogen peroxide has also been shown to be a promising biomarker for assessment of asthma [8].
However, the above-mentioned assays for EBC analysis are expensive and in a resource limited setting like India, an economical assessment of asthma control is desired.
The inflammatory markers including Nitric Oxide, leukotriene E4 and hydrogen peroxide result in acidification of exhaled air. Studies in asthma have pointed to the role of airway acidification in the airway pathophysiology [9]. Acidity (pH) is the most easily measured and widely studied biomarker in EBC [10].
EBC can be collected by two of the commercially available devices, namely, portable RTube and non-portable EcoScreen. There is a poor correlation between EBC pH obtained by RTube and EcoScreen [11-13].
Normal values of gas-standardized (“CO2-free”) EBC pH have been reported from multiple investigators and range between 7.5 and 8.1 [14-25]. The difference between pH values of deaerated and non-deaerated samples collected by EcoScreen, on immediate analysis has been studied in 23 subjects (including 10 asthmatics). Mean pH has been reported as 6.99 (6.85–7.13) and 8.17 (8.08–8.26) respectively [12]. In comparison to the above studies the Mean EBC pH in our study was 7.341 (7.05–7.65, SD: 0.167).
Deaeration is a process of removing CO2 from the EBC sample by bubbling Argon gas through the sample. Deaerated sample is known to have stable pH and a reproducible pH value after a year. The act of deaeration makes the sample less acidic by removing CO2 [4]. All the samples we studied were non-deaerated and analysed immediately after collection and thus were comparable.
There have been conflicting results on association between airway obstruction and EBC pH [26,27]. Our study has shown no significant correlation with severity of airway obstruction and EBC pH.
Our study documented no correlation of EBC pH with age and sex is consistent with other studies done in healthy population [16].
In previous study done by Kostikas K et al., it was concluded that EBC pH may identify patients with not well controlled asthma, however its utility may be limited to certain selected subgroups [28]. Ratnawati et al., have studied EBC pH in paediatric population with asthma, atopy and normal children and have concluded that there was no difference in EBC pH between these 3 groups however asthmatics with FEV1 <80% predicted had significantly lower pH [29]. We compared well controlled and poorly controlled asthma and have not found any significant correlation. It is worth a mention that we have not studied EBC pH in uncontrolled asthma.
We were not able to explain the differences in pH measurements between ABG analyser machine and pH electrode. But on a similar context with pleural fluid analysis this was consistent with the recommendation of using blood gas analyser for assessing pleural fluid pH over use of pH electrode [30,31].
Conclusion
We found no correlation of EBC pH with age, sex, severity of obstruction and control of asthma among patients with well controlled and partially controlled asthmatics. Method used for testing pH of EBC affects the result and has to be considered while interpreting studies. Further studies will be needed in normal Indian subjects and those with uncontrolled asthma to know efficacy of EBC pH in documenting objective control of asthma.
[1]. 2015 GINA Report: Global Strategy for Asthma Management and Prevention. 2015;1-159 [Google Scholar]
[2]. Hunt J, Exhaled breath condensate: an overviewImmunology and Allergy Clinics of North America 2007 27(4):587-96.10.1016/j.iac.2007.09.00117996577 [Google Scholar] [CrossRef] [PubMed]
[3]. Hunt J, Exhaled Breath Condensate pH AssaysImmunology and Allergy Clinics of North America 2007 27(4):597-606.10.1016/j.iac.2007.09.00617996578 [Google Scholar] [CrossRef] [PubMed]
[4]. Vaughan J, Ngamtrakulpanit L, Pajewski TN, Turner R, Nguyen T-A, Smith A, Exhaled breath condensate pH is a robust and reproducible assay of airway acidityEuropean Respiratory Society 2003 22(6):889-94.10.1183/09031936.03.0003880314680074 [Google Scholar] [CrossRef] [PubMed]
[5]. Michils A, Baldassarre S, Van Muylem A, Exhaled nitric oxide and asthma control: a longitudinal study in unselected patientsEur Respir J 2008 31(3):539-46.10.1183/09031936.0002040718057062 [Google Scholar] [CrossRef] [PubMed]
[6]. Pendharkar S, Mehta S, The clinical significance of exhaled nitric oxide in asthmaCanadian Respiratory Journal: Journal of the Canadian Thoracic Society. Pulsus Group Inc 2008 15(2):99-106.10.1155/2008/46376218354750 [Google Scholar] [CrossRef] [PubMed]
[7]. Montuschi P, Barnes PJ, Exhaled leukotrienes and prostaglandins in asthmaJournal of Allergy and Clinical Immunology 2002 109(4):615-20.10.1067/mai.2002.12246111941309 [Google Scholar] [CrossRef] [PubMed]
[8]. Teng Y, Sun P, Zhang J, Yu R, Bai J, Yao X, Hydrogen peroxide in exhaled breath condensate in patients with asthma: a promising biomarker?Chest 2011 140(1):108-16.10.1378/chest.10-281621436249 [Google Scholar] [CrossRef] [PubMed]
[9]. Chhabra SK, Gupta M, Exhaled breath condensate analysis in chronic obstructive pulmonary diseaseJ Chest Dis Allied Sci 2012 54(1):27-37. [Google Scholar]
[10]. Carpagnano GE, Barnes PJ, Francis J, Wilson N, Bush A, Kharitonov SA, Breath Condensate pH in Children With Cystic Fibrosis and AsthmaChest. Elsevier 2004 125(6):2005-10.10.1378/chest.125.6.200515189915 [Google Scholar] [CrossRef] [PubMed]
[11]. Leung TF, Li CY, Yung E, Liu EKH, Lam CWK, Wong GWK, Clinical and technical factors affecting pH and other biomarkers in exhaled breath condensatePediatr Pulmonol. Wiley Subscription Services, Inc., A Wiley Company 2006 41(1):87-94.10.1002/ppul.2029616292777 [Google Scholar] [CrossRef] [PubMed]
[12]. Prieto L, Ferrer A, Palop J, Domenech J, Llusar R, Rojas R, Differences in exhaled breath condensate pH measurements between samples obtained with two commercial devicesRespiratory Medicine 2007 101(8):1715-20.10.1016/j.rmed.2007.02.02317481878 [Google Scholar] [CrossRef] [PubMed]
[13]. Czebe K, Barta I, Antus B, Valyon M, Horváth I, Kullmann T, Influence of condensing equipment and temperature on exhaled breath condensate pH, total protein and leukotriene concentrationsRespiratory Medicine 2008 102(5):720-25.10.1016/j.rmed.2007.12.01318249106 [Google Scholar] [CrossRef] [PubMed]
[14]. Gessner C, Hammerschmidt S, Kuhn H, Seyfarth H-J, Sack U, Engelmann L, Exhaled breath condensate acidification in acute lung injuryRespiratory Medicine 2003 97(11):1188-94.10.1016/S0954-6111(03)00225-7 [Google Scholar] [CrossRef]
[15]. Hunt JF, Fang K, Malik R, Snyder A, Malhotra N, Platts-Mills TA, Endogenous airway acidification. Implications for asthma pathophysiologyAm J RespirCrit Care Med 2000 161(3 Pt 1):694-99.10.1164/ajrccm.161.3.991100510712309 [Google Scholar] [CrossRef] [PubMed]
[16]. Paget-Brown AO, Ngamtrakulpanit L, Smith A, Bunyan D, Hom S, Nguyen A, Normative data for pH of exhaled breath condensateChest 2006 129(2):426-30.10.1378/chest.129.2.42616478862 [Google Scholar] [CrossRef] [PubMed]
[17]. Hunt J, Yu Y, Burns J, Gaston B, Ngamtrakulpanit L, Bunyan D, Identification of acid reflux cough using serial assays of exhaled breath condensate pHCough 2006 2:310.1186/1745-9974-2-316608520 [Google Scholar] [CrossRef] [PubMed]
[18]. Borrill ZL, Smith JA, Naylor J, Woodcock AA, Singh D, The effect of gas standardisation on exhaled breath condensate pHEur Respir J 2006 28(1):251-52.authorreply 252-5310.1183/09031936.06.0002670616816353 [Google Scholar] [CrossRef] [PubMed]
[19]. Brunetti L, Francavilla R, Tesse R, Strippoli A, Polimeno L, Loforese A, Exhaled breath condensate pH measurement in children with asthma, allergic rhinitis and atopic dermatitisPediatr Allergy Immunol 2006 17(6):422-27.10.1111/j.1399-3038.2006.00426.x16925687 [Google Scholar] [CrossRef] [PubMed]
[20]. Efstathia M. Konstantinidi, Andreas S. Lappas, Anna S. Tzortzi, Panagiotis K. Behrakis, Exhaled breath condensate: technical and diagnostic aspectsScientific World Journal 2015 2015:43516010.1155/2015/43516026106641 [Google Scholar] [CrossRef] [PubMed]
[21]. Carraro S, Folesani G, Corradi M, Zanconato S, Gaston B, Baraldi E, Acid-base equilibrium in exhaled breath condensate of allergic asthmatic childrenAllergy 2005 60(4):476-81.10.1111/j.1398-9995.2005.00718.x15727579 [Google Scholar] [CrossRef] [PubMed]
[22]. Kostikas K, Papatheodorou G, Ganas K, Psathakis K, Panagou P, Loukides S, pH in Expired Breath Condensate of Patients with Inflammatory Airway DiseasesAm J Respir Crit Care Med 2002 165(10):1364-70.10.1164/rccm.200111-068OC12016097 [Google Scholar] [CrossRef] [PubMed]
[23]. Nicolaou NC, Lowe LA, Murray CS, Woodcock A, Simpson A, Custovic A, Exhaled breath condensate pH and childhood asthma: unselected birth cohort studyAm J Respir Crit Care Med 2006 174(3):254-59.10.1164/rccm.200601-140OC16675782 [Google Scholar] [CrossRef] [PubMed]
[24]. Niimi A, Nguyen LT, Usmani O, Mann B, Chung KF, Reduced pH and chloride levels in exhaled breath condensate of patients with chronic coughThorax 2004 59(7):608-12.10.1136/thx.2003.01290615223872 [Google Scholar] [CrossRef] [PubMed]
[25]. Rosias PPR, Dompeling E, Dentener MA, Pennings HJ, Hendriks HJE, Van Iersel MPA, Childhood asthma: exhaled markers of airway inflammation, asthma control score, and lung function testsPediatr Pulmonol 2004 38(2):107-14.10.1002/ppul.2005615211692 [Google Scholar] [CrossRef] [PubMed]
[26]. Antus B, Barta I, Kullmann T, Lazar Z, Valyon M, Horváth I, Assessment of exhaled breath condensate pH in exacerbations of asthma and chronic obstructive pulmonary diseaseAm J Respir Crit Care Med 2010 182(12):1492-97.10.1164/rccm.201003-0451OC20656939 [Google Scholar] [CrossRef] [PubMed]
[27]. Elhefny A, Mourad S, Morsi TS, Kamel MA, Mahmoud HM, Exhaled breath condensate nitric oxide end products and pH in controlled asthmaEgyptian Journal of Chest Diseases and TuberculosisThe Egyptian Society of Chest Diseases and Tuberculosis 2012 61(4):247-56.10.1016/j.ejcdt.2012.08.007 [Google Scholar] [CrossRef]
[28]. Kostikas K, Papaioannou AI, Tanou K, Giouleka P, Koutsokera A, Minas M, Exhaled NO and exhaled breath condensate pH in the evaluation of asthma controlRespiratory Medicine 2011 105(4):526-32.10.1016/j.rmed.2010.10.01521051211 [Google Scholar] [CrossRef] [PubMed]
[29]. Ratnawati Morton J, Henry RL, Thomas PS, Exhaled breath condensate nitrite/nitrate and pH in relation to pediatric asthma control and exhaled nitric oxidePediatr Pulmonol 2006 41(10):929-36.10.1002/ppul.2046916871619 [Google Scholar] [CrossRef] [PubMed]
[30]. Na MJ, Diagnostic tools of pleural effusion. Tuberculosis and respiratory diseasesThe Korean Academy of Tuberculosis and Respiratory Diseases 2014 76(5):199-210.10.4046/trd.2014.76.5.19924920946 [Google Scholar] [CrossRef] [PubMed]
[31]. Light RW, Pleural Diseases 2013 Lippincott Williams & Wilkins:101 [Google Scholar]