The provision of analgesia, sedation and relief of anxiety are major therapeutic goals in the conduct of endoscopic procedures involving the gastrointestinal tract.
In recent times, propofol has acquired the position of being the cornerstone of outpatient anaesthetic practice. The respiratory and cardiovascular depression that comes along with it also makes it a relatively unsafe agent in untrained hands.
Ketamine has been tried out as the sole agent or adjuvant in adult as well as pediatric practice. There is much more literature alluding to its use in children compared to adults. Gilger MA et al., retrospectively studied 402 procedures in which various combinations of midazolam, pethidine and ketamine were used [1]. Complications like hypoxia, agitation, emergence reactions, stridor, laryngospasm were evaluated. It was found that midazolam meperidine has the highest rate of complications while midazolam-ketamine has lowest rate of complications and highest rate of sedation. They found that the midazolam-ketamine combination had the lowest rate of complications and a rate of adequate sedation equivalent to that of the other combinations. Colonoscopies are generally done on an outpatient basis at our hospital.
The aim of this study was to use a lower dose of ketamine co-administered with midazolam and propofol in colonoscopy, to determine the level of sedation based on Ramsay Sedation Score and analgesia based on Visual Analog Scale (VAS) score and to study the speed of recovery and haemodynamic stability. The overall patient and endoscopist’s satisfaction were also recorded.
Materials and Methods
This was a prospective randomised controlled study done for a period of 2 years (July 2014-June 2016). Written informed consent was taken from the patients after explaining the procedure in detail and ethics committee approval was obtained.
Sixty ASA I-II patients-18 years of age or older who presented as outpatients to the gastroenterology services of our hospital for elective colonoscopy under general anaesthesia were included. The patients with a history of known allergy to propofol, or to soya bean or eggs, with chronic opioid or benzodiazepine use, uncontrolled diabetes or hypertension, intellectual disability that precluded meaningful communication required for conduct of the trial, and presence of any other significant co-morbidity that, in the assessment of the anaesthetist would have compromised the safe administration of an elective general anaesthetic were excluded from the study.
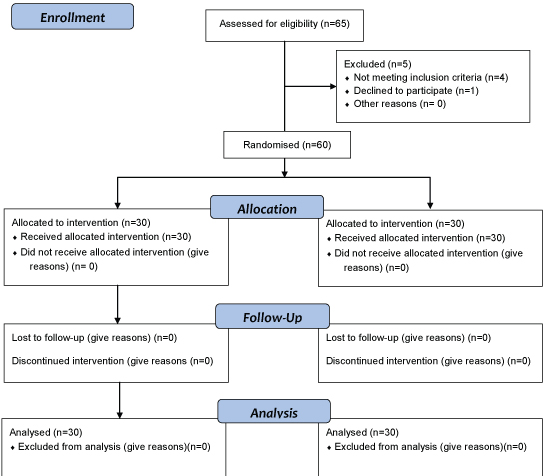
A pre-anaesthetic evaluation was carried out with special reference to airway and patients were categorised according to the ASA classification. The body weight was recorded. All patients were anaesthetised by the same anaesthesiologist. Eligible patients were randomised by sealed envelope technique into two groups. The concealment was obtained by computer generated group selection. Group I (n=30) (Fentanyl group) was assigned to receive midazolam 20 μg/kg, propofol and fentanyl 2 μg/kg. Group II (n=30) (Ketamine group) was assigned to receive midazolam 20 μg/kg, propofol and ketamine 0.5mg/kg [Table/Fig-1].
Consort 2010 flow diagram
The primary outcomes measured include heart rate, blood pressure, SpO2, ETCO2, Ramsay Sedation Score and recovery time; the secondary outcomes measured included endoscopist and patient satisfaction and adverse events.
Procedure
Patients were shifted onto the procedure room, monitoring was established with ECG, pulse oximetry and non-invasive blood pressure. Intravenous access was obtained with a 20 G cannula and a normal saline infusion was commenced. Supplemental oxygen was administered through nasal prongs (3 L/minute) or a Hudson mask (6 L/min). In the fentanyl group, midazolam was administered intravenously in a dose of 20 μg/kg, followed by fentanyl 2 μg/kg. This was followed by a bolus dose of 20-30 mg of propofol and subsequently, increments of 20-30 mg till a Ramsay Sedation Score [2] of 5 was achieved. In the ketamine group, following a 20 μg/kg bolus dose of midazolam, ketamine was administered intravenously at a dose of 0.5 mg/kg. This was again, followed-up with incremental boluses of 20-30 mg of propofol to target a Ramsay Sedation Score of 5. Once a score of 5 was achieved on the Ramsay Sedation Scale, the colonoscope was introduced. Any patient movement or obvious sign of discomfort was noted and additional boluses of 20 mg propofol were administered as required during the procedure. At the end of the procedure, patients were transferred to the recovery room where they were monitored by post-anaesthesia care nursing staff. Recovery from the anaesthetic was assessed using the Modified Aldrete Scoring System. [3] A score of 9 or more was required to confirm full recovery from the anaesthetic.
After full recovery from anaesthesia, a member of the anaesthetic team not involved with the procedure interviewed patients regarding their experience. Patients were asked to indicate their level of satisfaction specifically related to recall of any pain or discomfort at the time of introduction of the colonoscope or at any other time during the procedure on a 10 point Visual Analogue Scale (VAS). A score of 0 represented a totally unpleasant experience while a maximal score of 10 represented complete satisfaction. Patients were also asked to rate the level of nausea they may have felt on a 10 point VAS. A score of 0 represented no nausea and 10 represented the worst imaginable nausea. In the ketamine group, patients were questioned specifically regarding any dreams or hallucinations they may have experienced at any time during or after the procedure. Any emergence behavior was also noted. The endoscopist who conducted the procedure was also asked to grade the level of satisfaction with the adequacy of sedation during the procedure on a 0-10 scoring system, with a maximum score of 10 representing ideal conditions.
Data collected included age and sex of the patient, body weight, ASA physical status. The initial and total dose of propofol used was recorded. Heart rate, blood pressure and oxygen saturation were recorded at every 5 minutes intervals for 60 minutes. Hypotension was defined as a systolic blood pressure of 90 mm/Hg or less.
Time Intervals were defined as below:
Time taken to full sedation: Induction to Ramsay Sedation Score of 5;
Procedure time: Colonoscope in to colonscope out;
Recovery time: Colonoscope out to Modified Aldrete Score of 9.
Any adverse event that occurred during the entire procedure and recovery was recorded. We defined hypotension as a drop in systolic blood pressure to 90 mm Hg or less and a heart rate less than 50 was recorded as bradycardia.
Statistical Analysis
All continuous variables were compared using un-paired t tests; categorical variables were analysed using the chi-square test or the Fisher’s-exact test. Non-parametric, categorical variables were analysed using the Mann Whitney U test. A p-value of 0.05 or less was considered statistically significant. All statistical analysis was carried out using Medcalc Statistical Software version 11.0 (Medcalc Software bvba, Belgium).
Results
Total 60 patients were enrolled, who underwent outpatient colonoscopy under sedation in this study. The groups were matched at baseline in regard to age, sex, body weight and the ASA physical status. The mean age of patients in the fentanyl group was 44.8±9.1 years and that in the ketamine group was 42.1±10.3 years (p = 0.29). The mean body weight in the fentanyl group was 62±12 kg compared to 61.5±13.7 kg in the ketamine group (p=0.89). The male to female ratio and the ASA physical status of patients in both the groups were also comparable [Table/Fig-2].
| Parameters | Fentanyl | Ketamine | p-value |
|---|
| Age (years) | 44.8±9.1 | 42.1±10.3 | p=0.29 |
| Male (n) | 15 | 14 | |
| Female (n) | 15 | 16 | |
| Weight (kg) | 62±12 | 61.5±13.7 | p=0.89 |
| ASA-I (n) | 14 | 16 | |
| ASA-II (n) | 16 | 14 | |
*Highly significant (p≤0.001), **Significant (p≤0.05), ***Not significant (p>0.05)
Parameters measured
Time To Full Sedation: The time to full sedation in the ketamine group was significantly less than that in the fentanyl group (18.3±2.7 seconds Vs 22.4±2.2 seconds; p < 0.001) [Table/Fig-3].
| Variables | Fentanyl | Ketamine | p-value |
|---|
| Time to full sedation (seconds) | 18.3±2.7 | 22.4±2.2 | *p <0.0001 |
| Initial propofol dose (mg) | 37.3±11.7 | 53±13.4 | *p <0.0001 |
| Total dose of propfol (mg) | 87.3±18.7 | 112.3±24.5 | *p <0.0001 |
| Procedure time (min) | 20.5±2.8 | 21.5±2.7 | ***p =0.17 |
| Recovery time (min) | 5.8±1.4 | 8.0±1.9 | *p<0.0001 |
*Highly significant (p≤0.001), **Significant (p≤0.05), ***Not significant (p>0.05)
Initial dose of propofol: The end point of sedation was a Ramsay Sedation Score of 6. The mean initial dose of propofol in the ketamine group was 37.3±11.7 mg compared to 53±13.4 mg in the fentanyl group (p < 0.0001) The initial dose of propofol was significantly less in the ketamine group [Table/Fig-3].
Total dose of propofol: The ketamine group had significantly less propofol requirement for the entire procedure . (87.3±18.7 mg Vs 112.3±24.5 mg p < 0.0001 [Table/Fig-3].
Recovery time: Patients belonging to the ketamine group had a significantly shorter recovery time compared to those in the fentanyl group (5.8±1.4 Vs 8.0±1.9 minutes; p < 0.0001) [Table/Fig-3].
Procedure Time: We also looked at the total time taken to complete the procedure and compared it between groups. The total duration of procedure was taken as the time interval between the induction to withdrawal of the colonoscope. Procedure time was comparable between the groups – 20.5±2.8 minutes in the ketamine group and 21.5±2.7 minutes in the fentanyl group (p= 0.17) [Table/Fig-3].
Incidence of Hypotension: Thirteen patients developed hypotension in the fentanyl group. There was only one instance of hypotension in the ketamine group (p <0.0004) [Table/Fig-4].
Mean systolic blood pressure.
| Time (min) | Number | #SBP(mm of Hg)Fentanyl group | #SBP(mm of Hg)Ketamine Group | p-value |
|---|
| 0 | 30 | 140 | 140 | **p≤0.05 |
| 5 | 30 | 120 | 100 |
| 10 | 30 | 115 | 96 |
| 15 | 30 | 110 | 98 |
| 20 | 30 | 110 | 98 |
*Highly significant (p≤0.001), **Significant (p≤0.05), ***Not significant (p>0.05)
#SBP- Systolic Blood Pressure
Heart Rate: The mean heart rate during the entire procedure was calculated for all patients. The mean heart rate in the ketamine group was 73.6±7.2 beats per min and 67.1±7.4 beats per min in the fentanyl group. The mean heart rate in the ketamine group was significantly faster compared to the fentanyl group (p < 0.001) [Table/Fig-5].
| Time | Number | Fentanyl Group(Beats per minute) | Ketamine Group(Beats per minute) | p-value |
|---|
| Baseline0 minutes | 30 | 73 | 72 | *p≤0.001 |
| 5 min | 30 | 74 | 67 |
| 10 | 30 | 73 | 64 |
| 15 | 30 | 72 | 65 |
| 20 | 30 | 76 | 66 |
| Mean±SD | | 73.6±7.2 | 67.1±7.4 |
*Highly significant (p≤0.001), **Significant (P≤0.05), ***Not significant (p>0.05)
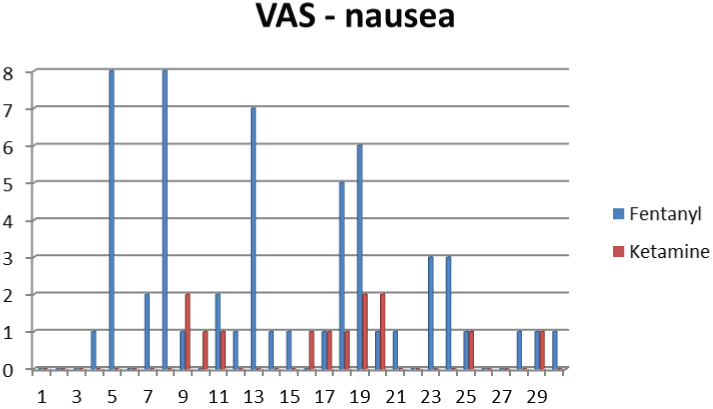
VAS-Nausea: According to VAS scale, patients in the fentanyl group had significantly more subjective feeling of nausea compared to the ketamine group (p=0.0052). The VAS scores for nausea in both the groups is depicted in graphic form below [Table/Fig-6].
Visual Analogue score-Nausea.
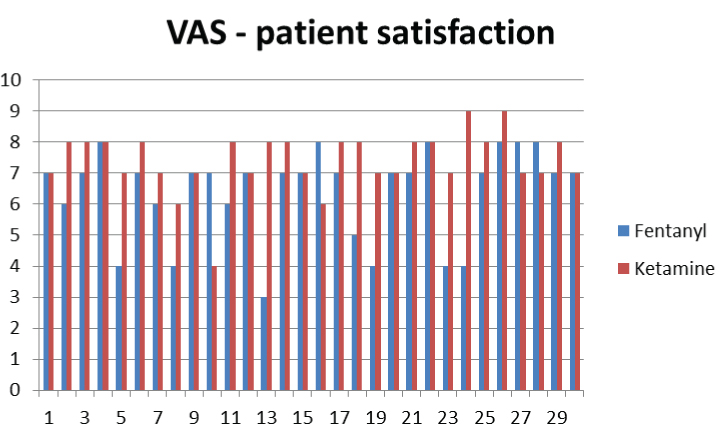
VAS-Patient Satisfaction: Overall satisfaction was significantly higher with the use of ketamine (p=0.006). The graph below shows VAS scores for patient satisfaction in all patients [Table/Fig-7].
Visual analogue score-Patient satisfaction.
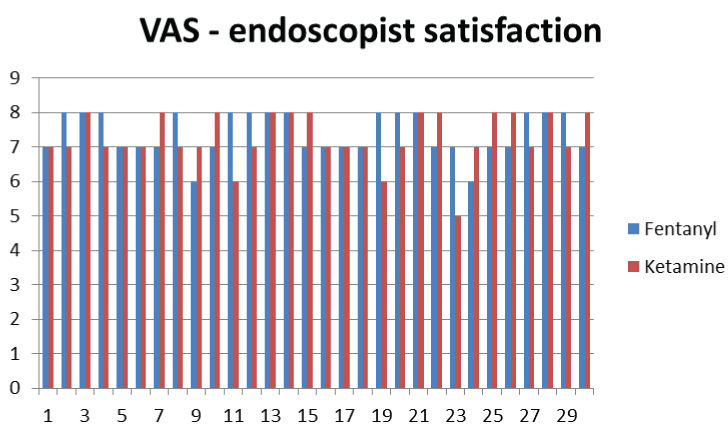
VAS Endoscopist’s Satisfaction: There was no significant difference in the level of satisfaction between the two groups as indicated by the endoscopists who performed the procedures. Endoscopist’s satisfaction on the VAS in shown below in graphic form [Table/Fig-8].
Visual Analogue Score-Endoscopist’s Satisfaction.
Emergence Phenomena: There was no incidence of unpleasant dreams or hallucinations or any other kind of emergence phenomena noted in our patients who underwent this study.
Discussion
Most patients prefer to be asleep during colonoscopy [4]. The use of optimal sedation and analgesia may decisively influence the performance and the quality of colonoscopy [5]. Pain is a major factor that results in dissatisfaction with colonoscopy. Looping of the colonoscope with stretching of the colonic wall and mesentery, distension from air insufflation along with force and torque on the insertion tube, can all lead to significant time to recovery.
As per study protocol, we found that the initial dose of propofol used to reach the target sedation score was significantly less in the ketamine group. Ketamine has a unique property of being a powerful analgesic even at sub-hypnotic doses. The dose of ketamine used was 0.5 mg/kg which is much less than the conventional anaesthetic dose. However, It was found that dose of ketamine had a significant “propofol sparing effect” when compared to the use of the narcotic analgesic, fentanyl.
Propofol has little or no analgesic property of its own; hence ketamine might complement the powerful hypnotic properties of propofol with its profound analgesic effects at relatively low doses. Ketamine- propofol combinations are attractive because of the opposing haemodynamic and respiratory effects of these two drugs and the analgesic property of ketamine at low doses have been previously used in a number of studies.
In a prospective study conducted by Jenifer et al., in 40 pediatric patients; one group received midazolam fentanyl combination for sedation while other group received ketamine, it was found that children sedated with ketamine were quieter, but had occasional movements during the procedure than fentanyl midazolam group. The findings were comparable to our findings where the requirement for additional dose of sedative was less in ketamine group than fentanyl group [6].
In another prospective randomised study conducted in 97 patients sedated with midazolam/ fentanyl /ketamine and midazolam/fentanyl/ placebo along with additional doses of propofol, ketamine group the need for jaw thrust, mask ventilation and disruptive movements were significantly less and gastroenterologist satisfaction was more. Haemodynamic stability was more with ketamine group [7].
Ketamine-propofol combination has also been shown to have a significant “opioid sparing effect” when used in outpatients undergoing breast biopsy [8]. Our study showed that in the ketamine group, patients reached the target sedation level (Ramsay Sedation Score of 5) significantly earlier than in the fentanyl group. This is as expected based on the pharmacokinetic properties of these agents; ketamine has a much quicker onset of action, resulting in a peak effect in 30 seconds. The onset of action of fentanyl is much slower, with the peak effect taking 1-3 minutes. The more rapid onset of action of ketamine may be an added advantage, especially in a busy outpatient surgical practice, with constraint on time.
In another study conducted by Mohammadreza K et al., where 80 adult patients were studied for sedation in two groups, one with fentanyl/propofol and another with ketamine/ propofol for colonoscopies; the mean patient satisfaction scores were more for ketamine/ propofol group than fentanyl group [9]. This was comparable to our study where the time for sedation and recovery time was much lesser in ketamine group than fentanyl group. The overall patient satisfaction was also higher in ketamine group in our study. The haemodynamic variations were comparable in our study.
Data suggests that ketamine decreases airway resistance, improves dynamic compliance and preserves functional residual capacity, minute ventilation and tidal volume while maintaining protective airway reflexes when given as IV infusion in intubated patient [10].
The cardiovascular stability that ketamine offers is an obvious advantage, especially in patients with poor reserves. The stimulant effect that ketamine has on the cardiovascular system sets it apart from other parenteral anaesthetic agents. This is inspite of its direct negative inotropic effect. It causes an increase in heart rate, systemic and pulmonary vascular resistances leading to increased pulmonary arterial and systemic pressures [11]. The concomitant administration of clonidine, a α2-catecholamine receptor agonist that blocks the release of norepinephrine by sympathetic nerves, significantly reduces the sympathomimetic effects of ketamine [12]. The continuous infusion of esmolol, a beta 1 receptor blocker, reduced the inotropic and chronotropic effects on the heart in a dose-related manner [13].
There is also some evidence that ketamine has a direct adrenergic effect by binding directly to alpha and beta adrenergic receptors. These observations strongly suggest that the sympathomimetic effects of ketamine are due to a combination of centrally mediated increased sympathetic nervous system stimulation, a possible direct effect, and the effect of ketamine in blocking the re-uptake of catecholamines.
Cardiovascular stability has been reported in cardiac surgery patients under anaesthesia induced by ketamine and diazepam or midazolam. However, Marlow R et al., reported significant increases in heart rate and blood pressure following intubation of primarily hypertensive patients after induction of anaesthesia with ketamine and midazolam [14].
We used the modified Aldrete Score of 9 to denote recovery from anaesthetic effect. Patients in the ketamine group reached recovery criteria significantly earlier than those in the fentanyl group. Earlier recovery with the ketamine-propofol combination compared to the fentanyl-propofol combination has also been the finding of the study by Messenger D et al., [15]. It appears that ketamine might have a significant role to play in day case anaesthesia where quick and clear headed recovery would be an essential requirement. The study included 63 patients who underwent orthopedic procedures involving the upper and lower limbs. The dose of ketamine used was 0.3 mg/kg compared to 0.5 mg/kg in our study. Patient’s perception of pain, recall and satisfaction ratings were comparable in both the groups in this study. Besides, most of the subjects of this study underwent orthopedic procedures involving the upper and lower limbs, which is likely to cause more pain and discomfort compared to colonoscopies.
We found that the subjective feeling of nausea by VAS was significantly less in the ketamine group. In a study of 100 patients who were divided into 3 groups of varying doses of ketamine along with propofol on women undergoing breast biopsy, the incidence of nausea was high in patients who received higher doses of ketamine compared to placebo [8]. However, the dose of ketamine that we used in our patients was less than the high-dose ketamine arm of this study.
Akin A et al. conducted a randomised controlled trial on 40 patients who underwent endometrial biopsy. Patients were randomised to receive a combination of ketamine-propofol or fentanyl-propofol. The dose of ketamine used was 0.5mg/kg, as we did in our study. They found that the ketamine-propofol was safe and efficacious; however, the patient satisfaction was higher in the fentanyl group [16]. We feel that the results of this trial should be interpreted with caution given the small sample size of only 20 patients in each arm. The incidence of nausea was higher with ketamine-propofol combination compared to fentanyl-propofol combination.
In another prospective randomised trial two groups were compared, group I received 100 mg ketamine and 200 mg propofol and group II received 50 mg ketamine and 200 mg propofol. Both groups were maintained with propofol boluses of 0.5 mg/kg titrated to adverse effects. The presence of adverse effects was significantly lower in group II and the total dose of propofol used was also less. The overall patient satisfaction was more with higher doses of ketamine. Thus, increasing the dose of ketamine or addition of ketamine to propofol than using plain propofol as done in our study was found to have a beneficial effect in view of haemodynamic stability or patient satisfaction [17].
In a study comparing 0.5 mg/kg ketamine and 1 mg/kg propofol (Group KP) with 10 μg/kg Alfentanil and 1mg/kg propofol (Group AP), it was found that Ramsay Sedation Score and discharge times were significantly higher in KP group than AP group. The need for additional dose for propofol was more with Group AP. Ketofol provided better haemodynamic stability and quality of sedation compared with alfentanil- propofol combination. These results were comparable with our findings where ketamine propofol combination had a better patient satisfaction [18].
We asked the endoscopist who conducted the colonoscopy to rate the level of satisfaction with the anaesthetic experience on a 0-10 VAS with 0 indicating least and 10 indicating highest level of satisfaction. The level of satisfaction on the VAS was comparable between the ketamine and the fentanyl groups.
We encountered no incidence of emergence phenomena in our study that are well-known to occur with the use of ketamine. We believe that this is mainly due to the low dose of ketamine that we used in our study. Previous studies have also shown a low incidence of dreams and hallucinations when ketamine is used in a low, sub-hypnotic doses. The use of propofol, which characteristically results in a calm and peaceful sleep, also may have mitigated the adverse emergence effects of ketamine. Previous studies have shown that propofol may, in fact, reduce the emergence phenomena seen with ketamine [19]. Midazolam may also have contributed to the absence of emergence phenomena that characterised our study.
Limitation
This study has several limitations. It would have been ideal to conduct the study in a blinded manner. However, technical difficulties arose with the blinding of syringes and also in finding appropriately trained staff that could document relevant information and database them, especially in the recovery area. Time constraints meant that senior nursing staff could not be recruited from the recovery area for the conduct of the study. However a bigger sample size would probably have meant more meaningful results and less likelihood of a type I error.
Conclusion
The present study shows that midazolam/ketamine /propofol combination provides adequate levels of analgesia and sedation, quicker recovery and has “propofol sparing” effect. Patients may be haemodynamically more stable with a lower incidence of significant hypotension. There is a distinct lack of emergence phenomena associated with a sub-hypnotic dose of ketamine. Patient satisfaction was higher in ketamine group. Thus, midazolam/ketamine/propofol is an effective drug combination that can be used as sedation for colonoscopies.
*Highly significant (p≤0.001), **Significant (p≤0.05), ***Not significant (p>0.05)