Umbilical Pilonidal Sinus-Experience at a Peripheral (Rural) Hospital
Piyush Gupta1, Pallavi Gupta2
1 Graded Surgeon, Department of Surgery, 162 Military Hospital Dinjan, Dibrugarh, Assam, India.
2 Surgeon, Department of Surgery, 162 Military Hospital Dinjan, Dibrugarh, Assam, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Piyush Gupta, Graded Surgeon, Department of Surgery, 162 Military Hospital Dinjan, Dibrugarh-786189, Assam, India.
E-mail: piyush_gupta18@rediffmail.com
Barber, Hair, Umbilical discharge
Dear Editor,
We are delighted to go through the article titled, “Umbilical Pilonidal Sinus: A Report of Two Cases and Recent Update of Literature” by Meher S et al., which was published online in Sep 2016 [1].
We would like to share our experience as rural surgeons in handling two cases of Umbilical pilonidal sinus in a remote area of Assam. The clinical suspicion is the mainstay in diagnosis since there is no known biochemical or radiological markers thus, the dilemmas in diagnosis and management which followed are worth a share.
Case 1
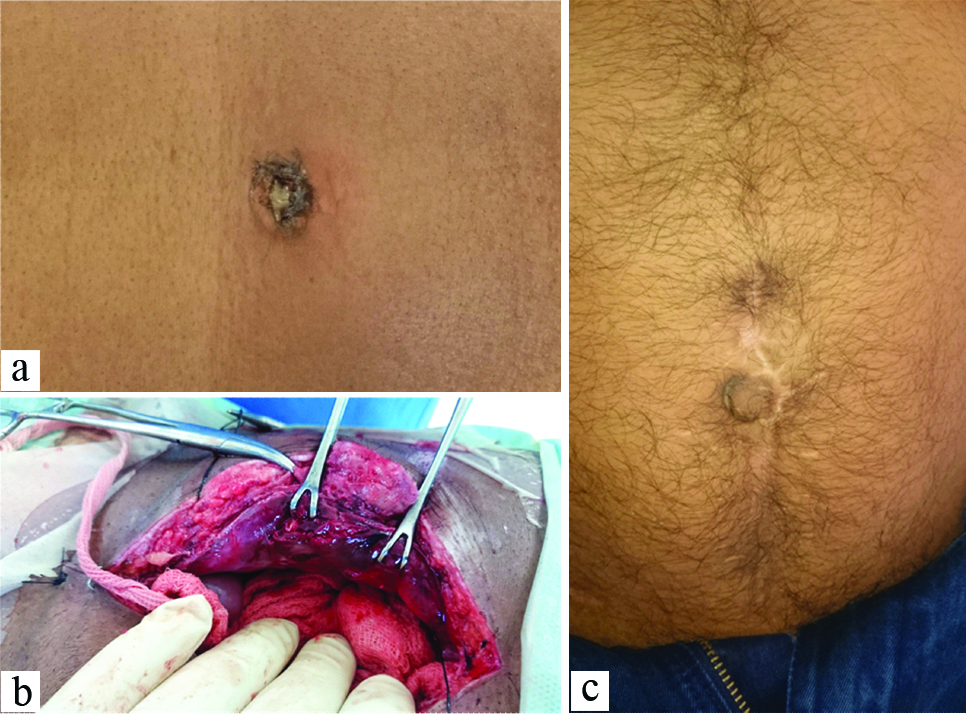
A 32-year-old man was brought with 10 days history of progressively severe pain felt all over the abdomen. He was running fever (T-100°F) with guarding and tenderness all over the abdomen. Pus discharge was seen at umbilicus which was seropurulent [Table/Fig-1a] and foul smelling. There were no other Gastrointestinal (GI) or Urinary features present; Hb-12 gm% and TLC-13,300 cumm. X-ray (only available imaging modality in this hospital) chest and abdomen- inconclusive. In view of the above features of peritonism a decision to proceed with emergency laparotomy was taken. Initially a small midline vertical incision was given to access the peritoneal cavity. We noticed inflamed rectus muscle on both sides [Table/Fig-1b] and no pus in peritoneal cavity. The contents inside were unremarkable. We examined the umbilicus again and tracked the pus in abdominal wall itself 1 cm around umbilicus. A small tuft of hair was also found and removed. Umbilical wound was washed and left to heal secondarily, and the laparotomy incision was closed in standard way. Postoperative care with i.v. antibiotics, daily wound care and early mobilisation was done. The patient’s recovery was uneventful even after one year of follow-up, there was no recurrence [Table/Fig-1c]. Interestingly, during the interaction he revealed to us that he was a barber by trade and did not use any apron while performing his act.
a) Preoperative presentation of a discharging umbilicus is seen; b) On peroperative was found to have oedematous and inflamed rectus muscle and abdominal wall; c) Postoperative image of a healthy umbilicus with healed laparotomy wound.
Case 2
A 26-year-old man came with a three day history of painful umbilicus with discharge. He had no fever or any other systemic features. Clinically, there was a seropurulent discharge at the umbilicus [Table/Fig-2] along with erythema and tenderness in periumbilical region. Routine laboratory investigations were within normal limits. He was taken up for an early incision and drainage with debridement of umbilicus. A similar tuft of hair in a small subcutaneous tract was discovered which was removed and excision of the tract was done. Wound healed with secondary intention and oral antibiotics for 5-7 days. One year follow-up in this case was also unremarkable and to our surprise he was also a barber by trade with similar professional practices.
Preoperative presentation of discharging umbilicus in the second case.

Discussion
We appreciate the extensive review of literature done by the authors. However, in aetiopathogensis, it was mentioned that jeep drivers being commonly affected. I would like to offer a clarification that jeep drivers of Second World War suffered from pilonidal sinus-sacro coccygeal and not umbilical pilonidal sinus [2]. Also, we would like to add a few points about investigation in such cases-diagnostic laparoscopy would be of immense help if available, with only difference that first port placement be at Palmar’s point. Non invasive investigations like sonography [3] may help to rule out other differential diagnosis in purulent umbilicus.
Risk factors like being a hair dresser, wearing tight clothing, poor personal hygiene and male gender seem to be significant as brought out by Meher S et al., as well [1]. Regarding management, we are in full agreement to the line of management as described.
To conclude, pilonidal sinus is a peculiar entity which has been perturbing since days of world war and gained popular name of ’jeep bottoms’. However, its occurrence at other parts of the body continues to be a rarity. The accessibility of hair as aetiological factor is an established fact however, it can be regarded as professional hazard as in these two cases we need further studies and multi centre observations.
[1]. Meher S, Mishra TS, Sasmal PK, Sharma R, Rout B, Umbilical pilonidal sinus: a report of two cases and recent update of literatureJ Clin Diagn Res 2016 10(9):PD20-PD22.10.7860/JCDR/2016/20251.856927790519 [Google Scholar] [CrossRef] [PubMed]
[2]. Norman S Williams, The Anus and Anal canalIn: Bailey & Love’s Short Practice of Surgery 2004 24th ednNew YorkArnold Publishers:1249 [Google Scholar]
[3]. Sharma V, Umbilical discharge and its management in adults-rare presentationIOSR Journal of Dental and Medical Sciences 2014 13(7):45-48.10.9790/0853-13744548 [Google Scholar] [CrossRef]