Hyperlipidemia is a disorder of abnormally elevated levels of any or all types of serum lipids and/or serum lipoproteins in the blood. It is the most common form of dyslipidemia. It may be primary, secondary or idiopathic. It is a common risk factor for myocardial infarction and stroke [1,2]. In India, prevalence of hypercholesterolemia is 13.9%, hypertriglyceridemia is 29.5%, high LDL is 11.8% and low HDL is 72.3% [3]. Statins are the most commonly used drugs for the treatment of hyperlipidemias [4]. They lower the cholesterol level by inhibition of HMG-CoA reductase enzyme, which is the rate-limiting enzyme in the synthesis of cholesterol [5]. They also cause a dose-dependent reduction in plasma LDL and triglycerides. They have modest HDL raising effect which is not dose-dependent [6].
Apart from being used to treat hyperlipidemia, they are also used for primary as well as secondary prevention of cardiovascular diseases like angina, myocardial infarction and stroke [7]. Considering the high prevalence rates of hyperlipidemia and cardiovascular diseases, number of patients taking one or other statin are huge. Recently, there have been several case reports of pancreatitis in patients on statin therapy. Cases of pancreatitis have been reported in patients taking lovastatin, fluvastatin, rosuvastatin, atorvastatin, simvastatin and pravastatin [8,9]. Based on this background, the present study was carried out with the aim to study the occurrence of pancreatitis in patients taking atorvastatin. This was assessed by evaluating changes in serum levels of lipase and amylase from their baseline value to three months post-treatment in patients who were newly started on atorvastatin therapy.
Materials and Methods
This was a prospective, observational study carried out over a period of one year in the Department of Medicine, New Civil Hospital, Surat, Gujarat, India, after getting approval from Scientific Review Committee and Institutional Ethical Committee.
Inclusion criteria: Newly diagnosed patients of hyperlipidaemia belonging to all age groups and both genders were included in the study. These patients were started on statin therapy for the first time.
Exclusion criteria: Patients with hypertriglyceridemia, cholecystitis, salivary gland infection, intestinal obstruction and pancreatic cancer were excluded from the study. Patients with a history of alcohol consumption, recent abdominal trauma or gastrointestinal surgery were excluded from the study. Also, patients who were concurrently taking drugs which are known to cause pancreatitis as an adverse effect, namely, corticosteroids, azathioprine, sulfonamides, tetracycline, anti-HIV medications, valproic acid, thiazides and oestrogens were excluded from the study.
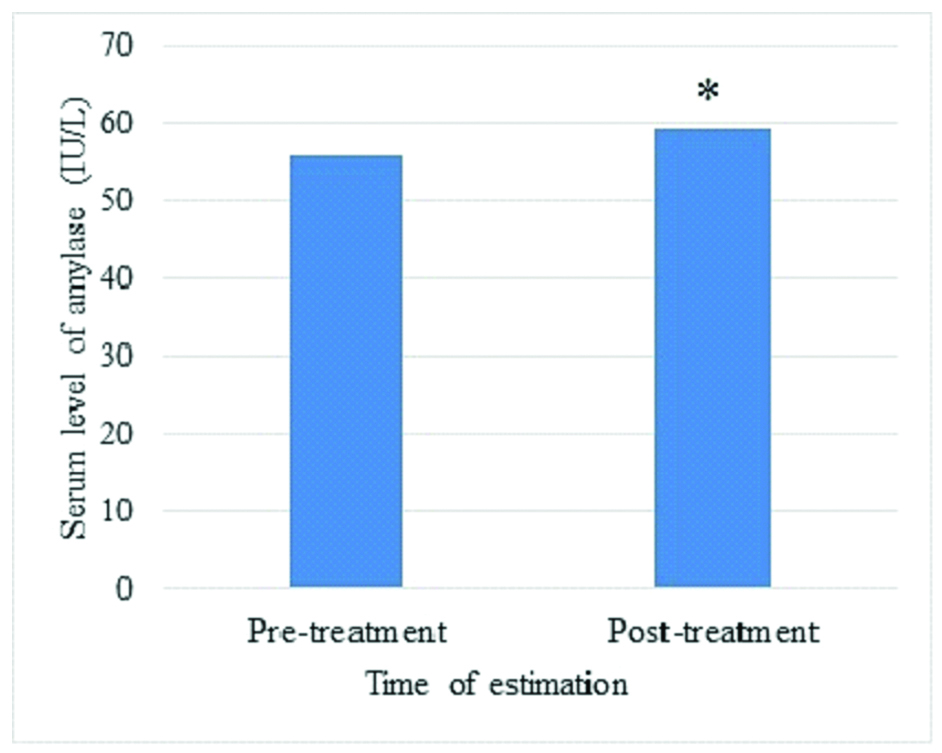
Based on the inclusion and exclusion criteria, a total of 72 patients, who attended the Medicine Outpatient Department and were diagnosed with hyperlipidemia, were enrolled in the study after obtaining a written informed consent from them. The patient’s demographic details, relevant medical history and specifications regarding treatment given were recorded in a predesigned, pre-approved patient data sheet. All the patients diagnosed with hyperlipidemia were prescribed tablet atorvastatin 20 mg at bedtime for 90 days by the physician from Department of Medicine. Atorvastatin was the most frequently prescribed statin in the present set up. It was easily available from the pharmacy of present hospital, as it was one of the routinely supplied statin drugs to the hospital. Drugs for other concurrent ailments were also prescribed. Patients were given patient compliance card in which they had to tick mark after taking the drug. Follow-up visit was done after 90 days of continuous statin therapy. Only compliant (consumption of ≥80% medications according to the prescription) patients were considered eligible for follow-up measurement of serum lipase and amylase. Compliance with the treatment was measured as per the following formula [10]:
Collection of Blood Samples
Two fasting blood samples were collected from each patient during the study for analysis of serum lipase and amylase and serum lipid profile. Patients were duly instructed not to eat or drink anything except plain water on the day of the test for 12 hours prior to blood draw. First baseline sample was collected at the onset of statin therapy and second sample was collected three months later with continued statin therapy. Serum lipase level was measured by turbidimetry method [11]. Serum cholesterol was measured by the cholesterol oxidase method [12]. Triglyceride was measured using ready to use triglyceride kit from Randox Laboratories Limited. HDL cholesterol was measured by polyethylene glycol modified enzymes [13]. LDL and VLDL were measured by an indirect method using Friedewald equation [14].
Statistical Analysis
All values are expressed as mean±standard deviation. Comparison of pre-treatment and post-treatment serum lipase and amylase levels was done using two tailed paired sample t-test. A p-value <0.05 was considered as statistically significant. SPSS version 23.0 was used for statistical analysis.
Results
Out of the 72 patients enrolled in the study, 60 patients were compliant with their treatment and were included in the final evaluation of results. Amongst them, 55% (n=33) were female and 45% (n=27) were male. Mean age of the study population was 56.87±9.42 years.
All the patients were suffering from at least one concurrent ailment. Hypertension was the most frequent concurrent disease in the study population. Medications were prescribed along with atorvastatin for these concurrent ailments. The names of concurrent ailments for which additional drug(s) were prescribed and also the number of patients suffering from them are given in [Table/Fig-1].
Distribution of concurrent ailments in the study population.
| Disease | Number of patients (n) | Percentage (%) |
|---|
| Hypertension | 38 | 63.33 |
| Diabetes mellitus | 32 | 53.33 |
| Ischemic heart disease | 11 | 18.33 |
| Common cold | 3 | 5.00 |
| Congestive Heart Failure | 3 | 5.00 |
| Hypothyroidism | 2 | 3.33 |
| Malaria | 2 | 3.33 |
| Ligament sprain | 2 | 3.33 |
| Nephrotic syndrome | 1 | 1.67 |
| Hypertensive nephropathy | 1 | 1.67 |
| Fungal infection | 1 | 1.67 |
| Epilepsy | 1 | 1.67 |
| TIA | 1 | 1.67 |
| Fibroadenoma | 1 | 1.67 |
Serum Lipid Profile
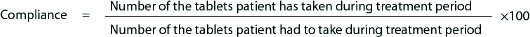
As shown in the [Table/Fig-2], there was a significant fall in total cholesterol, LDL cholesterol, VLDL cholesterol and triglyceride and a significant rise in HDL cholesterol after 90 days of treatment with atorvastatin in the hyperlipidemic patients. A p-value of less than 0.05 was considered significant.
Comparison between pre-treatment and post-treatment serum lipid levels.
*p=0.0017 Significant fall in the post-treatment levels; #p=0.005 Significant rise in the post-treatment levels; p<0.05 level of significance, using two tailed paired sample t-test.
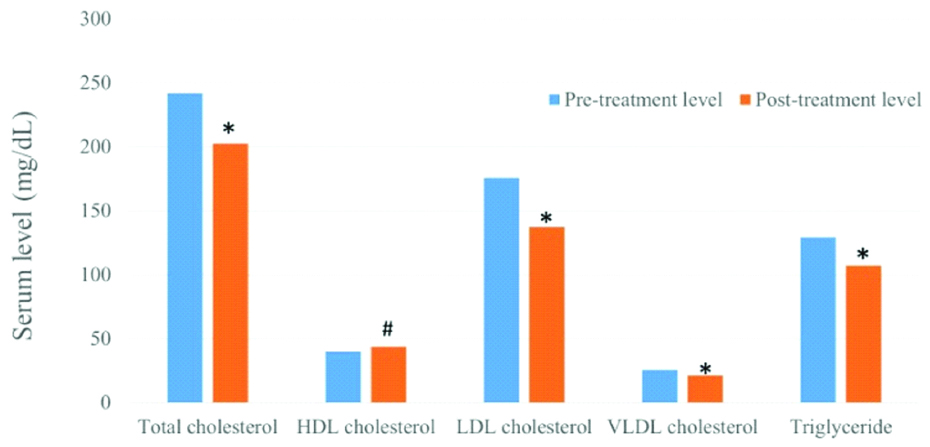
Serum lipase: The mean pre-treatment serum lipase level in the study population was 32.17±10.33 U/L which was in the normal range for all the patients. There was a significant increase in serum lipase levels post-treatment (35.23±10.14 U/L, p=0.016). The comparison between pre-treatment and post-treatment serum lipase levels are shown in [Table/Fig-3].
Gives the comparison between pre-treatment and post-treatment serum lipase levels.
*p=0.016 significant rise in serum lipase level. p<0.05 Level of significance, using two tailed paired sample t-test.
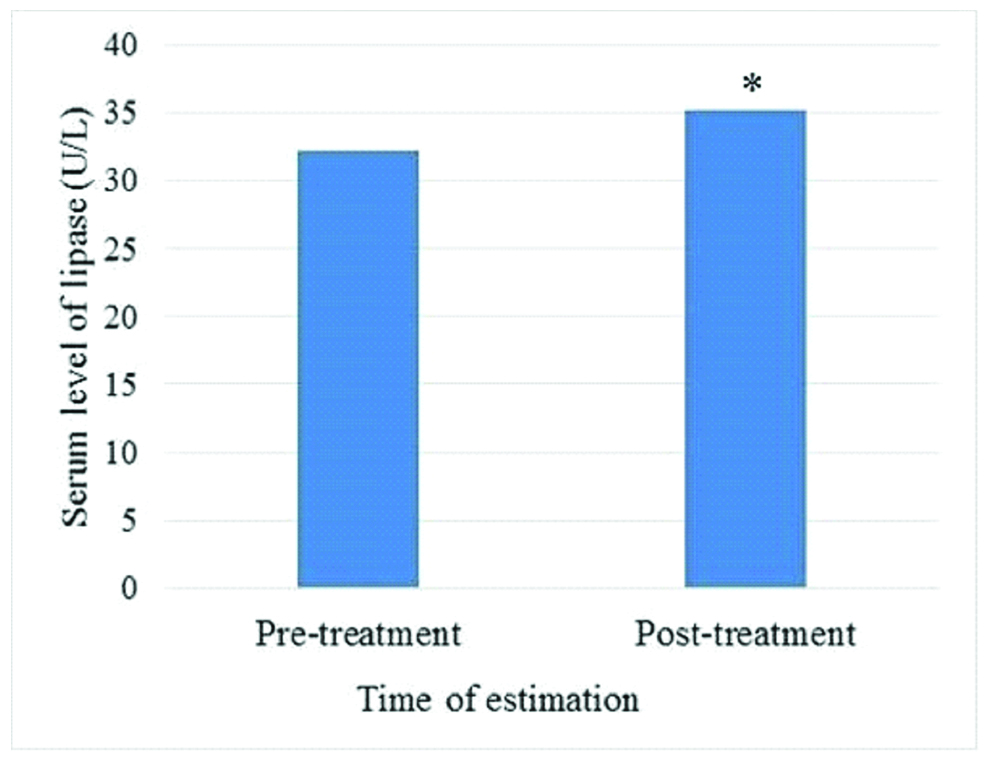
Serum amylase: Mean pre-treatment serum amylase level in the study population was 55.92±17.54 IU/L which was in the normal range for all patients. There was a significant increase in serum amylase levels after 90 days of treatment (59.40±15.28 IU/L, p=0.038). The comparison between pre-treatment and post-treatment serum amylase levels are shown in [Table/Fig-4].
Pre-treatment and Post-treatment values of serum amylase.
*p=0.038 significant rise in serum amylase level. p<0.05 Level of significance, using two tailed paired sample t-test.
Discussion
Hyperlipidemia or abnormal blood lipid levels, as an individual entity, is considered as a major risk factor for various cardiovascular diseases and stroke. Along with lifestyle modifications, pharmacological treatment is the mainstay of therapy for hyperlipidemia. Among the various groups of drugs used to treat hyperlipidemia, statins are the most commonly prescribed. There has been considerable evidence with regard to the efficacy and safety of usage of these drugs in hyperlipidemia. However, recently there have been various case reports suggesting an increased risk of pancreatitis with the use of statin therapy in the patients of hyperlipidemia [8,9].
In the study population, there was a preponderance of female patients (55%) which was not deliberate. Mean age of the study population was 56.87±9.42 years. Apart from hyperlipidemia, all the patients suffered from at least one concurrent disease. Amongst the concurrent diseases, hypertension was most common followed by diabetes mellitus and ischaemic heart disease. Because of the same reason, the patients were prescribed various concomitant drugs. Multivitamins, omeprazole, aspirin, metformin, amlodipine and enalapril were prescribed more frequently.
Lipid profile, which showed hyperlipidemia on the baseline investigation, showed a fall in serum total cholesterol, LDL cholesterol, VLDL cholesterol and triglyceride level and an increase in serum HDL cholesterol level in the blood sample collected on the 90-day follow-up visit. This illustrates the compliance as well as the effectiveness of the atorvastatin treatment in these patients.
The levels of serum amylase and lipase were within normal physiological range at the first visit (baseline) in all the patients. However, their levels were increased at the second visit (90-day post-treatment) and this increase was statistically significant for serum lipase as well as serum amylase. None of the patients developed clinically overt pancreatitis during the study period.
Lipase and amylase are digestive enzymes secreted by the pancreas. They are mainly secreted in the gastrointestinal tract and their levels in serum are normally found to be low. However, their levels in serum are increased in pancreatic pathologies [15]. In the present study, serum levels of both lipase and amylase were found to be significantly elevated after 90 days of atorvastatin treatment. The possibility of presence of already known causes of elevation in serum lipase and amylase were ruled out during enrollment. So it can be hypothesised that elevation in serum levels of lipase and amylase was due to atorvastatin. This is similar to the findings suggested in a case report by Prajapati S et al., of a 58-year-old male who developed pancreatitis while on atorvastatin therapy. He recovered completely within 10 days of atorvastatin withdrawal [16].
The mechanism behind statin-induced pancreatitis is yet ill defined. Pancreatitis is reported with multiple statins. Thus, statin induced pancreatitis appears to be a class effect rather than being associated with any particular statin only. This suggests that statin induced pancreatitis may be related to its pharmacological action which is inhibition of HMG CoA reductase as this property is shared by all the statins. Immune mediated inflammatory response, direct cellular toxicity, metabolic effects and drug-drug interaction through CYP3A4 are commonly postulated mechanisms among previously reported cases [8].
So far, the evidence suggesting a possible link between pancreatitis and statins are in the form of individual case reports only. In one case report, a 67-year-old female suffered from recurrent acute pancreatitis. She was on rosuvastatin therapy for hyperlipidemia. Pancreatitis did not recur after stopping the rosuvastatin [9]. On causality assessment scales, most of the case reports showed statins as the possible/likely cause of pancreatitis [17]. The present study shows elevation in serum lipase and amylase in patients on atorvastatin. Moreover, the most likely source of this elevation appears to be pancreas. Thus, the findings of this study support statins as a cause of pancreatitis in previously reported cases.
Serum amylase level is also elevated in conditions other than pancreatitis like salivary gland disease, intestinal disease and female reproductive tract disease [18]. Because of this, specificity of amylase alone for pancreatic pathology is only 20-60% [19]. However, serum lipase is more specific for pancreatic pathology. Specificity of lipase alone for pancreatic pathology is more than 80% [19]. Moreover combining these two parameters increases the specificity to 97-98% [20]. In the present study, serum amylase and lipase both were studied and both were found to be elevated. A combination of both the enzymes is more specific for pancreatic pathology, their elevated levels can be considered to be due to some kind of damage to pancreas rather than any other pathology. Moreover, patients with aetiological factors (including drugs) which are already known to cause pancreatitis were excluded from the study. This made it possible to consider that elevation in serum lipase and amylase to be due to atorvastatin.
Limitation
As the study being done was for postgraduate dissertation study with time limit, only one statin drug, atorvastatin, was considered in this study. Thus, the association of pancreatic damage with other statins could not be conclusively reported. Also, all the patients received multiple drugs including atorvastatin. Although, none of the drugs prescribed along with atorvastatin are known to cause pancreatitis yet, possibility of elevation in serum lipase and amylase to be due to these drugs also cannot be ruled out. Moreover, time of appearance of pancreatitis after onset of statin therapy has varied widely in previously reported cases. This period ranges from 1 day to few years [17]. However in the present study, follow-up for serum lipase and amylase level was done at 90th day (three months later). Because of this, impact of changes in serum lipase and amylase level occurring before three months and those occurring after three months could not be studied. Also, in the present study no tests were carried out to explore underlying mechanism of statin induced changes in the levels of serum amylase and lipase because of ethical concerns.
Conclusion
Statins are widely used in therapeutics. They are generally well tolerated and side effects associated with them are relatively rare. From the present study, It can be concluded that there is some association between statin use and pancreatic injury. Thus, statins should be used cautiously in the patients who are already at higher risk of developing pancreatitis. In patients developing pancreatitis, physician should consider stopping statin permanently and switching to another lipid lowering therapy. The causal association between drug and the event in such cases should be assessed and it should be reported under the pharmacovigilance program to widen the spectrum and make statin usage safer. In future, large scale studies assessing risk of pancreatitis in patients on statin therapy and experimental studies to explore the underlying mechanisms are needed.