Sleep disorders are common in the general population and affect 16.6%-40% of the world population [1,2]. Medical students are one subgroup of the general population, who appear to be particularly vulnerable to poor sleep quality, perhaps because of the high academic demands, clinical duties, lifestyle choices, and emotionally challenging work [3]. Furthermore, poor sleep quality is more common in the medical students than in the non-medical students [4]. Poor sleep quality affects cognitive functions and may lead to psychiatric disorders, psychosocial stress, reduced work efficiency, poor academic performance, and low quality of healthcare delivery [5].
Various factors, such as an individual’s personality, cognitive style, physical or mental illness, and sleep environment conditions, may contribute to the sleep architecture of the medical students [6]. Knowledge regarding the association between the personality traits of an individual and sleep quality is limited. Maladaptive personality traits are associated with an increased risk of sleep disorders and mental illnesses [7]. Mental illnesses, such as anxiety, depression, acute stress reaction, and psychotic disorder, may cause sleep disorders and vice versa [8-10].
Previous studies have attempted to explore the relationship between personality traits and circadian typology and sleep quality and quantity [11-13]. Tonetti L et al., found that the evening types were associated with higher impulsive sensation seeking scores than morning types, whereas the morning types scored higher than the evening types on the activity factor [11]. Furthermore, other studies have shown that individuals high in neuroticism traits have sleep problems-associated cognitive recitation and are over concerned about uncontrolled life events, leading to sympathetic hyperarousal [14-18].
Extraversion and conscientiousness are personality traits crucial for long-term success in medical training, whereas neuroticism is associated with poor academic outcome [19-22]. Therefore, the underlying personality traits may affect both the sleep quality and academic performance of medical students. The present study investigated the possible relationship between personality traits and sleep quality among medical students.
Materials and Methods
This study was a cross-sectional study involving a single time assessment conducted over two months (August 2015–September 2015) in a rural medical college in central India. The consent and all research procedures were reviewed and approved by the Institutional Ethical Committee of MGIMS, Sevagram. A detailed screening interview was conducted before recruiting the study subjects. All medical students from first and second year MBBS and willing to participate were included in the study. The subjects with a history of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) axis I psychopathology, sleep disorders or using sleep medications, substance use disorders, or serious neurological and medical disorders were excluded from the study.
Measures:
The subjects were evaluated for their socio-demographic profile, by using the Eysenck Personality Questionnaire (EPQ-R) Short Scale [23] and Pittsburgh Sleep Quality Index (PSQI) [24].
PSQI: It is a 19-item survey that assesses sleep quality over the previous month and yields seven subscales [24]. The responses are scored on a 3-point scale ranging from 0 (No difficulty during the past month) to 3 (severe difficulty i.e. three or more times a week). This score has been used to measure sleep quality among adults [25] and university students [26]. A higher score indicates poor sleep quality, and a global score of 5 has been established as the clinical cut-off. In our study, we excluded the medical students having sleep disorder or using sleep medications. Therefore, component 6 of scale (i.e., use of sleep medication) was not considered for final analysis.
EPQ-R Short Scale: It is a 48-self-report questionnaire that assesses the dimensions of personality, neuroticism, extraversion, and psychoticism. There are 12 questionnaires for each dimension of personality. Response for each question is binary i.e., ‘Yes’ or ‘No’. The ‘yes’ response is scored with 1 and ‘No’ response in scored with zero. Thus, each dimension has maximum score of 12 and minimum score of zero. Furthermore, it includes a Lie scale. The three psychometrics scales (Psychoticism, Extraversion, and Neuroticism) are predicted upon biologically based theory of personality [23].
Statistical Analysis
Quantitative and qualitative data for socio-demographic and clinical variables were analysed using SPSS 20.0 version and Graph pad prism 5.0 version. Student’s t-test was used to compare the scores of personality traits of the individuals with poor and good sleep quality. To evaluate qualitative variables, chi-square test and Fisher’s-exact tests were used. Pearson correlations were used to examine the relationship among personality traits, global scores, and subscales of the PSQI. The results were presented as mean±SD, and p<0.05 was considered statistically significant for all comparisons.
Results
Among 240 students, 34 students refused to participate in the study and 40 students failed to fulfill the eligibility criteria. The remaining 166 students were then recruited in the index study. [Table/Fig-1] shows the clinical and descriptive characteristics of the study population. The mean age of the students was 20.93±1.86 years. Most of the subjects were male (89 of the 166 subjects, 53.61%). Of the 166 subjects, 54 (32.53%) reported a poor sleep pattern on the PSQI. The prevalence of poor sleep quality was higher among the female subjects (28 of the 77 subjects, 36.36%) than among the male subjects (26 of the 89 subjects, 29.21%). However, the difference was statistically insignificant (Fisher’s-exact-test, p=0.40).
Comparison of male and female subjects in terms of PSQI global score and EPQ subscales.
| Variables | Overall (n=166) | Male (n=89) (Mean±SD) | Female (n=77) (Mean±SD) | t-test (Scores between male and female subjects) |
|---|
| Global score (PSQI) | 3.64±2.25 | 3.56±2.10 | 3.70±2.49 | t=0.50, p=0.61 |
| Psychoticism | 3.45±1.76 | 3.88±1.78 | 2.95±1.58 | t=3.57, p<0.001 |
| Neuroticism | 4.89±2.86 | 4.33±2.73 | 5.53±2.92 | t=2.73, p<0.001 |
| Extraversion | 7.79±2.99 | 7.79±2.73 | 7.78±3.24 | t=0.01, p=0.98 |
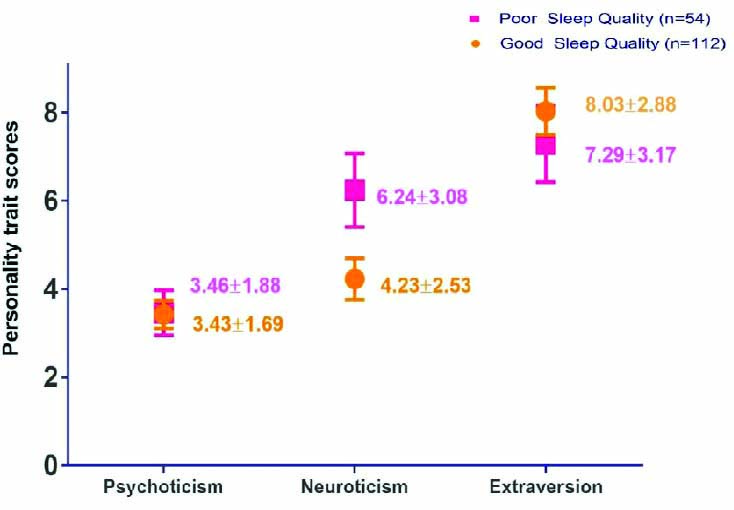
Higher score on psychoticism was observed among the male subjects (3.88±1.78) than among the female subjects (2.95±1.58), and significant difference was observed (p<0.001). The female subjects (5.53±2.92) were more neurotic than the male subjects (4.33±2.73, p<0.001). [Table/Fig-2] shows the comparison between the students with poor sleep quality and those with good sleep quality on the PSQI. The neuroticism score was higher among the students with poor sleep quality (6.24±3.08) than among those with good sleep quality (4.23±2.52), and the difference was highly significant (p<0.001). A non-significant difference was observed in the psychoticism trait among the students with good (3.43±1.69) and poor sleep quality (3.46±1.88, p= 0.93). The students with good sleep quality (8.03±2.88) showed a higher extraversion score than those with poor sleep quality (7.29±3.17); however, no significant difference was observed (p =0.13).
Comparison of personality traits between subjects with poor and good sleep quality.
To explore the strength of the association among personality traits, global score, and subscales of the PSQI, Pearson’s correlational analysis was performed. The correlational analysis showed that neuroticism was positively and significantly correlated with the global score (r = 0.39, p<0.001), daytime dysfunctions (r=0.44, p<0.001), and poor subjective sleep quality (r=0.27, p<0.001). Extraversion was negatively correlated with the global score (r=−0.16, p=0.03) and daytime dysfunctions (r=−0.20, p<0.01) [Table/Fig-3]. No significant correlation was observed between the age of the subjects and global score on the PSQI (r=−0.08, p=0.29). No significant relationship was observed between psychoticism and subscales of the sleep quality index.
Pearson’s correlation among personality traits, global score, and subscales.
| Personality traits/subscales | Subjective sleep quality | Sleep latency | Sleep duration | Sleep efficiency | Sleep disturbances | Daytime dysfunctions | Global score |
|---|
| Psychoticism | −0.05 (p=0.50) | 0.24 (p=0.50) | 0.004 (p=0.94) | −0.11(p=0.15) | −0.03 (p=0.62) | 0.09 (p=0.22) | 0.06 (p=0.44) |
| Neuroticism | 0.27*** p<0.001) | 0.34** (p=0.01) | 0.10 (p=0.16) | −0.01 (p=0.89) | 0.21** (p=0.004) | 0.44*** (p<0.001) | 0.39*** (p<0.001) |
| Extraversion | −0.12 (p=0.12) | -0.18 (p=0.28) | 0.048 (p=0.53) | −0.02 (p=0.78) | −0.04 (p=0.60) | −0.20** (p=0.007) | −0.16 * (p=0.03) |
*=p<0.05, **=p<0.01, ***=p<0.001
Discussion
In this study, approximately 32.53% of the medical students showed poor sleep quality on the PSQI, which is in accordance with the results of most studies conducted in Brazil [27,28], Mexico [29], and India [30]. A Chinese study reported 19.15% of medical students with poor sleep quality on the PSQI [31]. However, in Europe, a Lithuanian study revealed poor sleep quality in 40% of the medical students, as measured by the PSQI [32]. Most studies found no gender-based differences in the results [29,31]. Few studies have reported gender-based differences in the results of sleep quality; higher number of males were involved in an Indian study [30], whereas higher number of females were involved in a Brazilian study [27]. Although, we observed poor sleep quality among the female subjects (36.36% vs. 29.21%) than among the male subjects, the difference was not significant. The reason for this could be the high and low scores on neuroticism and psychoticism, respectively. However, further evaluation is required.
The prevalence of poor sleep varies among the studies possibly because of difference in measurement tools, culture, socio-demographic variables, and personality traits of medical students. Furthermore, the prevalence of poor sleep quality is higher in medical students than in the general population and other students. Along with the aforementioned variables, personality traits may be a logical reason for poor sleep quality and vice versa.
To the best of our knowledge, the present study is the first to associate sleep quality with personality traits among Indian medical students. We observed that individuals with poor sleep quality demonstrated higher scores on neuroticism but not on other emotional dimensions. Furthermore, neuroticism was correlated with poor subjective sleep quality, sleep latency, sleep disturbances and daytime dysfunctions. Moreover, it is not related to sleep duration, sleep efficiency, and sleep disturbances. Thus, our findings contribute to the growing literature, suggesting that personality trait–neuroticism may be uniquely predictive of sleep quality [33-35]. Neuroticism must be identified for improving the outcome because it is an intrinsic factor that may be responsible for poor sleep quality. Furthermore, it plays a vital role in the hyperarousal of the autonomic nervous system and over activation of the hypothalamic–pituitary–adrenal axis under stressful conditions, such as examinations and relationship issues [36]. A higher score on neuroticism reflects anxiety, depression, guilt, tension, moodiness, and low self-esteem in an individual, leading to pre-sleep cognition, that is, worrying, planning, analysing, and active thinking during bedtime [37]. Moreover, these individuals report poor subjective quality of sleep, indicating the perceived nature of sleep and daytime dysfunctions.
Although, all the three personality traits are related to sleep disorders, individuals scoring higher on neuroticism and lower on extraversion are more likely to complain about poor sleep quality and excess daytime drowsiness. No significant relationship was observed between the psychoticism score, which reflects aggressiveness, assertiveness, and egocentric and manipulative behavior, and sleep quality. The relationship observed between personality traits and sleep quality in this study is consistent with that observed in previous studies [33-35]. It reflects deficits in cognitive control mediated by the insular and orbitofrontal cortices [38].
According to the Eysenck’s theory of Introversion–Extroversion, introverts demonstrate higher levels of basal activity within the reticular-thalamic-cortical loop, which leads to higher tonic-cortical arousal than extroverts [39]. In present study, the introvert is more prone to poor sleep than an extrovert which is contradictory to Eysenck’s theory. The reason for this may be due to excessive pre-self-cognition and maladaptive attempts to control emotions, among medical students. However, this need to be explored in the future [39]. Future studies may exploit the potentials of the hypothesised brain region for developing potential interventions to improve sleep problems.
Conceptualisation of sleep quality is crucial for medical students because it is directly related to their academic and cognitive performance and minor psychiatric illnesses [40,41]. Our results may be relevant in understanding the influence of personality traits on the cognitive–emotional processing of pre-sleep cognition [33,42]. Further research is warranted to examine the effects of interventions that target these personality traits for improving the overall sleep quality.
Strengths and Limitations
The strengths of our study include an adequate sample size (post-hoc power-80.5%), a population-based, cross-sectional study design, and standardised scales for clinical assessment. However, our results should be interpreted considering few limitations. Although the standardised Pittsburg’s sleep quality questionnaire along with the Eysenck’s personality questionnaire were used to measure sleep quality and personality traits, introducing potential reporter bias, an objective measurement of the sleep pattern, such as polysomnography or actigraphy, could explore the relationship more accurately and effectively. The academic year of medical students, sleep latency, clinical duties, seasonal effects and use of sleep medicine affects the sleep quality. These factors need to be considered in future longitudinal studies. However; our findings provide an insight into the potential contribution of personality traits to sleep quality among medical students.
Conclusion
Poor sleep quality among medical students are related to personality traits, particularly with respect to neuroticism and extraversion, and our study supports the association between them. The present study will help the researchers and clinician working in the field of sleep medicine in expanding their understanding of biopsychological factors influencing sleep quality. The outcome of sleep disorders and academic performance may be improved by considering these relationships among medical students.
Declaration- The present research paper was Presented at MGIMS, Sevagram and received "Dr. Sushila Nayar Memorial Award for Undergraduate Research" on 19th April 2017.
*=p<0.05, **=p<0.01, ***=p<0.001