Growth and development of maxillofacial structures are influenced by genetic and environmental factors. Normal respiratory activity affects the harmonious growth of maxillofacial structures [1,2].
The methods for assessment of Pharyngeal Airway Space (PAS) in orthodontics are very limited. Conventionally, lateral cephalograms were used to determine the craniofacial morphology and possible airway obstruction. Due to its two-dimensional nature, lateral cephalogram has limitations when evaluating three-dimensional pharyngeal airway structures. The Magnetic Resonance Imaging (MRI) technique is being increasingly utilised to identify and evaluate soft tissue morphology, and to quantify pharyngeal size as it is non-invasive and permits accurate three-dimensional measurement of the airway. Among the predisposing factors for constriction of the pharyngeal airway such as allergies, environmental irritants, and infections, which are amenable to adequate treatment, there is also the natural anatomical predisposition to narrower airway passages [3-5]. Kirjavainen M et al., found that the oro- and hypopharynx were narrowed in Angle Class II Division 1 patients [6]. Hence, retrognathic mandible is one of the anatomic predisposing factors. Patients with narrower pharyngeal airway are more susceptible to mechanical collapse under the negative pressure of inspiration. Concomitant reductions in tone and abnormal muscle behaviour further favours airway occlusion during sleep [7]. Functional appliances are routinely used for correction of retrognathic mandible in growing individuals [8]. Airway improvement after mandibular advancement by Twin Block appliance may result in a reduced risk of developing long-term impaired respiratory function. Various studies have been performed to evaluate the effect of the activator, activator with high-pull headgear, cervical headgear, the Farmand appliance, modification of bionator, the Klammt appliance, the Herbst appliance, and RME (Rapid Maxillary Expansion) with Herbst appliance therapy on the pharyngeal airway in Class II patients [6,9-15]. CBCT imaging modality has also been used to assess pharyngeal airway [16]. However, to our knowledge there is no study in the literature mentioning the effect of the most commonly used functional appliance, that is, the Twin-Block appliance, in the improvement of pharyngeal airway dimensions among subjects with Class II malocclusion by MRI. The purpose of this study was to examine three-dimensional changes in pharyngeal airway by MRI after treatment with Twin-Block appliance.
Materials and Methods
A longitudinal clinical study was carried out on 12 patients (two females and ten males) in the age group of 12-14 years from February 2012 to March 2013. Sample size selected was 12 keeping power of study as 80% at 95% confidence interval. Study was approved by Ethical Committee of Maulana Azad Institute of Dental Sciences, New Delhi. Patients with Angle’s Class II Division 1 malocclusion with retrognathic mandible and horizontal or average growth pattern giving a positive clinical Visual Treatment Objective (VTO) were included in the study. Patients with history of respiratory disease or airway obstruction were excluded. After taking informed consent from all subjects following records were obtained; study models, clinical photographs, standardised lateral cephalograms and MRI of Head and Neck region. All the patients were given Twin-Block appliance for correction of Class II Division 1 malocclusion.
MRI Procedure
MRI of the pharyngeal airway was performed during wakefulness using Philips INTERA 1.5 T MRI scanner (Philips Electronics, Netherland). Standardised contiguous sagittal T1-weighted MR images acquired centred about the mid-sagittal plane through the long axis of the airway (50 slices, 3 mm thickness, 272 by 512 matrix, FOV = 240 mm, TR = 649 ms, TE = 15 ms). Axial sections of the pharyngeal airway (36 slices, 3 mm thickness, 224 by 512 matrix, FOV = 240 mm, TR = 649 ms, TE = 15 ms) were acquired to calculate area of each slice from above the level of nasopharynx to below the level of hypopharynx [17].
All records were collected at two stages: Stage I (T1), pre-treatment and Stage II (T2) after completion of active phase i.e., 6-9 months (mean duration of treatment = 8.3 months).
MRI Measurements
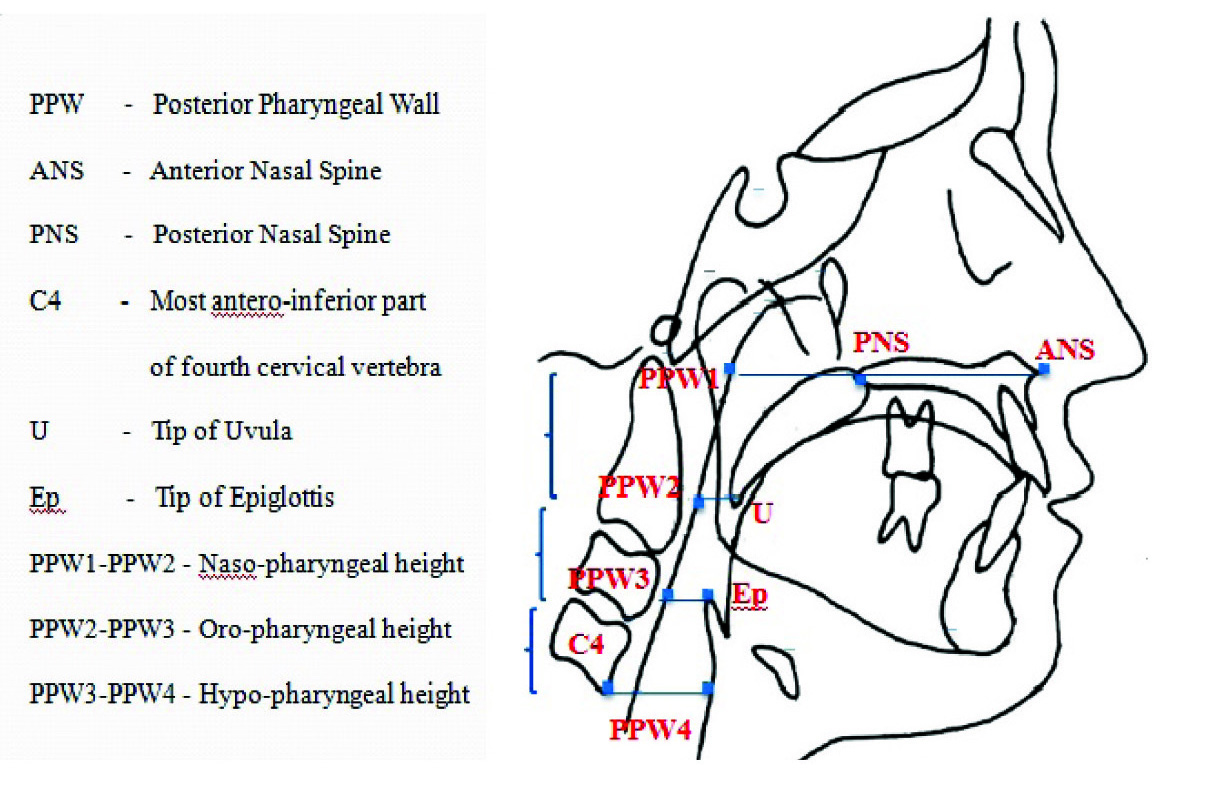
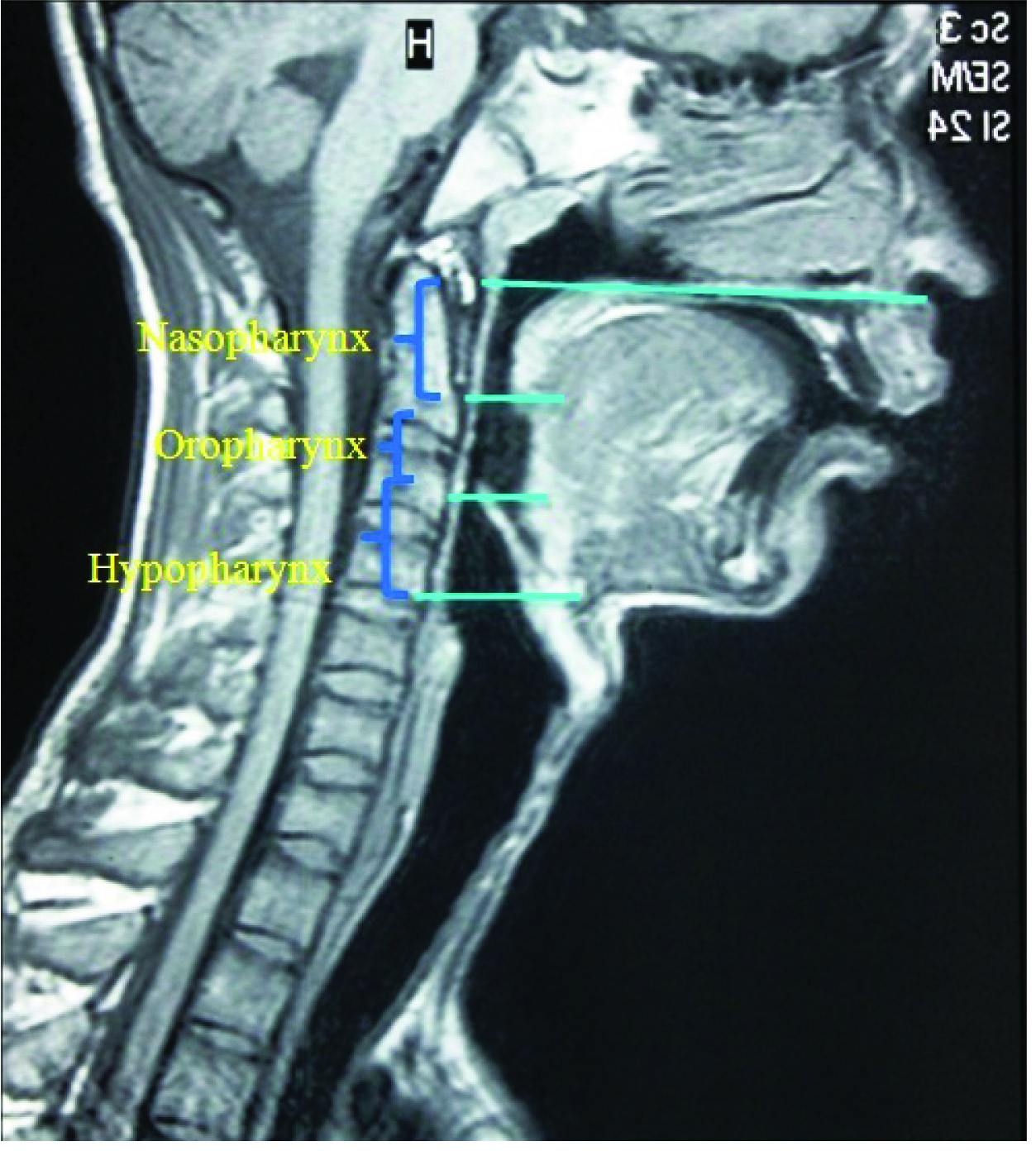
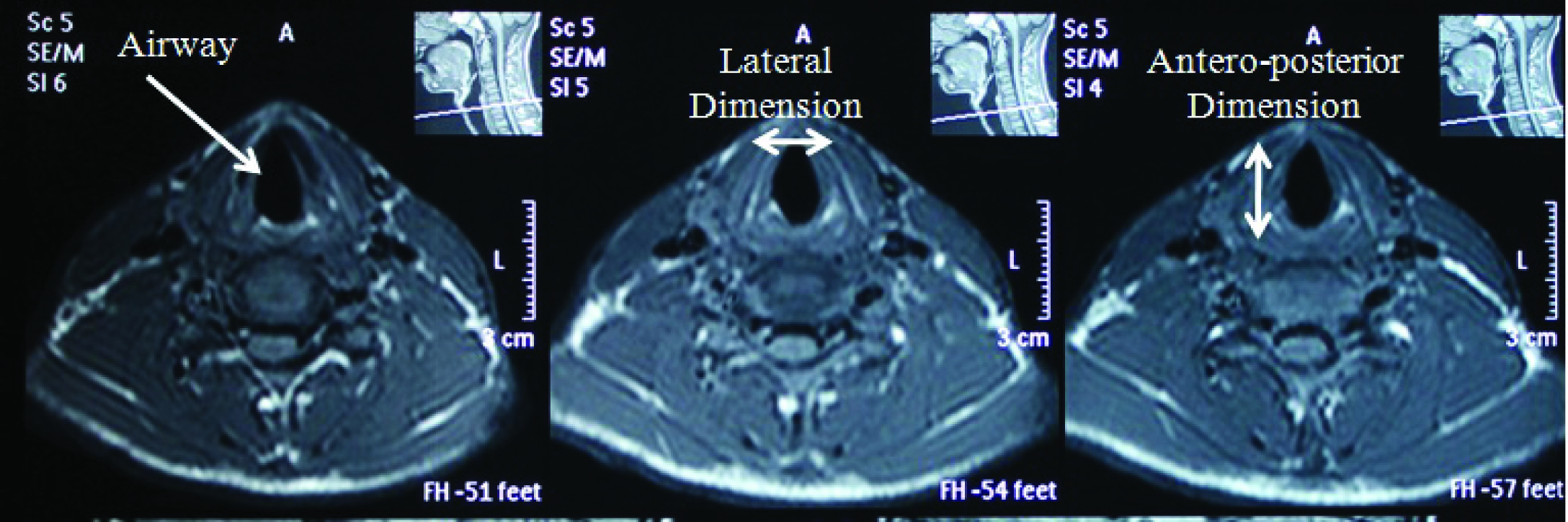
The upper airway was divided into three segments [Table/Fig-1,2] naso-pharynx (from the anterior nasal spine to the tip of the uvula), oro-pharynx (from the tip of the uvula to the tip of the epiglottis) and hypo-pharynx (from the tip of the epiglottis to the level of base of fourth cervical vertebra) [17]. Airway length was defined by the sum of the thickness of the axial images for the naso-pharyngeal, oro-pharyngeal and hypopharyngeal segments. Outline of airway was traced on axial sections [Table/Fig-3] and computer automatically gave area of outlined region. For calculating volume, area was multiplied with slice thickness of each axial section (3mm). All axial sections were traced starting from naso-pharynx to oro-pharynx. For evaluating antero-posterior changes, maximum linear distance was traced in naso-pharynx, oro-pharynx and hypo-pharynx parallel to Anterior Nasal Spine (ANS)- Posterior Nasal Spine (PNS) plane.
Landmarks and reference planes
MRI measurements on sagittal section.
MRI measurements on axial section.
Statistical Analysis
Data was entered into excel sheet and analysed by SPSS software version 17.0. Data was represented by mean and standard deviation. Change due to the treatment was expressed by mean and 95% confidence interval. Normality of the data was checked by Kolmogorov Smirnov test. The difference between the two means was observed by paired t-test, statistical significance was accepted if the p-value was <0.05.
Results
The present study was conducted on 12 growing patients (two females and ten males) in the age group of 12-14 years, with sagittal skeletal Class II relationship involving retrognathic mandible. All patients were treated by Twin-block appliance for correction of mandibular retrognathia. PAS changes were assessed by head and neck MRI.
At T2, a statistically significant increase in all three-dimensionsof PAS was observed in naso-pharynx, oro-pharynx and hypo-pharynx [Table/Fig-4,5]. After Twin-block treatment, maximum volumetric increase was seen in oro-pharynx with mean difference and standard deviation of 240±92.75mm3 (p<0.05) respectively. Oro-pharyngeal increase was followed by hypo-pharyngeal volume with mean and standard deviation of 207±139.62 mm3 (p<0.001) and naso-pharyngeal volume with mean and standard deviation of 111.51±137.03 mm3 (p<0.05). Maximum sagittal increase of 1.92±0.89 mm was seen in oro-pharynx (p<0.001) followed by hypo-pharynx (1.02±0.53 mm, p<0.001) and naso-pharynx (0.73±0.56 mm, p<0.001). Laterally, maximum increase was seen in oro-pharynx (1.61±0.55 mm, p<0.001) followed by hypo-pharynx (1.41±1.31 mm, p<0.001) and naso-pharynx (1.04±0.60 mm, p<0.001). There was significant increase in the vertical length of airway (PPW1-PPW2, PPW2-PPW3, PPW3-PPW4). Maximum increase in vertical length was seen in hypo-pharynx (1.421 mm, p<0.05) followed by oro-pharynx (1.392, p<0.01) and naso-pharynx (0.917, p<0.001). Total increase of 3.73 mm (PPW1 to PPW4) was observed in vertical dimension.
Pre-treatment and post-treatment three-dimensional MRI measurements (mean, standard deviation, n=12).
| Parameter | T1 | T2 |
|---|
| Mean±SD | Mean±SD |
|---|
| Naso-pharynx1. Area(mm2)2. Volume(mm3)3. A-P dimension(mm)4. Lat Dimension(mm)5. PPW1-PPW2(mm) (Vertical) | 868.7±248.052590±722.87.57±1.4815.92±3.3121.36±3.62 | 900.70±237.262701.5±712.928.31±1.5516.95±3.6022.28±3.35 |
| Oro-pharynx6. Area(mm2)7. Volume(mm3)8. A-P dimension(mm)9. Lat Dimension(mm)10. PPW2-PPW3(mm) (Vertical) | 880.47±290.982641.2±873.078.48±1.9115.35±3.4823.28±5.19 | 974.09±308.832882.1±938.1410.41±2.1216.96±3.8624.67±5.38 |
| Hypo-pharynx11. Area(mm2)12. Volume(mm3)13.A-P dimension(mm)14. Lat Dimension(mm)15. PPW3-PPW4(mm) (Vertical) | 1875.7±450.345627.2±1351.0210.72±2.1728.10±3.3322.38±4.23 | 1944.8±479.165834.3±1437.4911.74±2.3429.51±3.4523.79±4.19 |
Three dimensional treatment changes of pharyngeal airway as observed in MRI
| Parameter | Treatment changes |
|---|
| Mean(±SD) | p-value |
|---|
| Naso-pharynx1. Area(mm2)2. Volume(mm3)3. A-P dimension(mm)4. Lat Dimension(mm)5. PPW1-PPW2(mm) (Vertical) | 31.96111.51±137.030.73±0.561.04±0.600.917 | 0.021*0.017*0.001**<0.001 ***<0.001 *** |
| Oro-pharynx6. Area(mm2)7. Volume(mm3)8. A-P dimension(mm)9. Lat Dimension(mm)10. PPW2-PPW3(mm) (Vertical) | 93.62±12.97240.95±92.751.92±0.891.61±.551.392 | <0.001***<0.001***<0.001***<0.001***0.008** |
| Hypo-pharynx11. Area(mm2)12. Volume(mm3)13. A-P dimension(mm)14. Lat Dimension(mm)15. PPW3-PPW4(mm) (Vertical) | 69.03±46.5207.09±139.621.02±0.531.41±1.311.421 | <0.001***<0.001***<0.001***0.003**0.023* |
The difference between the two means was observed by paired –t test.
*p<0.05 (significant), ** p<0.01 (highly significant), *** p<0.001 (highly significant)
Discussion
Craniofacial form, skeletal maturity and age affects the dimensions of pharyngeal airway. Children with mandibular retrognathia and increased sagittal jaw relationship are particularly at risk of having small pharyngeal airway dimensions [18]. Although, lateral cephalogram is routinely used for diagnosis by orthodontists, changes in the lateral dimension and volume of PAS cannot be assessed by routinely used cephalograms.
Three-dimensional imaging is the appropriate method for the evaluation of PAS dimension. Although, computed tomography [16] studies have been done to assess the effect of mandibular advancement devices on airway, MRI is used in present study for evaluation of PAS. MRI is a non-ionising imaging tool which is probably the best method for soft tissue imaging. [17]. MRI is superior to CBCT as it doesn’t expose patients to ionising radiations and offers superior contrast for definitively characterising soft tissue structures [19]. Therefore, this study aimed to evaluate changes in PAS after Twin Block treatment in Class II Division 1 patients using MRI. In the present study, after Twin Block treatment, a statistically significant increase was seen in all portions of airway that were measured. One important and novel finding of our study was that mandibular advancement improved the patency of PAS, but this occured predominantly due to an increase in the volume of oro-pharynx and is mediated by an increase in all three dimensions of oro-pharynx. Maximum increase was found in oro-pharynx (240.95±92.75) followed by hypo-pharynx (207.09±139.62) and naso-pharynx (111.51±137.03). A major increase in the volume of oro-pharynx as compared to naso-pharynx and hypo-pharynx can be attributed to the forward posture of the tongue and is probably produced by anterior positioning of the mandible during the treatment.
In the present study, lateral and sagittal widening of PAS are observed. Maximum changes in lateral and sagittal dimension were seen in oro-pharynx as compared to naso-pharynx and hypo-pharynx. According to Zhao X et al., and Kyung SH et al., airway increase is gained at the expense of an increase in transverse diameter [20,21]. Gale DJ et al., noticed an increase in the pharyngeal area using a mandibular advancement device but with substantial individual variability [22].
Lateral increase in PAS can be attributed to the maxillary expansion performed in upper appliance of Twin-block, soft tissue connections between the mandible, tongue, lateral pharyngeal walls and the soft palate which are stretched by mandibular advancement [23] resulting in lateral widening.
In vertical dimension, maximum increase was observed in hypo-pharynx followed by oro-pharynx and naso-pharynx. Total increase of 3.73 mm was found in the vertical dimension of airway. Vertical increase can be attributed to increase in lower anterior facial height due to mandibular repositioning concomitant with growth.
Thus, the present study confirmed that there is a positive effect of functional appliance therapy on the PAS dimension. The positive impact of myofunctional appliance treatment on the airway dimension cannot be justified only by the skeletal changes achieved. Functional appliance treatment causes many bony and soft tissue changes like, forward position of tongue, increase in lower anterior facial height, raised position of hyoid and lateral displacement of parapharyngeal fat pads away from the airway along with the difference in tongue posture.
In the present study, increase in all dimensions of PAS was observed. Similarly, Schutz TCB et al., also noticed an increase in the volume of hypo-pharynx following Class II correction by Herbst appliance, and attributed this improvement to forward mandibular repositioning [15]. Kinzinger G et al., noticed that Class II malocclusion correction by functional mandibular advancement was not effective in preventing breathing problems in patients who were at risk [14]. It is known that Class II dentoskeletal disharmony does not exhibit a tendency for self correction along with growth. Functional appliance therapy eliminates the hindrance for normal growth of mandible and airway passage. Another justification for the improvement could be ‘‘catch-up growth,’ whereby children with small oropharyngeal dimensions would have a greater intrinsic stimulus to increase their capacity for respiratory function [9]. The literature [9,24] supports the fact that the improvement in the pharyngeal airway following functional appliance therapy are maintained in the long-term.
It is also noteworthy that individual differences in normal growth and in the response of treatment are considerable. Even a small diameter change in dimension of PAS can result in a substantial volumetric change and can have a great effect on airflow because the resistance decreases four times as the radius increases.
When narrow pharyngeal airway is suspected clinically, MRI should be considered for three-dimensional assessment as it gives best soft tissue contrast.
Limitation
Limitation of present study is the lack of control group due to ethical issues, relatively high cost, as well as the limited availability of MRI technique. Long-term study is required to assess the stability of increased pharyngeal airway volume.
Conclusion
Following Twin-Block treatment, MRI assessment revealed a significant increase in the PAS in all three dimensions. Significant increase in all three dimensions of PAS was observed following Twin Block treatment in Class II Division 1 subjects.
Maximum volumetric increase was seen in oro-pharynx, followed by hypo-pharynx and naso-pharynx. MRI is an accurate, three-dimensional, non-invasive and superior diagnostic tool for soft tissues and should be considered specially when mandibular morphology may affect PAS viz., obstructive sleep apnea, craniofacial abnormalities like Pierre Robin Syndrome, micrognathia and long face syndrome associated with hypertrophied tonsils etc.
The difference between the two means was observed by paired –t test.
*p<0.05 (significant), ** p<0.01 (highly significant), *** p<0.001 (highly significant)