Introduction
Sacroiliac Joint (SIJ) is a familiar nociceptive source of Low Back Pain (LBP). Patients with SIJ pain commonly present with tenderness around the Posterior Superior Iliac Spine (PSIS) which can be recorded by using pressure pain algometer. Mechanical Diagnosis and Therapy (MDT) is a manual therapy technique which uses repetitive movements to assess and treat the dysfunction. MDT is found to be effective in treating SIJ pain; however, its effect on Pain Pressure Threshold (PPT) is not yet determined.
Aim
To determine the effect of Mechanical Diagnosis and Therapy on Pain Pressure Threshold in Sacroiliac Joint pain.
Materials and Methods
A total of 25 subjects with unilateral LBP of age group 20-65 years participated in the study. Subjects with the direction of preference, pain around the PSIS, positive on two out of four pain provocation tests were included in the study. These patients were given 30 repetitions of either anterior or posterior rotation of the innominate, for four sessions. PPT and Visual Analogue Scale (VAS) were used to measure the effect of treatment. Data were analysed by using paired t-test.
Results
There was a significant improvement seen (p<0.01) in PPT and VAS after four consecutive sessions of treatment.
Conclusion
A significant statistical difference was seen in PPT and VAS with p-value <0.01 at the end of four sessions of MDT treatment. The study suggests that MDT can be used effectively in managing SIJ tenderness around the PSIS and pain. However, future studies should focus on comparing MDT with a control group or with other manual therapy techniques.
Introduction
Sacroiliac joint is common but often a misdiagnosed cause of LBP [1]. Approximately 13% of patients with persistent LBP have the origin of pain from SIJ and impacts 16-17% of Indian patients with LBP [2,3].
Sacroiliac joint pain attributes to the pain arising from SIJ structures [2,4,5]. The pain is associated with factors such as joint laxity, degeneration, trauma, positional faults, mal-alignment, muscle imbalances, derangement and hypomobility at SIJ [6,11].
Patients often complain of pain in the groin, buttock and lower extremities [12-14]. Frequently, patients point out pain and tenderness with one finger (Fortin finger test) in the region inferior to the PSIS as a common symptom [12-17].
Conventionally physiotherapists use treatment which consists of electrotherapy, exercise therapy and manual therapy. Manual therapy includes manipulation, Maitland’s and Mulligan’s mobilisation and muscle energy technique in treating SIJ pain [4].
The MDT is a well-known exercise and manual therapy technique developed by Robin McKenzie. It is an active therapy that empowers the patients by self-management skills and can give a sense of confidence and independence to them [18]. This technique uses repeated movements to assess and treat musculoskeletal disorders of the spine and the extremities. Based on the results of repeated movements, the patient’s condition is classified into derangement, dysfunction and postural syndrome or other categories [11,19-22].
During the repeated movement examination, patients with derangement syndrome will have a direction of preference i.e., a certain movement may either augment or alleviate pain. The movement which alleviates or abolishes pain becomes the treatment of choice untill the derangement or symptoms are reduced. A repeated anterior or posterior rotation of the innominate is performed to classify patients with SIJ pain into derangement syndrome [11]. MDT has been employed in treating derangement syndromes under various regions such as cervical, lumbar, shoulder, temporomandibular joint and SIJ by using the principle of repeated movements [11,19-24].
It has been speculated by a few researchers that the subjects with conjectured SIJ pain point out the most intensely painful area adjacent to the PSIS [14-16]. A recently formulated clinical diagnostic rule for a study which drew recommendations from systematic reviews endorsed the use of examination of dominant pain in the PSIS region for SIJ pain [17]. The authors even found it reasonable to consider pain in the PSIS region as one of the most important clinical signs which can lead to the clinical diagnosis of SIJ pain [14-17,25]. Hence, it is crucial to analyse the effect of MDT on pain around the PSIS.
Physical examination of tenderness and location of pain at PSIS using a pressure test is still ambiguous in interpretation, the reason being the failure to standardise the pressure exerted by the finger [15,26]. PPT is defined as the point at which a non-noxious pressure stimulus changes into a nociceptive pressure sensation. The Pressure algometer is usually used as an outcome measuring tool, which objectively quantifies PPT or pressure pain sensitivity [26]. Usability of pressure algometry is unarguably reliable in assessing tenderness at PSIS, with ICC varying between 0.60 and 0.82 that is moderate to good [15]. SIJ pain is confirmed by using a composite of four pain provocation tests which is claimed to produce good results. Two positive tests out of four (distraction, compression, thigh thrust, and sacral thrust tests) have a likelihood ratio of 4, 0.88 sensitivity and 0.78 specificity [5].
MDT has beneficial effects in reducing pain in SIJ, same has been found by investigators in the previous study [11] however; its effect on PPT in the SIJ has not been validated. Hence, the present study intends to determine the effect of MDT on PPT in patients with SIJ pain.
Materials and Methods
This is a single group pre-post test intervention study, which was carried out during the period between January 2016 to December 2016, in the Department of Physiotherapy, KS Hegde Medical Academy, Mangalore a Tertiary Care Hospital in Karnataka, India. Ethical Clearance of the study was obtained from the Institutional Ethical Committee of the Department of Physiotherapy, NITTE University. The current study is a part of an ongoing larger RCT, using power 80%, this sample size was determined.
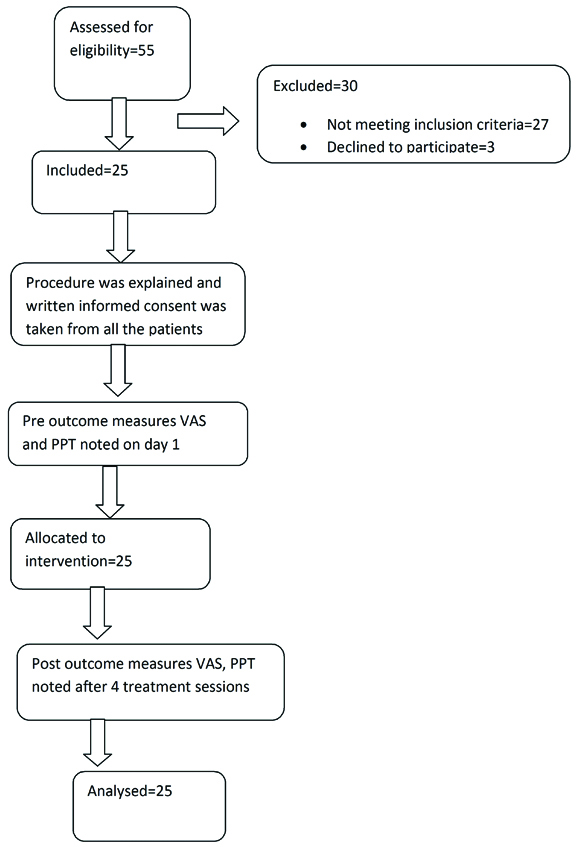
A total of 55 subjects with unilateral LBP in the age group between 20-65 years were screened clinically by the physician for the presence of SIJ pain. These diagnosed SIJ subjects were then referred to the physiotherapy outpatient department. Subjects were included if they had direction of preference, sub-acute or chronic symptoms, pain below L5 level, pain around PSIS, two out of four pain provocation tests i.e., ‘distraction, compression, thigh thrust, and sacral thrust tests’ positive. Subjects were excluded if on screening they had midline back pain, lumbar disc related pain, above L5 spinal level pain, radicular pain with neurological deficits. The screening was done by using McKenzie assessment for the lumbar spine [27]. Subjects were also excluded if they had reported spondylolisthesis, bilateral back pain, true limb length discrepancy, scoliosis, reported hip or lower limb pathology or fracture, any back, hip or knee surgery, SIJ pain in pregnant females, a systemic illness like ankylosis spondylitis, rheumatoid arthritis, arthropathies, hospitalisation due to severe trauma. All the subjects agreed not to undergo any other form of treatment apart from the exercise program provided in the study for four days, albeit, no attempts were made to refrain them from taking medications. A written informed consent was obtained from all the subjects prior to the study. Schematic diagram showing the enrolment of the patients and the study procedure is displayed in [Table/Fig-1].
Schematic diagram showing the enrolment of the patients and the study procedure.
Measurements
After the preliminary examination, the outcome measures were assessed on the first day prior to the commencement of the treatment and after the fourth day of intervention by the assessor who was a physiotherapist with six years of clinical experience and was blind to the intervention.
Outcome measure included PPT, recorded by digital algometer. The subjects were made to lie in the prone position with the probe of algometer placed 1 cm inferior to the PSIS, and an axial force was applied [15]. The participants were asked to report the very first pain perceived on the application of force. The readings were taken in a gap of one-minute interval for three times and the mean was considered as the final score. The force measurements were recorded in Newton. The pain perception was assessed using VAS which is a 10 cm straight line with markings from 0-10, where 0 signifies no pain and 10 denotes the worst pain. The patients were asked to mark a point on this line to indicate their current pain severity. The outcome measures were taken at the end of the four sessions of the intervention [28-30].
Intervention
A repeated movement examination using MDT principles was done to identify the direction of preference. Ten repetitions of anterior or posterior rotation of the innominate were performed to abolish or magnify symptoms. Once the direction of preference or the behaviour of symptoms was identified, the same movement was given as a treatment. Three sets of ten repetitions with a period of one-minute rest between each set were given for four days. All the patients were also advised to repeat 30 repetitions after every 2-3 hour. The treatment was provided by a manual therapist with six years of clinical experience and certification in the Level A course (lumbar spine), certified by the McKenzie Institute of India.
Procedure
Repeated anterior rotation of the innominate: In a half kneeling or a lunge position, a repeated end range anterior rotation of the innominate was encouraged [Table/Fig-2a,b] [31].
Starting position for anterior rotation of the innominate.

Final position for anterior rotation of the innominate.

Repeated posterior rotation of innominate: in supine position repeated posterior rotation of the innominate was encouraged by getting the hip and knee into flexion towards the chest [Table/Fig-3].
Demonstration of posterior rotation of the innominate.

Statistical Analysis
Statistical analysis was done using Statistical Package for Social Science (SPSS) version 16.0. At a 95% confidence interval p-value <0.01 was considered to be statistically significant. The data analysis was done using a paired t-test to compare pre and post scores.
Results
A total of 25 patients with SIJ pain (22 subacute; 3 chronic) were included in the present study. The study enrolled 13 females and 12 males with mean age of 39.92±13.56 and 40.58±11 years respectively. There were no dropouts. A decrease in the scores of PPT and pain after the four intervention sessions were observed, as shown in [Table/Fig-4]. The improvement in the scores of PPT and VAS was statistically significant (p<0.01).
Intra group comparison of outcome measures using paired t-test.
| Outcome Measure | Pre | Post | Mean difference | p-value |
|---|
| Pain pressure threshold | 29.40±11.75 | 40.25±11.70 | 10.85 | <0.01 |
| Visual analogue scale | 6.84 (±1.84) | 3.56 (±2.03) | 3.28 | <0.01 |
Discussion
The SIJ is often neglected but also considered as a significant cause of LBP [12,32]. The current study was focused on the management of SIJ pain using principles of MDT. The McKenzie method or popularly referred to as MDT requires the active involvement of the subject by producing self-generated loading strategies both in the assessment and treatment [11]. The MDT technique uses repeated movements to obtain mechanical responses and classifies into three syndromes i.e., postural, dysfunction and derangement or others [11,19-21]. A derangement syndrome is customary when there is a rapid change in the baseline symptoms during the movement examination.
In the present study, the subjects were classified into derangement syndrome as they demonstrated improvement of symptoms after performing either repeated anterior and posterior rotation of the innominate. Authors observed a statistically significant difference in PPT and pain intensity. Findings of the present study are in concurrence with the previous research which used MDT principles in treating chronic neck pain [22]. The study reported improvement in PPT with the mean difference of 2.52±1.87 in PPT and 1.37±0.92 in VAS [23]. For consistency, the treatment was limited to four supervised sessions over 4 consecutive days. Additionally, the literature lacks the standard and optimal parameters for delivering MDT exercises [33,34]. Previous studies have also imposed the same dosage and have achieved effective results. Garcia A et al., found McKenzie exercises superior to the back school and identified similar improvement concerning pain and disability (mean difference: 2.4 and 5.2 respectively) after four treatment sessions in non-specific LBP [28]. Long A et al., also observed alleviated pain and improved function in LBP after four visits [30]. The results of the present study are in uniformity with the aforementioned studies. Most of the subjects in the present study had symptoms ranging from seven days to seven weeks (subacute), except three patients who had symptoms of more than 7 week duration (chronic) [35]. It has been speculated that MDT exercises works well on subacute LBP symptoms than chronic symptoms [36]. Similar to present observation, Schenk RJ et al., also demonstrated a significant improvement in pain and disability in subacute LBP patients after only three sessions of MDT [35]. Also, in this sense, Machado LA et al., found MDT along with first-line care had noticeable improvement in pain when compared to first-line care only in patients with acute back pain [37]. There are several studies supporting the use and efficacy of MDT. A previous study compared McKenzie with Mulligan’s SNAG technique and found the former was more useful in reducing pain and disability in chronic LBP [38]. Though, some authors have suggested that MDT and Orthopaedics Manual Therapy (OMT) methods were slightly more effective than just advice in LBP patients [23]. A randomised controlled trial observed that MDT was mildly effective for pain, however, not effective for disability when compared to placebo in nonspecific chronic LBP [39]. Nonetheless, present results are in accordance with a recent Meta-analysis which concluded that MDT has statistically and clinically great significant role in reducing pain intensity in acute and subacute LBP when compared to manual therapy along with the exercises. The study further stated that MDT is more effective in reducing pain and disability than other rehabilitation techniques in chronic LBP [40]. A case report on SIJ pain found similar results as the present study. They hypothesised that the loose bodies in the joint articulation cause painful locking or dysfunction in the movement. The debris can get entrapped, and therefore it responds to repeated movements which may reduce the displacement and thereby improve symptoms [11]. This could be one of the possible reasons for the significant results in the present study. However, from a theoretical perspective, a variety of structures could have been the source of the subjects’ symptoms in the present study. These include, but are not limited to, the deranged: articular cartilage, sacroiliac ligament, the aberrant position of the iliac bone due to tight hamstrings, gluteus maximus/iliopsoas, joint locking and hypomobility of the SIJ [9,41-43]. The SIJ can be put under strain by tightened muscles attached in proximity to the joint causing rotation of the innominate [42,43]. An inflexible muscle can also lock the joint in an abnormal position [9]. In an RCT which compared the effectiveness of Mulligan’s Bend leg raise technique with McKenzie’s knee to chest movement repetitions on hamstring tightness, found an immediate increase in length in both the group [44].
Authors in the present study speculate a resolution of tight hamstrings, gluteus maximus/iliopsoas in the subjects which could have led to the correction of positional dysfunction or unlocking of the joint after performing repeated end range loading strategies. Hypomobility is also a known factor of SIJ pain [9]. Authors also contemplate that by encouraging repeated anterior or posterior rotation of the innominate, the hypomobility could have been reversed thereby producing rapid and significant improvement in the symptoms. MDT is a reliable and valid approach for evaluation of both the spine and extremities [19-23,27]. MDT, when compared to other conservative treatment strategies, is an effective treatment choice [40].
Limitation
Several limitations were encountered in the present study which needs to be addressed in future studies. Due to small sample size, the results cannot be generalised to the population. Future studies would have more compelling evidence if it included a control group. Future clinical trials comparing MDT with other manual therapy techniques are also needed. The present study determined the short-term effect of MDT; its long-term effect is not yet established.
Conclusion
Mechanical Diagnosis and Therapy is an active treatment technique which can render self-reliant techniques to the patients for their pain management and thus empowering them with confidence. In the present study, a four-day treatment regime is accomplished by improving PPT and pain. Hence, MDT can be beneficial in managing pain and pressure pain sensitivity in patients with SIJ pain.
[1]. Cibulka MT, Koldehoff R, Clinical usefulness of a cluster of sacroiliac joint tests in patients with and without low back painJ Orthop Sports Phys Ther 1999 29(2):83-92.10.2519/jospt.1999.29.2.8310322583 [Google Scholar] [CrossRef] [PubMed]
[2]. Laslett M, Evidence based diagnosis and treatment of painful sacroiliac jointJ Man Manip Ther 2008 16(3):142-52.10.1179/jmt.2008.16.3.14219119403 [Google Scholar] [CrossRef] [PubMed]
[3]. Saumya S, Anurag S, Dhanesh K KU, Harramb M, Prevalence of sacroiliac joint dysfunction among Indian Low Back Pain PatientsIndian Journal of Physiotherapy and Occupational therapy 2018 12(2):20-23.10.5958/0973-5674.2018.00031.X [Google Scholar] [CrossRef]
[4]. Neha B, Arunmozhi R, Maneesh A, Pooja A, Effectiveness of therapeutic interventions in sacroiliac joint dysfunction: a systematic reviewInt J Physiother Res 2016 4(3):1484-88.10.16965/ijpr.2016.111 [Google Scholar] [CrossRef]
[5]. Laslett M, Aprill CN, McDonald B, Young SB, Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of testsMan Ther 2005 10(3):207-18.10.1016/j.math.2005.01.00316038856 [Google Scholar] [CrossRef] [PubMed]
[6]. Zelle BA, Gruen GS, Brown S, George S, Sacroiliac joint dysfunction evaluation and managementClin J Pain 2005 21(5):446-45.10.1097/01.ajp.0000131413.07468.8e16093751 [Google Scholar] [CrossRef] [PubMed]
[7]. O’Sullivan PB, Beales DJ, Diagnosis and classification of pelvic girdle pain disorders-Part 1: a mechanism based approach, within a biopsychosochial frameworkMan Ther 2007 12(2):86-97.10.1016/j.math.2007.02.00117449432 [Google Scholar] [CrossRef] [PubMed]
[8]. Riddle DL, Freburger JK, Evaluation of the presence of sacroiliac joint region dysfunction using a combination of tests: a multicenter intertester reliability studyPhys Ther 2002 82(8):772-81. [Google Scholar]
[9]. Clavel AL, Sacroiliac joint dysfunction: from a simple pain in the butt to integrated care for complex low back painTechniques in Regional Anesthesia and Pain Management 2011 15:40-50.10.1053/j.trap.2011.06.002 [Google Scholar] [CrossRef]
[10]. Shearar KA, Colloca CJ, White HL, A randomized clinical trial of manual versus mechanical force manipulation in the treatment of sacroiliac joint syndromeJ Manipulative Physiol Ther 2005 28(7):493-501.10.1016/j.jmpt.2005.07.00616182023 [Google Scholar] [CrossRef] [PubMed]
[11]. Horton SJ, Franz A, Mechanical diagnosis and therapy approach to assessment and treatment of derangement of the sacroiliac jointMan Ther 2007 12(2):126-32.10.1016/j.math.2006.06.00116891145 [Google Scholar] [CrossRef] [PubMed]
[12]. Slipman CW, Jackson HB, Lipetz JS, Chan KT, Lenrow D, Vresilovic EJ, Sacroiliac joint pain referral zonesArch Phys Med Rehabil 2000 81(3):334-38.10.1016/S0003-9993(00)90080-7 [Google Scholar] [CrossRef]
[13]. Donatelli RA, Wooden MJ, Orthopaedic Physical Therapy 2001 3rd edChurchill LivingstoneElsevier:393 [Google Scholar]
[14]. van Leeuwen RJ, Szadek K, de Vet H, Zuurmond W, Perez R, Pain pressure threshold in the region of the sacroiliac joint in patients diagnosed with sacroiliac joint painPain Physician 2016 19(3):147-54. [Google Scholar]
[15]. Fortin JD, Falco FJ, The Fortin finger test: an indicator of sacroiliac painAm J Orthop (Belle Mead NJ) 1997 26(7):477-80. [Google Scholar]
[16]. Forst SL, Wheeler MT, Fortin JD, Vilensky JA, The sacroiliac joint: anatomy, physiology and clinical significancePain Physician 2006 9(1):61-67. [Google Scholar]
[17]. Petersen T, Laslett M, Juhl C, Clinical classification in low back pain: best-evidence diagnostic rules based on systematic reviewsBMC Musculoskelet Disord 2017 18(1):18810.1186/s12891-017-1549-628499364 [Google Scholar] [CrossRef] [PubMed]
[18]. Takasaki H, Mechanical diagnosis and therapy enhances attitude toward self-management in people with musculoskeletal disorders: a preliminary evidence with a before–after designSAGE Open Med 2017 5:01-09.10.1177/205031211774098629163947 [Google Scholar] [CrossRef] [PubMed]
[19]. Krog C, May S, Derangement of the temporomandibular joint; a case study using Mechanical Diagnosis and TherapyMan Ther 2012 17(5):483-86.10.1016/j.math.2011.12.00222177711 [Google Scholar] [CrossRef] [PubMed]
[20]. Aina A, May S, A shoulder derangementMan Ther 2005 10(2):159-63.10.1016/j.math.2005.01.00115922237 [Google Scholar] [CrossRef] [PubMed]
[21]. Kidd J, Treatment of shoulder pain utilizing mechanical diagnosis and therapy principlesJ Man Manip Ther 2013 21(3):168-73.10.1179/2042618613Y.000000003724421628 [Google Scholar] [CrossRef] [PubMed]
[22]. Seo SC, Choi JY, Joo MY, Kim JH, Chang SK, Effects of sling exercise and Mckenzie exercise program on neck disability, pain, muscle strength and range of motion in chronic neck painPhysical Therapy Rehabilitation 2012 1(1):40-48. [Google Scholar]
[23]. Paatelma M, Kilpikoski S, Simonen R, Heinonen A, Alen M, Videman T, Orthopaedic manual therapy, McKenzie method or advice only for low back pain in working adults: a randomized controlled trial with one year follow-upJ Rehabil Med 2008 40(10):858-63.10.2340/16501977-026219242624 [Google Scholar] [CrossRef] [PubMed]
[24]. Johnson OE, Adegoke BO, Ogunlade SO, Comparison of four physiotherapy regimens in the treatment of long-term mechanical low back painJ Jpn Phys Ther Assoc 2010 13(1):09-16.10.1298/jjpta.13.925792891 [Google Scholar] [CrossRef] [PubMed]
[25]. McGrath M, Composite sacroiliac joint pain provocation tests: A question of clinical significanceInternational Journal of Osteopathic Medicine 2010 13(1):24-30.10.1016/j.ijosm.2009.06.002 [Google Scholar] [CrossRef]
[26]. Pelfort X, Torres-Claramunt R, Sánchez-Soler J, Hinarejos P, Leal-Blanquet J, Valverde D, Pressure algometry is a useful tool to quantify pain in the medial part of the knee: An intra- and inter-reliability study in healthy subjectsOrthop Traumatol Surg Res 2015 101(5):559-63.10.1016/j.otsr.2015.03.01626025162 [Google Scholar] [CrossRef] [PubMed]
[27]. Clare H, Adams R, Maher C, Construct validity of lumbar extension measures in McKenzie’s derangement syndromeMan Ther 2007 12(4):328-34.10.1016/j.math.2006.07.00616971163 [Google Scholar] [CrossRef] [PubMed]
[28]. Garcia A, Gondo F, Costa R, Cyrillo F, Costa L, Effects of two physical therapy interventions in patients with chronic non-specific low back pain: feasibility of a randomized controlled trialRev Bras Fisioter 2011 15(5):420-27.10.1590/S1413-3555201100500001922002187 [Google Scholar] [CrossRef] [PubMed]
[29]. Garcia A, Costa L, Hancock M, Costa L, Identifying patients with chronic low back pain who respond best to mechanical diagnosis and therapy: secondary analysis of a randomized controlled trialPhys Ther 2015 96(5):623-30.10.2522/ptj.2015029526494768 [Google Scholar] [CrossRef] [PubMed]
[30]. Long A, Donelson R, Fung T, Does it matter which exercise? A randomized control trial of exercise for low back painSpine 2004 29(23):2593-602.10.1097/01.brs.0000146464.23007.2a15564907 [Google Scholar] [CrossRef] [PubMed]
[31]. Mckenzie R, May S, The lumbar spine Mechanical diagnosis and therapy 2003 2nd edSpinal PublicationChapter 13 pp. 248 [Google Scholar]
[32]. Cohen S, Chen Y, Neufeld N, Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatmentExpert Rev Neurother 2013 13(1):99-116.10.1586/ern.12.14823253394 [Google Scholar] [CrossRef] [PubMed]
[33]. Garcia A, Costa L, da Silva T, Gondo F, Cyrillo F, Costa R, Effectiveness of back school versus mckenzie exercises in patients with chronic nonspecific low back pain: a randomized controlled trialPhys Ther 2013 93(6):729-47.10.2522/ptj.2012041423431213 [Google Scholar] [CrossRef] [PubMed]
[34]. Dunsford A, Kumar S, Clarke S, Integrating evidence into practice: use of McKenzie-based treatment for mechanical low backpainJ Multidiscip Healthc 2011 4:393-402.10.2147/JMDH.S2473322135496 [Google Scholar] [CrossRef] [PubMed]
[35]. Schenk RJ, Jozefczyk C, Kopf A, A randomized trial comparing interventions in patients with lumbar posterior derangementJ Man Manip Ther 2003 11(2):95-102.10.1179/106698103790826455 [Google Scholar] [CrossRef]
[36]. Ibrahimaj A, Deliu S, Sylejman M, Effectiveness of the McKenzie method in the treatment of low back pain in subacute and chronic stageResearch in Physical Education, Sport & Health 2015 4(1):79-86. [Google Scholar]
[37]. Machado LA, Maher CG, Herbert RD, Clare H, McAuley JH, The effectiveness of the McKenzie method in addition to first-line care for acute low back pain: a randomized controlled trialBMC Med 2010 8:1010.1186/1741-7015-8-1020102596 [Google Scholar] [CrossRef] [PubMed]
[38]. Waqqar S, Shakil-Ur-Rehman S, Ahmad S, Mckenzie treatment versus mulligan sustained natural apohphyseal glides for chronic mechanical low back painPak J Med Sci 2016 32(2):476-79. [Google Scholar]
[39]. Garcia AN, Costa LDCM, Hancock MJ, Souza FS, Gomes GVFO, Almeida MO, McKenzie Method of Mechanical Diagnosis and Therapy was slightly more effective than placebo for pain, but not for disability, in patients with chronic non-specific low back pain: a randomised placebo controlled trial with short and longer term follow-upBr J Sports Med 2018 52(9):594-600.10.1136/bjsports-2016-09732728701365 [Google Scholar] [CrossRef] [PubMed]
[40]. Lam OT, Strenger DM, Chan-Fee M, Pham PT, Preuss RA, Robbins SM, Effectiveness of the McKenzie Method (Mechanical Diagnosis and Therapy) for treating low back pain: literature review with meta-analysisJ Orthop Sports Phys Ther 2018 48(6):476-90.10.2519/jospt.2018.756229602304 [Google Scholar] [CrossRef] [PubMed]
[41]. Cohen SP, Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatmentAnesth Analg 2005 101(5):1440-53.10.1213/01.ANE.0000180831.60169.EA16244008 [Google Scholar] [CrossRef] [PubMed]
[42]. Arab MA, Nourbakhsh RM, Mohammadifar A, The relationship between hamstring length and gluteal muscle strength in individuals with sacroiliac joint dysfunctionJ Man Manip Ther 2011 19(1):05-10.10.1179/106698110X1280499342684822294848 [Google Scholar] [CrossRef] [PubMed]
[43]. Schamberger W, The Malalignment Syndrome implications for medicine and sport 2002 New YorkChurchill Livingstone [Google Scholar]
[44]. Kulkarni PP, Devasthali A, Kumar A, Pimpale S, Comparison of effectiveness of bend leg raise technique of mulligan v/s knee to chest technique of Mckenzie to improve forward flexion range in subjects with hamstring tightness within the age group of 20-30 yearsInternational Journal of Recent Scientific Research 2016 7(9):13426-31. [Google Scholar]