Systemic lupus erythematosus related pancreatitis is an exclusive diagnosis that is made based on different clinical, biochemical and radiological findings. The incidence of SLE related pancreatitis is low and in the literature sufficient data is not available regarding management of such cases. The present three cases reported with symptoms and signs of acute pancreatitis, in which the diagnosis of SLE was done later and the acute pancreatitis was the presenting condition.
Case 1
A 19-year-old female presented to the Department of Medicine with a complaint of fever for one month and severe abdominal pain for 4-5 days. Patient had recurrent episodes of fever for the last six months and fever was subsiding on taking paracetamol. Patient had diffuse abdomen pain, more in the upper quadrant and it was insidious, progressive and non-radiating.
On physical examination, vitals were within normal limits. Hyper and hypopigmented patches were present all over back and neck and rashes on the face. Bilateral cervical lymphadenopathy was observed. The abdomen was soft, tender with guarding. The patient was not co-operative to rule out organomegaly. Other systemic examinations such as of the central nervous system, cardiovascular system, and respiratory system were found to be normal.
Laboratory investigations are shown in [Table/Fig-1]. She was evaluated for other causes of pain abdomen and pancreatitis. Endoscopy and lower gastrointestinal scopy were done. Antinuclear Antibody (ANA) global test showed nucleus homogenous pattern which was strong positive (+++) on HEP-2 cells. Antinuclear antibody profile was strong positive for nRNP/Sm (+++), dsDNA (+++) and anti-nucleosomes (+++). Antibodies to Cardiolipin (ACA–IgM) was positive with the titer 24 PLU/mL.
Laboratory investigations of all three cases with normal value.
| Investigation | Case 1 | Case 2 | Case 3 | Normal Range |
|---|
| Serum bilirubin total | 0.7 | 0.6 | 3.2 | 0.3 to 1.2 mg/dL |
| Serum bilirubin direct | 0.3 | 0.2 | 3.1 | <0.2 mg/dL |
| Serum bilirubin indirect | 0.4 | 0.4 | 0.1 | |
| Alkaline phosphatase (ALP) | 192 | 77 | 422 | 50-390 IU/L |
| Alanine aminotransferase (ALT) | 66 | 470 | 315 | 08-29 IU/L |
| Aspartate aminotransferase (AST) | 453 | 255 | 1324 | 15-45 IU/L |
| Serum albumin | 2.7 | 1.96 | 2.7 | 3.5-5 g/dL |
| IgG level | 4 | 2.40 | 3.70 | 2-3.5g/dL |
| Serum urea | 117 | 4 | 64 | 10-40 mg/dL |
| Serum creatinine | 1.9 | 0.3 | 1.6 | 0.5-1.2 mg/dL |
| Serum amylase | 977 | 174 | 864 | 28-100 U/L |
| Serum lipase | 3583 | 204 | 3699 | 8-80 U/L |
| Thyroid stimulating hormone | 5.48 | 1.46 | 5.120 | 0.3 to 4.5 μIU/mL |
| ESR | 66 | 39 | 5 | 0-20 |
| Platelet count | 67,000 | 3,37,000 | 67,000 | 1.5-4 lacs/μL |
| Viral hepatitis B | Negative | Negative | Negative | Negative |
| Viral hepatitis C | Negative | Negative | Negative | Negative |
| C reactive protein | 73.3 | 10.5 | Negative | 0-5 mg/L |
| C3 | 20 | 31 | 20 | 90-150 mg/dL |
| C4 | 5 | 1 | 1 | 15-50 mg/dL |
| Urine protein | 77 | 1495 | Negative | 24-180 mg/24hours |
| Procalcitonin | 0.9735 | Negative | 0.871 | <0.5 mcg/L |
| Antibodies to dsDNA | Positive (>800) | Negative | Positive (>800) | >100 IU/mL |
Ultrasonography of abdomen showed mesenteric lymphadenitis and bulky pancreas.
Multiple mesenteric lymph nodes within bilateral iliac fossa and paraumbilical regions, largest among the right iliac vessel and few of lymph nodes are clustered in the right lower quadrant with probe tenderness. Cervical lymph node biopsy was suggestive of Lupus lymphadenitis. Section showed partially effaced nodal architecture with hyperplastic lymphoid follicles in cortex and paracortex with confluent areas of necrosis, with dense karyorrhectic debris, numerous basophilic bodies, interspersed blood vessels showing thickened walls with fibrinoid deposits in walls, lined by plump endothelial cells. No granulomas were seen.
Skin lesions over back and neck were erythematous and macular, suggestive of Disseminated Lupus erythematosus and patient was advised to start fluticasone ointment. As ANA and Anti-ds DNA were positive, she was diagnosed as SLE with Autoimmune pancreatitis. Even though, steroid pulse therapy was indicated, it could not be initiated because the patient was in probable sepsis as procalcitonin was positive and multiorgan failure was there. Hence, antibiotics were changed from ceftriaxone to injection meropenem. Renal function tests were deranged with high creatinine and oliguria. The patient developed respiratory distress and severe hypoxemia. After which patient was intubated in view of hypotension, inotropes were started. The patient got cardiac arrest and immediately CPR was started according to ACLS guidelines. But the patient could not be revived.
Case 2
A 27-year-old female presented to the Department of Medicine with complaints of severe abdominal pain for 10 days and vomiting for one week. Abdominal pain was insidious, diffuse, colicky type without any radiation. The pain was aggravated by eating. Vomiting was non-bilious, non-projectile, contained food particles and not associated with haematemesis. No history of fever.
On physical examination, vitals were within normal limits, abdomen was soft, severe tenderness was present in epigastric region with guarding. No organomegaly and free fluid in the abdomen. Other systemic examinations such as of the central nervous system, cardiovascular system, and respiratory system were found to be normal.
Laboratory investigations are shown in [Table/Fig-1].
ANA global showed nucleus granular (+++) and cytoplasm granular (+++) on HEP-2 Cells. Antinuclear antibody profile was strong positive for nRNP/Sm (+++), sm (+++) and Rib P-Protein (++).
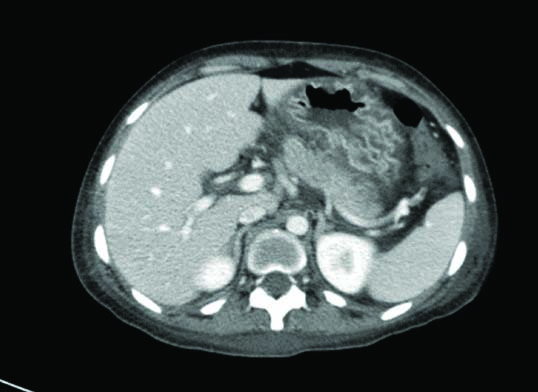
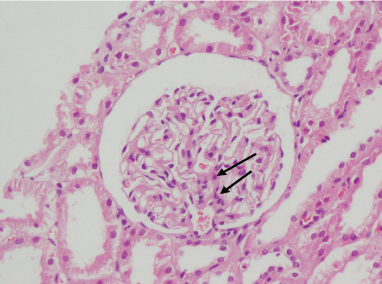
She was evaluated for abdominal pain and pancreatitis, upper and lower gastrointestinal scopy was done which showed gastritis and colitis, respectively. Ultrasonography was suggestive of bilateral moderate-gross pleural effusion and mild-moderate ascites. Computed tomography was suggestive of pancreatitis as shown in [Table/Fig-2]. Punch biopsy of skin from the forearm was suggestive of connective tissue disorder including SLE and vasculitis. A gastric biopsy was suggestive of chronic nonspecific gastritis. Biopsy was done from ileum, colon and rectum to rule out Infective serositis with colitis but no features of infective colitis were seen in the section studied. On renal biopsy-primary diagnosis was Lupus Nephritis and pattern of injury was focal proliferative glomerulonephritis as shown in [Table/Fig-3].
Computed tomography image of the patient indicated bulky pancreas (←).
Kindly biopsy of the patient indicated class III lupus nephritis segmental endocapllary proliferation along with increased mesangial cellularity is seen (←).
The patient was started on pulse steroid therapy. She was started on mycophenolate mofetil 500 mg thrice a day, steroids were given for a period of six weeks and later on tapered. After starting steroids, the patient developed psychosis, which was managed with psychiatric consultation and anti-psychotics. Pleural effusion and ascitic fluid were tapped, fluid was transudative. Enalapril (anti-hypertensive) was started in a dose of 5 mg twice a day for proteinuria. Hydroxychloroquine 200 mg twice a day was started after ophthalmic consultation. After three months, steroids were tapered and stopped. During follow-up, her proteinuria was negative, red cell cast became negative, urine was normal, ESR was normalised and the patient became asymptomatic. As behavioral abnormality related to SLE improved, so anti-psychotics were stopped. Then, her condition improved gradually over a period of 2-3 months.
Case 3
A 23-year-old female presented to the Department of Medicine with complaints of fever for 10-15 days and abdomen pain for two days.
On physical examination, vitals were within normal limits. The patient had jaundice and severe anaemia (Haemoglobin-7 g/dL). Systemic examination showed patient to have oral ulcers, erythematous papules, rash on face. The abdomen was soft and diffuse tenderness was present. Other systemic examination such as of the central nervous system, cardiovascular system, and respiratory system were found to be normal.
Laboratory investigations are shown in [Table/Fig-1].
ANA global showed nucleus granular (+++) and homogenous (+++) and cytoplasm fine granular (+++) on HEP-2 cells. Antinuclear antibody profile was strong positive for nRNP/Sm (+++), sm (+++), nucleosomes (+++) and histones (+++).
The patient had recurrent oral ulcers and joint pain, The erythematous rash was present and ANA was positive. Based on these, clinical diagnosis of SLE was established and was put on methylprednisolone and started with intravenous, ceftriaxone, intravenous fluids. Ultrasonography of abdomen was suggestive of the bulky pancreas. Patient developed hypotension and urine output was decreased. Nephrology consultation was taken and she was started on inotropes. The patient developed tachycardia with heart rate >250 beats/minute. In view of decreased oxygen saturation, she was intubated. She developed cardiac arrest and CPR was initiated as per ACLS protocols. Patient could not be revived.
Discussion
Systemic lupus erythematosus presenting with acute pancreatitis as an initial complaint is a rare entity. Diagnosing this condition is in itself a big challenge as clinicians have to rule out other possible aetiologies such as gallstone induced obstruction of pancreatic duct and alcohol-induced pancreatic toxicity. SLE is a multisystem disease, which involves the gastrointestinal system in about 50% of patients [1,2]. Pancreatitis is a rare complication of SLE. Only 99 cases of SLE pancreatitis had been documented in the literature and out of these only 10 cases had reported pancreatitis as an initial presentation of SLE [3,4].
SLE pancreatitis can occur as the generalised flare or during disease quiescence. Pathophysiology of SLE related pancreatitis is thought to be multifactorial and exact mechanism is not yet known. There are certain risk factors associated with SLE related pancreatitis- hypertriglyceridemia, recent viral infection, psychosis, and drug toxicity are the important ones [5]. Complement activation and autoimmune reactions, viral infections, vasculitis, intimal thickening, proliferation and immune complex deposition may play a role in the underlying mechanism of the disease [6]. Autoantibody production along with abnormal cellular immune response may lead to inflammation of parenchyma [7]. The increase in the numbers of cases of pancreatitis as an initial presentation of SLE supported that SLE is the underlying aetiologic factor [6].
Diagnosis of SLE pancreatitis depends on clinical features, laboratory and CT findings. In present cases, acute pancreatitis was diagnosed based on clinical symptoms and laboratory findings (that is remarkable elevated amylase and lipase enzymes). Lupus nephritis was confirmed by ANA positivity and positive anti-ds DNA serum titers in addition to renal biopsy.
Anti-ds DNA antibodies are highly diagnostic of SLE however, their absence doesn’t rule out SLE [8]. In case 2, anti-ds DNA was negative but the diagnosis of SLE was confirmed by kidney biopsy. A study by Fabrizio C et al., showed that anti-ds DNA antibodies are absent in SLE cases with serositis [9].
It is difficult to treat SLE pancreatitis with steroids because of the known toxic effects of steroids but they can make remarkable improve in the prognosis of such patients due to their immunosuppressive effects [10].
In case 1, we couldn’t start the steroids. Initially patient had features of sepsis and pro-calcitonin was positive (0.9375), in view of sepsis and deranged renal function test, steroid therapy was deciphered. Thus, patient condition deteriorated and she succumbed to illness.
In case 2, the patient didn’t have kidney injury but had subnephrotic proteinuria and was not requiring dialysis. Steroids were started in consultation with gastroenterologist and nephrologist early in the course of illness. The patient developed psychosis after initiation of steroids but could have been due to SLE. On continuation of steroids, psychosis and pain abdomen subsided. Gradually over the period of time proteinuria subsided.
In case 3, patient was very sick at the time of admission and expired within 24 hours. The diagnosis of SLE with pancreatitis was done only after receiving the laboratory reports.
Conclusion
To conclude, SLE presenting with pancreatitis is a severe form of SLE which is rarely seen in clinical practice. Here out of three cases, two ended up with mortality and one survived with steroid therapy. Early diagnosis and timely initiation of steroid pulse therapy may improve the outcome in SLE patients presenting with pancreatitis.
Steroid therapy in acute pancreatitis of other aetiology is hazardous. If it is SLE related pancreatitis, after ruling out other causes of pancreatitis, the steroid is advised to be started early for better outcome of the patient.
[1]. Reynolds JC, Inman RD, Kimberly RP, Chuong JH, Kovacs JE, Walsh MB, Acute pancreatitis in systemic lupus erythematosus: report of twenty cases and a review of the literatureMedicine 1982 61(1):25-32.10.1097/00005792-198201000-000036173564 [Google Scholar] [CrossRef] [PubMed]
[2]. Hiraishi H, Konishi T, Ota SI, Shimada T, Terano A, Sugimoto T, Massive gastrointestinal hemorrhage in systemic lupus erythematosus: successful treatment with corticosteroid pulse therapyThe American Journal of Gastroenterology 1999 94(11):334910.1111/j.1572-0241.1999.01551.x10566742 [Google Scholar] [CrossRef] [PubMed]
[3]. Wang F, Wang NS, Zhao BH, Tang LQ, Acute pancreatitis as an initial symptom of systemic lupus erythematosus: a case report and review of the literatureWorld Journal of Gastroenterology 2005 11(30):476610.3748/wjg.v11.i30.476616094728 [Google Scholar] [CrossRef] [PubMed]
[4]. Jia Y, Ortiz A, Mccallum R, Salameh H, Serrato P, Acute pancreatitis as the initial presentation of systematic lupus erythematosusCase Reports in Gastrointestinal Medicine 2014 2014:57149310.1155/2014/57149325197582 [Google Scholar] [CrossRef] [PubMed]
[5]. Makol A, Petri M, Pancreatitis in systemic lupus erythematosus: frequency and associated factors-a review of the Hopkins Lupus CohortThe Journal of Rheumatology 2010 37(2):341-45.10.3899/jrheum.09082920032096 [Google Scholar] [CrossRef] [PubMed]
[6]. Duncan HV, Achara G, A rare initial manifestation of systemic lupus erythematosus-acute pancreatitis: case report and review of the literatureThe Journal of the American Board of Family Practice 2003 16(4):334-38.10.3122/jabfm.16.4.334 [Google Scholar] [CrossRef]
[7]. Tian XP, Zhang X, Gastrointestinal involvement in systemic lupus erythematosus: insight into pathogenesis, diagnosis and treatmentWorld Journal of Gastroenterology 2010 16(24):297110.3748/wjg.v16.i24.297120572299 [Google Scholar] [CrossRef] [PubMed]
[8]. Kavanaugh A, Tomar R, Reveille J, Solomon DH, Homburger HA, Guidelines for clinical use of the antinuclear antibody test and tests for specific autoantibodies to nuclear antigensArchives of Pathology & Laboratory Medicine 2000 124(1):71-81. [Google Scholar]
[9]. Fabrizio C, Fulvia C, Carlo P, Laura M, Elisa M, Francesca M, Systemic lupus erythematosus with and without anti-dsDNA antibodies: analysis from a large monocentric cohortMediators of Inflammation 2015 2015:32807810.1155/2015/32807826063969 [Google Scholar] [CrossRef] [PubMed]
[10]. Breuer GS, Baer A, Dahan D, Nesher G, Lupus-associated pancreatitisAutoimmunity Reviews 2006 5(5):314-18.10.1016/j.autrev.2005.11.00416782555 [Google Scholar] [CrossRef] [PubMed]