The isolation of NTM from clinical specimens is increasing among both immunocompromised and immunocompetent and also in the elderly patients in the last years [1-3]. NTM are typically environmental microorganisms and certain species of them may cause opportunistic diseases in human with various predisposing conditions of host-related factors. Pulmonary infections related to NTM are the most frequent disease type of these bacteria, although involving other parts of the body has also been reported. Among immunocompromised patients; the rate of reported infections like in the lymph nodes, soft tissues and cutis, catheter and bone-joints have been increased [4]. The genus Mycobacterium contains more than 150 species. Detection of mycobacteria at species level is necessary and itself provides useful information on epidemiology and successful options for treatment [5].
Mycobacteriosis in fish is a chronic progressive disease. Some mycobacterial species that normally cause mycobacteriosis in ornamental fish are Mycobacterium marinum (M. marinum), Mycobacterium cheloni (M. cheloni), and Mycobacterium fortuitum (M. fortuitum), and several other species of mycobacteria have also been identified to be associated with this disease [6]. Diagnosis of this disease in aquarium fish is usually done by histopathology, culture, determination of bacterial growth characteristics, pigment type, colony morphology, and biochemical tests. M. marinum is an opportunistic pathogen causing several human infections reported worldwide including Iran [7,8]. Non-tuberculosis mycobacteria such as M. marinum can be transmitted to human from contaminated ornamental fish or contaminated environment (contaminated water) during contact with the aquarium while cleaning or touching the fish through cuts or scratches on the skin [9-12]. M. cheloni and M. fortuitum are aggressive species growing fast and distributed widely in the environment (soil and water), which are the common cause of nosocomial infections that usually cause superficial lesions, possibly pulmonary disease, and primary lymphadenopathy [13]. Isolation of rapidly growing mycobacteria were frequently reported in pulmonary infections from Taiwan, China, and Singapore [14,15].
Due to the zoonotic character of fish mycobacteriosis, increasing opportunistic infections via NTM in the elderly and immunocompromised patients and on the other hand existence of difficulties in long-term treatment of NTM infections, the aim of this study was to isolate and identify the species of non-tuberculous mycobacteria from aquarium fish samples. Detection of drug resistance of isolates was done to isoniazid, ethambutol, rifampin, Streptomycin, kanamycin, ciprofloxacin, and amikacin.
Materials and Methods
Fish samples: Fifty-three aquarium fish of eight different species including eight Carassius auratus, four Xiphophorus maculatus, four Microgeophagus altispinosus, four Andinoacara rivulatus, three Heros severus, 10 Puntius conchonius, 12 Poecilia latipinna, and eight Astronatus ocellatus were randomly selected from different aquarium stores in Tabriz. In some aquarium fish, there were signs of illness such as lethargy, scale loss and skin lesions, and some of the samples had no clinical signs and appeared to be healthy. The samples were immediately transferred to the Tuberculosis and Lung Disease Research Center of Tabriz University of Medical Sciences for laboratory work.
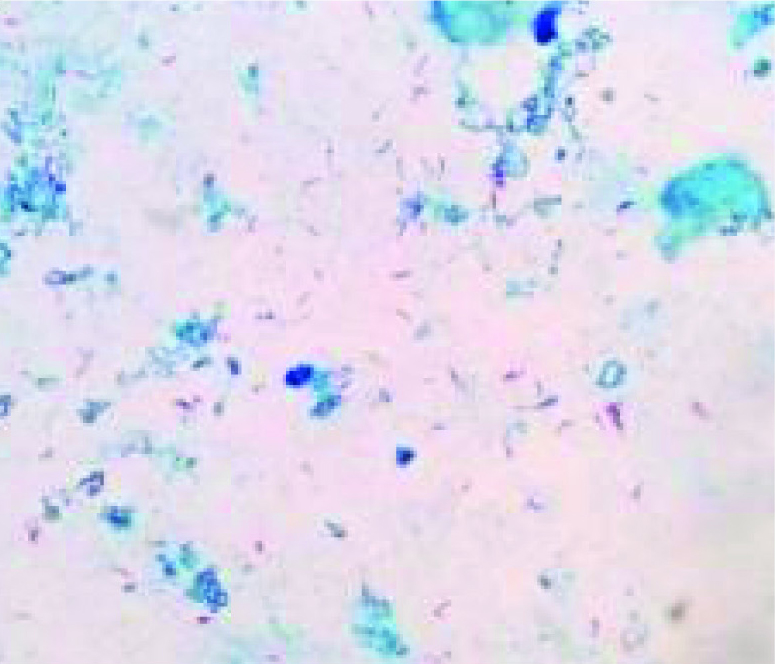
Laboratory examination: The internal organs including liver, spleen, kidney, intestines, and different organs of the fish were separated by sterile scissors, scraped off in small sizes, and homogenized in a vortex machine for three minutes in a sterile falcon tube containing distilled water and sterile glass pearl. Then, the sample was filtered by transferring them from the current containers into the new falcon tubes by inserting the sterilized gas into the tubes, and used them for Ziehl-Neelsen staining (ZN staining) to see AFB. In each of the slides prepared, one hundred fields of vision were examined with optical microscope with magnification of 1000.
For culture examination, the homogenized samples of fish organs were also centrifuged and decontaminated by the Petroff method [16]. One volume of the sample was poured into two volumes of Sodium Hydroxide 1N solution in a falcon tube and soda 1N was added. After the samples passed through digestion and decontamination, they were placed at a room temperature for half an hour in a shaking machine to homogenize and then centrifuged at a speed of 3000 rpm for half an hour. In the stage after centrifugation of the samples, the supernatants were discarded under a ventilation hood and by adding a drop of phenolphthalein 0.01% as a colour reagent and with the help of 1N hydrochloric acid neutralizing the pH of the samples was performed (pH 6/8). Then, under the hood, 20 μl of the sediment was inoculated in Lowenstein-Jensen Culture media (each sample in two culture media) and incubated for eight weeks at 30°C and 37°C [17]. Culture media were examined daily for four weeks and then once a week for three months to observe growth and determine the growth rate of mycobacteria. Samples that were positive for development but their cultivation remained negative until the end of this period were incubated for another four weeks (for a total of 12 weeks) [17,18].
Identification of isolated mycobacterium species: Identification of isolated mycobacterium species was done using phenotypic characteristics (growth rate, growth at different temperatures, colony morphology, and pigment production test) and biochemical tests {niacin and urease production, heat resistant catalase test (68°C), hydrolysis between 80, 3-day arylsulfatase test, and nitrate reduction test} [18].
Evaluation of drug resistance of isolates: Drug resistance of isolated strains was studied proportionally. For this purpose, first, a dilation equal to half McFarland was prepared from suspension of isolated mycobacterium species and then a concentration of 0.01 was prepared from that, and 0.2 mL of diluted suspension was inoculated to Lowenstein-Jensen Culture media containing isoniazid 0.2 μg/mL, ethambutol 2 μg/mL, rifampin 40 μg/mL, streptomycin 4 μg/mL, kanamycin 20 μg/mL, ciprofloxacin 4 μg/mL, and amikacin 20 μg/mL antibiotics, and Lowenstein-Jensen Culture media without antibiotics (as control) and incubated for six weeks at 37°C. If the bacterial growth rate (the number of colonies) in antibiotic-containing media was less than 1% in comparison with the control culture medium, the strain was considered susceptible; and if the growth rate was equal to or greater than 1% relative to the control medium, it was considered as a resistant strain. The standard Mycobacterium tuberculosis strains H37Rv, which was sensitive to all the drugs used in this test, was used as control strain [19-21].
Ethical Approval
The experimental protocol was reviewed and approved by Ethical Review Committee, Islamic Azad University of Karaj and conducted accordıng to Institutional Animal Care and Use Committee of Iran (IACUC no.= 140426/ February 12, 2016).
Results
Among fifty-three ZN-stained specimens, seven (13.2%) gave positive direct microscopic results for mycobacteria [Table/Fig-1].
Using the bacterial culture method, out of 53 samples, Mycobacterium spp.colonies was observed in 15 (28.3%) Lowenstein-Jensen agar tubes [Table/Fig-2].
Mycobacterium sp. colonies on Lowenstein-Jensen agar.

Identification of different species of mycobacterium from 15 isolates obtained by culture based on phenotypic characteristics and biochemical tests was as follows [Table/Fig-3,4]: M. fortuitum, 6 cases; M. marinum, 3 cases; M. smegmatis, 3 cases; M. terrea, 1 case; M. flavescens, 1 case; and M. asiaticum, 1 case.
Phenotype characteristics and biochemical tests
| Growth at temperatures30°C-37°C | Colonymorphology | Pigmentproduction | Growth rate | Biochemical testes | Mycobacterium spp. |
|---|
| Niacin | Nitrate Reduction | Catalase heatstable 68°C | Tween 80 Hydrolysis | Arylsulfatase(3days) | Urease |
|---|
| + | + | S | N | Growth < 7 days | - | + | + | - | + | + | M. fortuitum |
| + | - | S | P | Growth > 7 days | - | - | - | + | - | + | M. marinum |
| + | + | S | N | Growth < 7 days | | + | + | + | - | | M. smegmatis |
| + | + | S | N | Growth > 7 days | - | + | + | + | - | - | M. terrae |
| + | + | S | Sc | Growth < 7 days | - | + | + | + | - | + | M. flavescens |
| + | + | S | P | Growth > 7 days | - | - | + | + | - | - | M. asiaticum |
+: the isolate was positive for the test; -: a negative reaction for the test.
P= Photochromogenic; Sc= Scotochromogenic; N= Non-chromogenic; R= Rough; S= smooth
Mycobacterial species isolated from samples
| Aquarium fish species | Samples | Contaminatedcases | Isolated mycobacterial species |
|---|
| Mfl | Ma | Mm | Mfo | Ms | Mt |
|---|
| Poecilia latipinna | 12 | 5 | - | + | + | ++ | + | - |
| Xiphophorus maculatus | 4 | 0 | - | - | - | - | - | - |
| Carassius auratus | 8 | 3 | - | - | + | + | + | - |
| Microgeophagus altispinosus | 4 | 0 | - | - | - | - | - | - |
| Andinoacara rivulatus | 3 | 0 | - | - | - | - | - | - |
| Puntius conchonius | 10 | 4 | - | - | + | ++ | + | - |
| Heros severus | 4 | 0 | - | - | - | - | - | - |
| Astronatus ocellatus | 8 | 3 | + | - | - | + | - | + |
| Total | 53 | 15 | 1 | 1 | 3 | 6 | 3 | 1 |
Mfl = M. flavescens; Ma = M. asiaticum;Mm = M. marinum;
Mfo = M. fortuitum;Ms = M. smegmatis; Mt = M. terrae
In drug sensitivity study, from among the strains isolated (14 cases) 93.33% were resistant to streptomycin (12 cases) 80% to isoniazid, (12 cases) 80% to rifampin, (10 cases) 66.66% to etambutol, (9 cases) 60% to kanamycin, (6 cases) 40% to amikacin, and (3 cases) 20% to ciprofloxacin. The results indicated that streptomycin had the highest drug resistance and the lowest drug resistance was related to ciprofloxacin.
Discussion
In direct microscopic examination using ZN staining method, 13.2% of AFB were identified, and in the bacterial culture (28.3%) AFB were isolated. Although direct microscopic sensitivity is less than culture experiment, it may provide valuable information, especially when bacterial culture fails probably due to the destruction of mycobacterium species by the host defense system or very low levels of living bacteria in the tissue [6].
Mycobacteria have a global distribution and widely swarm in aquatic environments [13,22,23]. Mycobacteriosis is one of the common infections in ornamental fish reported in more than 150 species [24]. When the fish is in infected with mycobacteria, it usually does not behave differently from non-infectious fish. We only suspected their being infected when their mobility weakens, the colour of the skin of the fish becomes faint, and other clinical symptoms such as the inflammation of the skin, skin lesions or wounds, exophthalmos and so on occur [25]. As various species of non-TB mycobacterium can potentially be transmitted to humans from fish, water, and their living environmental, such as aquariums and reservoirs and fish ponds and cause skin infections [9,11,13,26,27], the people working in aquarium stores and anyone who is somehow associated with ornamental fish should take precautionary and preventive steps, even when in contact with seemingly healthy fish. Drug therapy is not recommended for fish and has a limited value for the disease as treatment does not remove mycobacteria from the populations of infected fish [24].
Considering the development of the aquaculture industry and the increase in the importance of domestic ornamental fish, it is necessary to provide fast and accurate tools for the identification of pathogens and their treatment. Moreover, it is important for veterinarians and aquaculture specialists to be aware of clinical signs of the disease transmissible between fish and humans and ways to minimize the risk of exposure to these organisms. Among important feature of many of the mycobacterial species causing this disease are their opportunistic character and the disease being often associated with people who have a weakened immune system. Most infections occur among people having aquariums at home, or breeders and fishermen and may be a business risk for specific people at risk for this infection [24,28]. When washing of an aquarium by immunosuppressed patients, safety precautions such as wearing gloves, shaving hands and even wearing a mask and the adequate chlorination of tanks should be carefully considered [24].
Increase in reports of infections caused by opportunistic pathogens, including non-TB mycobacteria in the elderly or immunocompromised patients on the one hand, and very difficult treatment and the need for long-term treatment for these infections on the other have made this a serious issue in relation to the general health of society [3,23,29].
Mycobacterium flavescens has been isolated from pulmonary diseases, osteomyelitis, keratitis, disseminated post-injection infection and gluteal abscess [13]. Mycobacterium smegmatis has been known as the causative agent of skin and soft tissue infection, pulmonary disease, endocarditis, osteomyelitis, lymphadenitis, arthritis and disseminated infections [30,31]. M. asiaticum has been isolated from progressive pulmonary disease and extrapulmonary disease in human such as flexor tenosynovitis, keratitis and olecranon bursitis [32].
In humans, M. marinum could be cause of nodular and granulomatous inflammation of the tendon sheaths of hands and fingers, subcutaneous tissues, skin and is referred to as ‘fish tank granuloma’, ‘swimming pool granuloma’, ‘fish fanciers disease’, ‘fish handlers’, or ‘fish TB’ [24,33,34]. Mycobacterium fortuitum has been diagnosed in post-injection abscess disease, sternal wound infection, traumatic osteomyelitis, mastitis, cellulitis and peritonitis [13].
The results of studying the samples showed that M. marinum and M. fortuitum were isolated more than other species (9 out of 15). Many studies have shown that these species commonly cause mycobacteriosis in ornamental fish. Three species of M. fortuitum, Mycobacterium gordonia, and M. terrea have been reported in relation to fish mycobacteriosis in the Republic of Kazakhstan [35]. Many of the infections caused by M. marinum in human have a slow and spontaneous recovery in 1 to 6 years. Small lesions may heal themselves, but in other cases, multiple antibiotic treatments are required for several months [29,36]. Antibiotic treatment may prevent the progression of deep-seated infection, but the bacteria are highly resistant to the treatment [24,27]. Antibiotic therapy for humans include isoniazid, rifampin, perazinamide, ethambutol, streptomycin, kanamycin, ciprofloxacin, azithromycin and some quinolones. Infection responds to appropriate antibiotic therapy slowly and depending on the extent and severity of infection, the course of antibiotic treatment may vary from 2 weeks to more than 18 months [13,21,29].
Normally, the infection is not very aggressive and responds to treatment, although months of treatment may be necessary. Sometimes, the infection can spread to deeper tissues such as the bone that hardly responds to treatment [4,21]. Deep infections usually require both antibiotic and surgical treatments. Removal of necrotic tissue including joint synovial, joint tenosinovial or joint removal is essential. Moreover, amputation to control the infection despite proper antibiotic treatment and multiple removal of necrotic tissue may be required [21]. Considering the use of the drugs mentioned in the treatment and the results of investigating the susceptibility and drug resistance of isolated mycobacterium species, streptomycin had the highest drug resistance with 93.33% and the lowest drug resistance was related to amikacin (40%) and ciprofloxacin (20%). Thus, ciprofloxacin and amikacin can be used as selective therapies for treatment, but this is a serious challenge to the treatment of diseases caused by NTM species. Probably one of the factors contributing to high resistance to streptomycin is the use of this drug in the treatment of other infectious diseases [21,37].
Limitation
The limitation was low number of viable mycobacteria in the tissue. It may be caused by killing of mycobacteria through host defense mechanisms or destruction of the mycobacteria during the preparation of the samples. This could lead to negative cultivation results. Additionally, biochemical examination is a time consuming method, the results are often difficult to interpret and variations among strains may occur. The reason for the difficult interpretation of the biochemical profile may lie in mixed mycobacterial cultures due to contamination with other bacteria among some samples.
Conclusion
In recent years, mycobacterial infections in aquarium fish have received much attention, which is due to the increasing importance of aquariums in the world and more attention to public health. This study isolated some bacteria from aquarium fish such as M. marinum, M. fortuitum, M. smegmatis, and M. flavescens known as pathogens from fish and humans. It was also indicated that isolated strains were resistant to most of the drugs used in the treatment. Given the zoonosis of the disease, the difficulty of treatment, and the need for a long-term treatment period, those who are involved with aquariums and aquaculture equipment, or even those who keep ornamental fish at home for entertainment, especially the people with immunodeficiency. More considerations are needed to prevent or reduce the transmission of disease to humans.
+: the isolate was positive for the test; -: a negative reaction for the test.
P= Photochromogenic; Sc= Scotochromogenic; N= Non-chromogenic; R= Rough; S= smooth
Mfl = M. flavescens; Ma = M. asiaticum;Mm = M. marinum;
Mfo = M. fortuitum;Ms = M. smegmatis; Mt = M. terrae